Abstract
Purpose
To report a series of five cases with retinitis following episodes of febrile illness, its evaluation, management and outcome.
Method
Retrospective, consecutive case series of five patients presenting with acute retinitis, following a febrile illness.
Results
The retinal lesions had a sudden onset with rapid evolution, preceded by a febrile episode within one month of presentation, in all cases. Extensive serology and PCR testing were non-contributory toward identifying the etiology and guiding therapy. Systemic corticosteroid therapy was effective in hastening the resolution of lesions.
Conclusion
Post-fever retinitis appears to be a distinct clinical form of acute hemorrhagic non-necrotizing retinitis without a uniformly identifiable cause, and some evidence pointing toward a para-infectious etiology secondary to flu-like illnesses. With an unusual morphological presentation and annual seasonal patterns in the endemic areas, it is important to differentiate this entity, from other forms of infectious retinitis, before initiating corticosteroid therapy.
Similar content being viewed by others
Introduction
Retinitis forms a subset of posterior uveitis according to the International Uveitis Study Group [1] and Standardization of Uveitis Nomenclature working group [2] classification. In many cases, history and characteristic clinical appearance can guide toward a correct diagnosis and initiation of treatment. While in other cases, additional serological testing or polymerase chain reaction (PCR) test is needed to establish the diagnosis. It is important to rule out infectious etiology in cases of acute retinitis before initiating corticosteroid or immunosuppressive therapy.
Retinitis characterized by multifocal retinal infiltrates, cotton-wool spots and retinal hemorrhages—following a febrile illness has previously been reported from southern part of India [3, 4]. Despite similar clinical presentation, the underlying etiologies reported in these studies were variable, while a majority of these cases were idiopathic in nature. Additionally, India being a tropical country, these cases specifically presented during cooler months of the year, with an annual recurrence pattern [5, 6].
India is a diverse country and our case series highlights a morphologically distinct form of non-necrotizing acute retinitis, which is similar in presentation to the previous cases reported in southern India, however in a different geographical area; where it has not been reported earlier. We describe the clinical presentation, morphology of lesions, clinical course, treatment and outcome in five cases of acute non-necrotizing retinitis with a common history of febrile illness, prior to presentation and relevant review of literature.
Material and methods
This study is a single center, observational case series carried out at a tertiary referral eye institute of national importance in central India. Five consecutive cases of acute retinitis having a common previous history of febrile illness, were included between October 2019 and January 2020, before COVID-19 was declared a pandemic in India. All cases had a documented history of febrile illness with no specific etiology of fever documented in records. All patients underwent detailed ophthalmological examination that included best-corrected visual acuity (BCVA), intraocular pressure (IOP), anterior and posterior segment evaluation, fundus fluorescein angiography, fundus photography, and optical coherence tomography. Investigations included complete hemogram, erythrocyte sedimentation rate, venereal disease research laboratory tests (VDRL), human immunodeficiency virus (HIV) ELISA, Mantoux test, serum angiotensin-converting enzyme (ACE) test, and radiograph chest. Thorough systemic evaluation of all the patients by infectious disease specialist was performed, along with detailed laboratory work-up, including malaria parasite, Widal test, chikungunya IgG/IgM, Dengue IgG/IgM, Toxoplasma immunoglobulin IgG/IgM, and Weil-Felix test. Other investigations like polymerase chain reaction for herpes simplex virus and varicella-zoster virus (HSV/HZV) were carried out as necessary. Patient’s referral notes were reviewed for details of fever, history of travel and treatment received for the same; ocular intervention, systemic investigations, previous laboratory tests or microbiological evidence and any other relevant information was documented. All patients received systemic corticosteroids for retinitis, after having undergone a complete evaluation by internist. Details of the type of steroids, dose and duration of therapy were noted. Treatment and procedure details of patients who had been referred from outside were also recorded.
All patients belonged to central India and had not travelled out of the geographical area under study, within the last three months. The research adhered to the tenets of the Declaration of Helsinki.
