Abstract
Purpose
To compare the safety and the effectiveness of one-port vs. three-port diagnostic vitrectomy in undiagnosed cases of posterior segment inflammation.
Methods
We retrospectively collected data from 80 consecutive diagnostic vitrectomies performed using a one-port (n = 40) or a three-port approach (n = 40). Cases of suspected postoperative endophthalmitis were not included in the study. Several variables were compared among groups, including length of surgery, postoperative best-corrected visual acuity (BCVA), diagnostic success and surgical complications.
Results
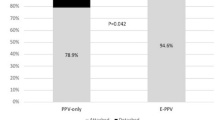
The mean duration of surgery was shorter in the one-port group when compared to the three-port group (15 ± 8 min vs. 49 ± 30; p = 0.0001). The patients were observed for a mean follow-up of 19 months (range 1–84). In the one-port group, the mean BCVA improved from 1.31 ± 0.96 to 0.57 ± 0.59 logarithm of minimum resolution (LogMAR) (p = 0.0009). In the three-port group, BCVA improved from 0.98 ± 0.76 to 0.51 ± 0.76 LogMAR (p = 0.0005). The difference in mean postoperative BCVA between groups was not significative at the last follow-up. One-port vitrectomy yields to a final diagnosis in 80% of the cases, and three-port vitrectomy in 48%. Most of the one-port vitrectomies were carried out under topical anesthesia. After surgery, in both groups three eyes developed a retinal detachment.
Conclusions
In this pilot study, the one-port diagnostic vitrectomy has proven to be as effective and safe as the three-port approach, allowing a reduction in surgical times. One-port diagnostic vitrectomy might be considered as the first option for those cases where more complex surgical procedures are not needed.

Similar content being viewed by others
References
Margolis R, Brasil OFM, Lowder CY, Singh RP, Kaiser PK, Smith SD, Perez VL, Sonnie C, Sears JE (2007) Vitrectomy for the diagnosis and management of uveitis of unknown cause. Ophthalmology 114:1893–1897. https://doi.org/10.1016/j.ophtha.2007.01.038
Patel DS, Khan IJ, Zayed MG, Partridge D, Rennie IG, Mudhar HS, Sheard R (2018) Full diagnostic vitrectomy with posterior vitreous detachment induction for the diagnosis of vitritis due to uncertain etiology. Retina 39:1872–1879. https://doi.org/10.1097/IAE.0000000000002243
Carrol DM, Franklin RM (1981) Vitreous biopsy in uveitis of unknown cause. Retina 1:245–251
Sen HN, Bodaghi B, Hoang PL, Nussenblatt R (2009) Primary intraocular lymphoma: diagnosis and differential diagnosis. Ocul Immunol Inflamm 17:133–141. https://doi.org/10.1080/09273940903108544
Chan CC, Sen HN (2013) Current concepts in diagnosing and managing primary vitreoretinal (intraocular) lymphoma. Discov Med 15:93–100
Donahue SP, Kowalski RP, Brian H, Friberg TR (1993) Vitreous cultures in suspected endophthalmitis biopsy or vitrectomy? Ophthalmology 100:452–455. https://doi.org/10.1016/S0161-6420(93)31623-4
Harper TW, Miller D, Schiffman JC, Davis JL (2009) Polymerase chain reaction analysis of aqueous and vitreous specimens in the diagnosis of posterior segment infectious uveitis. AJOPHT 147:140–147. https://doi.org/10.1016/j.ajo.2008.07.043
Oshima Y, Wakabayashi T, Sato T, Ohji M, Tano Y (2010) A 27—gauge instrument system for transconjunctival sutureless microincision. Ophthalmology 117:93–102.e2. https://doi.org/10.1016/j.ophtha.2009.06.043
Doft D, Donnelly H (1991) A single sclerotomy vitreous biopsy technique in endophthalmitis. Arch Ophthalmol 109:465
Pion B, Valyi Z, Janssens X, Koch P, Libert J, Caspers L, Willermain F (2013) Vitrectomy in uveitis patients. Bull Soc Belge Ophtalmol 322:55–61
Han D, Wisniewski S, Kelsey S, Doft B, Barza M, Pavan P (1999) Microbiologic yields and complication rates of vitreous needle aspiration versus mechanized vitreous biopsy in the endophthalmitis vitrectomy study. Retina 19:98–102
Cimino L, Aldigeri R, Marchi S, Mastrofilippo V, Viscogliosi V, Coassin M, Soldani A, Luisa S, De Fanti A, Belloni L, Zerbini A, Parmeggiani M, Chersich M, Soriano A, Salvarani C, Fontana L (2018) Changes in patterns of uveitis at a tertiary referral center in Northern Italy: analysis of 990 consecutive cases. Int Ophthalmol 38:133–142. https://doi.org/10.1007/s10792-016-0434-x
Holladay JT (1997) Proper method for calculating average visual acuity. J Refract Surg 13:388–391
Priem H, Verbraeken H, De Laey J (1993) Diagnostic problems in chronic vitreous inflammation. Arch Clin Exp Ophthalmol 231:453–456
Rizzo S, Belting C, Genovesi-Ebert F (2010) Retinal detachment after small-incision, sutureless pars plana vitrectomy: possible causative agents. Graefes Arch Clin Exp Ophthalmol 248:1401–1406. https://doi.org/10.1007/s00417-010-1404-z
Schrey S, Krepler K, Wedrich A (2006) Incidence of rhegmatogenous retinal detachment after vitrectomy in eyes of diabetic patients. Retina 26:149–152
Chan A, Leng T, Moshfeghi D (2012) Cannula-based 25-gauge vitreous tap and injection: a new surgical technique. Retina 32:1021–1022
Vahedi S, Adam MK, Dollin M, Maguire JI (2017) 25-Gauge trocar cannula for acute endophthalmitis-related in-office vitreous tap and injection patient comfort and physician ease of use. Retina 37:657–661
Lobo A, Lightman S (2003) Vitreous aspiration needle tap in the diagnosis of intraocular inflammation. Ophtalmology 110:595–599. https://doi.org/10.1016/S0161-6420(02)01895-X
Huang JS, Russack V, Flores-Aguilar M, Gharib M, Freeman WR (1993) Evaluation of cytologic specimens obtained during experimental vitreous biopsy. Retina 13(2):160–165
Jiang T, Zhao Z, Chang Q (2014) Evaluation of cytologic specimens obtained during experimental vitreous biopsy using B-cell lymphoma line. Eur J Ophthalmol 24:911–917. https://doi.org/10.5301/ejo.5000488
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This study was approved by the Ethical Committee of Reggio Emilia.
Informed consent
Informed consent was obtained for all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Coassin, M., Braconi, L., Sborgia, G. et al. One-port vs. three-port diagnostic vitrectomy for posterior segment diseases of unknown origin. Int Ophthalmol 40, 3217–3222 (2020). https://doi.org/10.1007/s10792-020-01504-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01504-3