Results
Study subjects
Five patients between the age of 23 and 46 years—otherwise healthy and immunocompetent—who presented with acute retinitis, following an episode of fever, were included. Three of these patients had bilateral involvement, while the retinal involvement was unilateral in the remaining two patients. Average duration between the febrile episode and onset of ocular symptoms, varied from one and five weeks. None of the patients showed evidence of anterior segment inflammation or raised IOP. In all five cases, the systemic examination was unremarkable, and the thorough laboratory workup was inconclusive (Table 1). Four out of five patients received intravenous-pulsed corticosteroid therapy; while one was managed using oral corticosteroids, along with antiviral therapy. All the patients were followed up for at least six months. None of the patients demonstrated any evidence of neovascular complications or recurrence of retinitis lesions, in the follow-up period (Table 1).
Case findings
Case 1
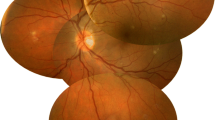
A 46-year-old Indian Asian male presented with a complaint of painless, rapidly progressive diminution of vision in both eyes (OU) for one week. Patient had an episode of fever one month ago that lasted for four days. Physical examination was unremarkable and therefore, the fever was diagnosed as seasonal flu-like illness and treated symptomatically. At presentation, BCVA was 20/400 and 20/500 and IOP was 10 and 12 mm of Hg in right eye (OD) and left eye (OS), respectively. Anterior segment was quiet, and pupillary reflexes were normal. Posterior segment examination revealed mild vitritis with 1 + vitreous haze in both eyes. Optic disc and major vascular arcades appeared normal in the right eye; but there was loss of foveal-reflex and presence of superficial and intraretinal hemorrhages at the macula (Fig. 1a). Infero-temporal to macula a flat whitish lesion with irregular borders and associated hemorrhage was noted (Fig. 1a). Optic disc appeared hyperemic with fullness of vessels. Single creamish flat lesion, with regular borders was present temporal to the optic disc (Fig. 1b).
(At Presentation) Fundus picture (FP) shows active retinitis lesions in right (a) and left (b) eye. (Blue arrow-superficial and intraretinal hemorrhages) Fundus fluorescein angiography (FFA) of OD (arterio-venous phase) shows increasing hyperfluorescence with start of leakage (Yellow arrow-blocked fluorescence) (c) and late leakage with disc involvement in OS (late arteriovenous phase) (d). Optical coherence tomography (OCT) scan shows disturbed foveal contour with subfoveal deposits in OD (e) and peripapillary nerve fiber layer edema, intraretinal edema and sub foveal serous exudation in OS (f). OS appears more active compared to OD. The latter shows features of resolving lesions. (At 6 months follow-up) FP Both eyes (g and h) show fully resolved lesions
FFA (OD) showed blocked fluorescence in areas of retinal hemorrhages. The lesion appeared uniformly hypofluorescent in early phase and became increasingly hyperfluorescent in subsequent frames, followed by late leakage (Fig. 1c). Findings suggestive of a full thickness retinitis lesion in the stage of central clearing. FFA (OS) showed increasing hyperfluorescence that migrated towards the center of the lesion, ultimately covering the entire lesion in late phase, suggestive of an active full-thickness retinitis lesion (Fig. 1d). In addition, the left eye had disc hyperfluorescence (Fig. 1d). OCT of both eyes, revealed full-thickness hyper-reflectivity with effacement of retinal layers (Fig. 1e, f). Foveal contour was distorted in OD, due to the presence of resolving subretinal exudation and possible subfoveal fibrosis (Fig. 1e). In OS, presence of subfoveal serous retinal detachment and intraretinal edema was noted, adjacent to the active lesion (Fig. 1f).
Based on a non-specific history and non-contributory laboratory findings—a specific etiological diagnosis could not be established. Since the retinitis involved the macular region in both eyes with optic nerve and papillomacular bundle, affected in OS—the patient was started on intravenous pulsed corticosteroid therapy to control inflammation, followed by a tapered oral regimen. Lesions in OD resolved in three weeks, whereas OS showed resolution of original lesion and disc hyperemia on one hand, but developed a fresh extension of the lesion at its superior border on the other. Significant improvement in visual acuity was noticed. At two months, OD showed retinal atrophy without significant pigmentary changes, while OS revealed resolution of retinitis, marked by decreasing infiltrates and exudation. At six months follow-up, the right eye was stable, while the left showed diffuse thinning of retina in the area of papillomacular bundle (Fig. 1g, h). Visual acuity at the end of six months was 20/40 in OD and 20/100 in OS.
At one year, no pigmentary changes or development of neovascular membranes were observed. This pattern of healing corroborated our initial clinical impression, that the lesion was limited primarily to the retina and spared the underlying retinal pigment epithelium and choriocapillaris. During the entire follow-up period, the patient did not develop any recurrent lesions and maintained a stable visual acuity.
Case 2
A 23-year-old Indian female presented with diminution of vision in left eye for 10 days. Patient gave a history of fever one month ago. Presenting visual acuity was 20/20 OD and 20/100 OS and IOP was 14 mm Hg in both eyes. Pupillary reflexes were normal. The Anterior Segment was quiet. Fundus examination of OS showed creamish lesion below the macula with surrounding exudation (Fig. 2a). In OD a faint whitish lesion was noted temporal to macula. Optic disc was normal and mild vitritis was present in both eyes. On FFA the lesion was hypo-fluorescent in the early phase with progressive hyper-fluorescence in late frames in both eyes (Fig. 2b). OCT showed full thickness hyper-reflectivity and effacement of affected retina, and confirmed the presence of subretinal fluid with macular involvement in OS.
(At presentation) FP OS (a) shows active retinitis with exudative fluid. FFA late phase showing hyperfluorescence (b). (After 1 month of steroid treatment) OD fundus picture shows appearance of fresh multiple fulminant retinitis lesions with hemorrhages with subretinal fluid (c). (At 2 months after steroid and antiviral treatment) OS fundus picture shows resolution of early features with appearance of fresh peripapillary lesion (d). (At 6 months follow-up) with continued treatment, OS OCT picture; fovea (e) appears dry and thinned, however, with preserved outer layers. OD fundus picture (f) the retinitis looks mostly resolved
Patient recalled having a mild flu-like illness and responded to over-the-counter medications. We started her on oral corticosteroids—1 mg/kg body weight. After a month of treatment, visual acuity in OS returned to 20/40, accompanied by the resolution of retinitis patch and subretinal fluid (SRF). But in the OD, visual acuity deteriorated to 20/30 and a fulminant retinitis lesion associated with hemorrhages appeared along with subretinal fluid (Fig. 2c). Since the clinical picture was worsening, we undertook diagnostic vitreous surgery to perform PCR testing in order to rule out an infectious etiology, which could have been worsening following the administration of corticosteroids. PCR results for Herpes simplex virus, Varicella Zoster virus, Cytomegalovirus and Toxoplasma were negative. Despite negative results, the patient was started on antiviral therapy—Acyclovir 800 mg, five times a day, in view of progressive retinitis in OD.
Corticosteroids were withdrawn and antiviral therapy was continued. Notwithstanding, a fresh crop of lesions developed inferotemporal to macula in OD and in peripapillary area in OS (Fig. 2d). Therefore, a decision to reintroduce corticosteroids under antiviral cover was taken. At the end of 2 weeks, the lesions stabilized and one month after diagnostic vitrectomy—both eyes showed significant improvement. At 6 months, visual acuity had recovered to 20/30 in both eyes (Fig. 2e, f). Corticosteroids were tapered and stopped, while antiviral therapy was continued for 6 months.
Case 3
A 36-year-old Indian Asian male presented with diminution of vision in OD for six days with a history of fever two weeks ago. Previous records revealed flu-like upper respiratory tract symptoms with fever, that had fully resolved with treatment at a local facility, before reporting to us for visual complaints. Presenting visual acuity was 20/200 and 20/20 and IOP was 14 and 16 in OD and OS, respectively. Fundus examination OD revealed mild vitritis and creamy-white lesion adjacent to the optic disc and associated with retinal hemorrhages and submacular fluid (Fig. 3a). Fundus findings of the left eye were unremarkable. FFA (OD) was suggestive of active retinitis without associated vasculitis (Fig. 3b). OCT (OD) showed full-thickness hyper-reflectivity and effacement of affected retina, and confirmed the presence of SRF with macular involvement (Fig. 3c).
(At Presentation) FP OD (a) shows lesions close to the optic disc, retinal hemorrhages and serous detachment of macula. FFA–OD shows increasing hyperfluorescence in the late phase with pooling (b). OCT picture, OD (c) scan shows intraretinal edema and serous detachment of macula. (At 1 month follow-up) FP OD (d) shows near total resolution of the lesion with appearance of hard exudates. (At 6 months follow-up) OCT picture OD (e) shows normal foveal contour with mild thinning of macula and loss of ellipsoid zone (yellow arrow) in the subfoveal area
In view of the proximity of the lesion to the optic disc; patient was started on pulsed steroid therapy (1 g/day) followed by tapered oral corticosteroids (1 mg/kg). At one-month visual acuity (OD) recovered to 20/20p with significant clinical resolution (Fig. 3d) and foveal-contour had returned to normal on OCT. However, at six months follow-up, the vision had slightly dropped to 20/40 (OD) and OCT showed macular thinning and loss of ellipsoid zone in the sub-foveal area (Fig. 3e).
Case 4
A 40-year-old female presented with diminution of vision in both eyes for three weeks. There was a history of fever two months ago. Presenting visual acuity was 20/125 and 20/200 and IOP of 12 and 16 mm of Hg, in OD and OS, respectively. Fundus (OD) showed presence of creamy-white juxta-foveal lesion with SRF and superficial hemorrhages (Fig. 4a). Left eye showed multiple small creamy-white retinal lesions at the posterior pole, involving the macula with minimal SRF. There was presence of vitreous cells in both eyes.
(At Presentation) Fundus picture OD (a) shows active retinitis lesions with exudative maculopathy. FFA–OS (b) shows progressive hyperfluorescence with pooling of dye. OCT scan OD (c) shows exudative detachment, inner layer hyper-reflectivity and intraretinal edema. (At 1 month follow-up) fundus picture OS (d) shows significant resolution of lesion. (At 3 months follow-up) OCT scan OS (e) shows complete resolution of lesion with normal foveal contour and foveal thinning
FFA showed hypo-perfusion in the area of lesion in both eyes. Optic disc and retinal vessels showed staining. Late-phase showed increasing hyper-fluorescence and pooling of dye (Fig. 4b). OCT (OD) through macula showed hyper-reflectivity and effacement of the retinal layers along with SRF, intra-retinal edema and hard-exudates (Fig. 4c). OCT (OD) through lesion showed hyper-reflectivity of retinal layers, subretinal and intraretinal fluid and a large foveal cyst.
Erythrocyte sedimentation rate (ESR) was elevated (22 mm). Owing to bilateral macular involvement, the patient was started on pulsed corticosteroid therapy (1 g/day); followed by oral steroids (1 mg/kg) tapered weekly. At one month the lesions started to resolve in both the eyes. Visual acuity improved to 20/160 (OU) in one month. OCT showed restoration of foveal contour at three months; however, the onset of thinning was evident in OS (Fig. 4d, e). At one year the right eye had recovered fully, while OS developed foveal thinning; with visual acuity of 20/20 (OD) and to our surprise 20/40 (OS).
Case 5
A 28-year-old Indian Asian male presented with diminution of vision in OS for three weeks with a history of fever two months ago. Presenting visual acuity was 20/20 and 20/800 and IOP 16 mm Hg OU. Fundus examination of the left eye revealed, creamy-white lesion extending along upper-temporal vascular arcades (Fig. 5a). Mild vitritis, multiple hemorrhages with hard exudates and serous macular detachment was present in OS. Fundus examination of OD was unremarkable.
(At Presentation) fundus picture OS (a) shows active retinitis lesion with surrounding exudative serous retinal detachment. FFA OS (b) shows progressive hyper-fluorescence due to leakage. OCT scan OS (c) shows serous macular detachment. (At 4 months follow-up) OCT scan OS (d) shows restoration of foveal contour and (at 6 months follow-up) fundus picture OS (e) shows complete resolution of lesions
FFA (OS) showed features suggestive of active retinitis with retinal hemorrhages (Fig. 5b). Subsequent frames showed progressive hyper-fluorescence due to leakage and pooling of the dye in subretinal space. The optic disc also showed hyper-fluorescence. OCT (OS) showed full-thickness hyper-reflectivity and effacement of affected retina and confirmed the presence of SRF with macular involvement (Fig. 5c).
Patient was started on pulsed corticosteroid therapy (1 g/day) followed by oral corticosteroids (1 mg/kg) tapered weekly. With treatment, lesions began to resolve and OCT showed resorption of SRF and restoration of normal foveal contour (Fig. 5d). Patient gained 20/20 visual acuity in the left eye at four months, and maintained a stable clinical course at last follow-up after six months (Fig. 5e).
Discussion
This series highlights a unique presentation and clinical course of acute retinitis, the etiology of which remains elusive. It could be grouped as a subset of acute non-necrotizing retinitis, likely secondary to a para-infectious process and hence immune-mediated, therefore should be dealt with—distinct from—established forms of infectious/viral posterior uveitis. This is the first report of a series of such cases of acute retinitis from central India. The consistency of this clinical presentation, after subsidence of a febrile episode—and not concurrent with it; immunocompetent status of all the patients, and clinical resolution hastened by systemic corticosteroids—are some of the clinical clues, that point toward an immunological cause as against an infectious one. We also did not come across any recurrence of lesions after initial resolution and none of the cases in this series were found to have associated systemic vasculitis or autoimmune disease. The possibility of retinitis—resulting from an autoimmune trigger—following a viral flu-like episode; was considered to be a likely etiology.
The lesions were unifocal to multifocal in distribution and seemed to have a predilection for the peripapillary retina, often involving the macula—either direct involvement with retinitis or secondarily due to an exudative response—causing serous macular detachment. Optic nerve was frequently involved, depending on its proximity to the lesion and features of optic nerve inflammation were present in three out of five cases. The lesions were unilateral in two cases while three had bilateral involvement at presentation. IOP was normal at presentation and remained within normal limits until last follow-up. The time duration, from development of fever to the onset of ocular symptoms was—one week to five weeks. After starting steroid therapy, time required for complete resolution of lesions ranged from one to six months. Final visual acuity was better than during presentation and remained stable in all cases. Total follow-up duration was six months in two cases, while the rest had one year of follow-up.
In our study, all the patients had mild fever and treatment was symptomatic in most cases at the local hospitals, without extensive diagnostic evaluation. Review of records showed the treatment included a wide range of drugs such as broad-spectrum antimicrobials and often in addition to it an anti-malarial or anti-parasitic agent. By the time patients reported to a retinal specialist for diminution of vision, the initial fever had subsided and patients did not report having any systemic symptoms. It is important to note that all the cases were otherwise healthy—immunocompetent individuals. None of the patients gave a history of fever associated with rash or joint pains and all tested negative for Herpes, Toxoplasma, and HIV or sexually transmitted diseases. Detailed history and examination were negative for the other likely factors, which could contribute toward a compromised immune system, such as advanced age, diabetes mellitus, cancer, use of corticosteroids, immunosuppressive therapy or radiation treatment. There was no history of ocular procedures involving administration of corticosteroids in the form of peribulbar or intraocular injection. It becomes imperative to highlight the former; since Takakura et al. [7] and associates described five patients, who developed necrotizing herpetic retinitis following intraocular or periocular corticosteroid administration.
It is noteworthy that, in a study by Kawali et al. [3] who had reported a larger number of similar clinical presentations in southern India; there was no significant difference between the clinical outcome of the cases—whose therapy was guided by a positive serology, vis-a-vis those who tested negative. Therefore, patients who were treated with specific therapeutic agents—antivirals or antibacterials—in addition to corticosteroids; did not have a different outcome, compared to those who were treated on corticosteroids alone, in the absence of a serological diagnosis. In their study of 119 patients, PCR testing did not yield positive results in any of the cases [3]. There appears to be a lack of direct evidence of an infectious etiology at the time of active retinitis. In addition, most cases did not have a specific etiological diagnosis of fever and were presumed to have a ‘viral-fever’ like illness by treating physicians. They could, however, establish serological diagnosis of Chikungunya, Dengue and Rickettsia in some of their cases; while interestingly multiple serologies turned positive in individual samples, in cases of several patients. This makes it rather speculative—whether presumptive etiology could be used to guide therapeutic intervention in this subset of retinitis cases.
Viral infections occur in close synchrony with environmental factors; the vector responsible for transmission of virus, is directly influenced by conducive environmental conditions for its own breeding and dissemination [8, 9]. Serological assays tend to remain positive, in a population, long after the epidemic or illness has subsided [5, 10]. Serologies may not provide a definitive evidence of an ongoing ocular infection in this subset of retinitis and guiding treatment based on the same is unlikely to yield better results and could sometimes delay institution of anti-inflammatory therapy.
Another study published in 2014 by Vishwanath et al. [4] from southern India, was first of its kind, describing a series of 14 cases; presented over a period of one year. Authors suggested that, irrespective of the cause of fever, clinical presentation of cases was similar with inner-retinitis at the posterior pole and a favorable response to steroids, suggesting a possible immunological basis for this condition. In their case series of 14 patients, only four cases had identifiable etiology—one each of chikungunya, enteric fever, malaria and abdominal abscess. All the cases presented with anterior segment inflammation [4].
Our study varies from study by Vishwanath et al. [4] in two aspects: one—none of our cases presented with anterior segment inflammation and no patient was found to have any identifiable cause of the febrile episode. Another important aspect highlighted by our study is the geographic endemicity that could play an important role in the occurrence of variable presentation in these cases [6]. The cases of retinitis presenting concurrently with the episode of fever are more likely to yield serological diagnosis. Our cases uniformly presented with visual symptoms, once the fever had completely subsided. Both the previous studies [3, 4] have been reported from southern India, while our study is from a tertiary eye institute of central India—this could be a harbinger of future similar presentations in central India. It will also be interesting to note if COVID pandemic alters its clinical picture or epidemiology in any way.
Of special mention is our case 2, where despite all possible interventions—diagnostic vitreous surgery, antiviral medications and systemic steroids; the retinitis showed a dual pattern. The old lesions responded to corticosteroids and subretinal fluid resolved, but the appearance of new lesions or evolution of existing ones could not be prevented. Again, a fresh crop of lesions in both eyes appeared, despite the patient being on antiviral therapy. The PCR testing did not yield a positive result. Although antivirals are known to suppress viral replication below the threshold of detection by PCR [11]. However, in this case the antiviral therapy was initiated after diagnostic vitreous surgery, and once the procurement of vitreous for PCR testing was completed.
Depending heavily on establishing serological and molecular diagnosis, to guide therapeutic approach in these cases—could result in delaying the most important pivotal therapy, i.e., corticosteroids—once this clinically distinct subset of retinitis has been established. Although, systemic examination and detailed laboratory work-up are imperative, in order to rule out latent or ongoing systemic infections, like tuberculosis, before initiation of corticosteroid therapy. Detailed serology undertaken to guide specific therapeutic approach, does not appear to alter the clinical outcome; as seen in our cases as well as previously published data [12]. Invasive diagnostic modalities and PCR testing could be undertaken; especially under the circumstance, when primary failure to corticosteroid therapy has been established or there is a continued progression of retinitis despite adequate therapy. Aggressively increasing the dose of corticosteroids in the early phase of therapy should be avoided, since the response to the same could be variable and irreversible damage could result in case of a missed diagnosis of underlying infectious etiology. Posterior sub-tenon’s depot corticosteroid injection must be fully avoided, in view of irreversibility of the procedure—in cases where primary treatment failure requires a revised therapeutic approach.
Detailed laboratory evaluation to establish the etiology of fever, appears more relevant, during active febrile illness in guiding its management per se [12]. All our patients presented after the acute febrile illness had subsided, and once the clinical ocular diagnosis was established, corticosteroid therapy was initiated without delay. We ordered investigations, such as complete blood counts, renal function tests, liver function tests, HIV, Hepatitis B surface antigen test, Hepatitis C antibody test, radiograph chest, diabetic profile, and blood pressure. Once it was established that the patient is systemically well, based on laboratory investigations and physical exam—there did not appear a need to subject them extensively to another expensive battery of serological investigations. And this could be a rather practical and feasible clinical approach, in a resource limited country like ours; where this subset of retinitis following fever appears to be endemic, based on published literature.
Treatment with corticosteroids, tapered based on clinical response, appears adequate and effective in hastening resolution of lesions, irrespective of the etiology of preceding febrile illness. These cases of fever associated retinitis are self-limiting; however, the timely administration of corticosteroids keeps a check on collateral inflammatory damage. This is the first time we are reporting this pattern from a tertiary referral instiute from central India and have primarily studied and reported the clinical features, presentation and the management of these cases. There has been a focus on elucidating the differences between the clinical characteristics of fever-associated retinitis, from established viral-retinitis, and to understand the significance of extensive serological and invasive diagnostic tests in their management and outcome. However, we will need to further analyze more such cases in coming years, to better understand the epidemiology, especially in the background of COVID pandemic. Also, the small number of cases and retrospective and observational nature of the study combined with limited availability of the evaluation data from previous febrile illness, could constitute the limitations of this study.
Conclusion
Post fever retinitis appears to be a distinct subset of acute non-necrotizing retinitis, with reports from Indian subcontinent, based on the published literature. It presents, following a febrile illness, of indeterminate etiology—possibly a viral flu-like illness. Clinical examination to identify its distinct morphological picture is important and helps distinguish it from the established forms of infectious retinitis. It usually has a self-limiting course, which could be modified by initial therapy with systemic corticosteroids—that needs to be titrated based on clinical response. Intensive serological and laboratory work-up, including PCR tests on ocular fluids may not benefit the clinical course or alter the outcome. The visual outcome is usually satisfactory with timely diagnosis and treatment. No recurrences or neovascular complications were noted during a follow-up period of up to one year.
References
Yoser SL, Forster DJ, Rao NA (1993) Systemic viral infections and their retinal and choroidal manifestations. Surv Ophthalmol 37(5):313–352
Bloch-Michel E, Nussenblatt RB (1987) International Uveitis Study Group recommendations for the evaluation of intraocular inflammatory disease. Am J Ophthalmol 103(2):234–235
Kawali A, Srinivasan S, Mohan A, Bavaharan B, Mahendradas P, Shetty B (2020) Epidemic retinitis with macular edema-treatment outcome with and without steroids. Ocul Immunol Inflamm 20:1–5
Vishwanath S, Badami K, Sriprakash KS, Sujatha BL, Shashidhar SD, Shilpa YD (2014) Post-fever retinitis: a single center experience from south India. Int Ophthalmol 34(4):851–857
Mahendradas P, Kawali A, Luthra S, Srinivasan S, Curi AL, Maheswari S, Ksiaa I, Khairallah M (2020) Post-fever retinitis—newer concepts. Indian J Ophthalmol 68(9):1775–1786
Kawali A, Srinivasan S, Mahendradas P, Shetty B (2020) Epidemic retinitis and community outbreaks. Indian J Ophthalmol 68(9):1916–1919
Takakura A, Tessler HH, Goldstein DA, Guex-Crosier Y, Chan CC, Brown DM, Thorne JE, Wang R, Cunningham ET (2014) Viral retinitis following intraocular or periocular corticosteroid administration: a case series and comprehensive review of the literature. Ocul Immunol Inflamm 22(3):175–182
Colwell RR, Patz JA (1998) Climate, infectious disease and health: an interdisciplinary perspective: a colloquium was convened by the American Academy of Microbiology to discuss research issues relating to the effects of climate on the incidence and distribution of infectious disease. The colloquium was held in Montego Bay, Jamaica, June 20–22, 1997. American Society for Microbiology, Washington, DC
Fisman D (2012) Seasonality of viral infections: mechanisms and unknowns. Clin Microbiol Infect 18(10):946–954
Rathinam SR, Tugal-Tutkun I, Agarwal M, Rajesh V, Egriparmak M, Patnaik G (2020) Immunological tests and their interpretation in uveitis. Indian J Ophthalmol 68(9):1737–1748
Tran TH, Rozenberg F, Cassoux N, Rao NA, LeHoang P, Bodaghi B (2003) Polymerase chain reaction analysis of aqueous humour samples in necrotising retinitis. Br J Ophthalmol 87(1):79–83
Bhaskaran D, Chadha SS, Sarin S, Sen R, Arafah S, Dittrich S (2019) Diagnostic tools used in the evaluation of acute febrile illness in South India: a scoping review. BMC Infect Dis 19(1):970
Funding
None.
Author information
Authors and Affiliations
Contributions
SK worked up and clinically managed the cases. SK and DS performed the literature review and drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Data availability
Not applicable.
Animal research (ethics)
Not applicable.
Ethics approval and consent to participate
The institutional review board did not require protocol approval for preparation and publication of such case series. All patients enrolled in this case series provided signed informed consent for the investigations and treatments carried out at the hospital. Their clinical charts were reviewed in order to obtain data and clinical information used in this manuscript. This manuscript does not contain any patient identifying information.
Consent to publish (ethics)
Informed consent was obtained from all the patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karkhur, S., Soni, D. Clinical spectrum, disease course and management outcome of post-fever retinitis cases: experience from a tertiary eye institute in central India. Int Ophthalmol 42, 2697–2709 (2022). https://doi.org/10.1007/s10792-022-02258-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02258-w