Abstract
The previous acute respiratory diseases caused by viruses originating from China or the middle east (e.g., SARS, MERS) remained fast developing short diseases without major sequalae or any long-lasting complications. The new COVID-19, on the other hand, not only that it rapidly spread over the world, but some patients never fully recovered or even if they did, a few weeks later started to complain not only of shortness of breath, if any, but general weakness, muscle pains and ‘brain fog’, i.e., fuzzy memories. Thus, these signs and symptoms were eventually labelled ‘long COVID’, for which the most widely used definition is ‘new signs and symptoms occurring 4–8 weeks after recovering from acute stage of COVID-19’. The other most frequent manifestations associated with long COVID include headache, loss of memory, smell and of hair, nausea, and vomiting. Thus, long COVID is not a simple disease, but complex disorder of several organ systems malfunctioning; hence, it is probably more appropriate to call this a syndrome. The pathogenesis of long COVID syndrome is poorly understood, but initial and persistent vascular endothelial injury that often triggers the formation of microthrombi that if dislodged as emboli, damage several organs, especially in the brain, heart and kidney, by creating microinfarcts. The other major contributory mechanistic factor is the persistent cytokine storm that may last longer in long COVID patients than in others, probably triggered by aggregates of SARS-Co-2 discovered recently in the adrenal cortex, kidney and brain. The prevalence of long COVID is relatively high, e.g., initially varied 3–30%, and recent data indicate that 2.5% of UK population suffers from this syndrome, while in the US 14.7% of acute COVID-19 patients continued to have symptoms longer than 2 months. Thus, the long COVID syndrome deserves to be further investigated, both from clinical and basic research perspectives.
Similar content being viewed by others
Introduction
When COVID-19 was first detected at the end of 2019 in China, it appeared to be ‘just another’ acute respiratory infection… The prediction was plausible, especially since similar viral, respiratory infections, mostly originating from animals, appeared several times in or around China during the last 20 years. The manifestation and presentations of COVID-19 were similar to those of SARS (Severe Acute Respiratory Syndrome) that occurred in 2003 and to those of MERS (Middle East Respiratory Syndrome). MERS was first reported in Saudi Arabia in 2012, but both the initial SARS and MERS looked “flu”-like diseases, with most cases resolving, without any residual sequalae in a few days or weeks.
COVID-19, on the other hand, was soon accompanied by higher rates of mortality than SARS and MERS. Because of this recognition, and due to the rapid spread of this new infection caused by SARS-CoV-2, we published 2020 a short review entitled “COVID-19: New disease and chaos with panic, associated with stress” (Szabo 2020). And when the initial panic and chaos settled, new problems related to COVID-19 started to appear, i.e., this is more than a simple, acute respiratory disease that resolves quickly, since some long-lasting sequelae would remain in 6–30% of patients that are related to other organs besides the respiratory tract (Lopez-Leon et al. 2021) (Fig. 1). As it was recently summarized, “patients wrote ‘the first textbook’ on long COVID” (Ochoa 2022). This review was mostly based on Ryan Prior’s “The Long Haul” book which chronicles the patient-led fight to officially recognize and treat long COVID (Prior 2022). Actually, it is worth quoting more from recent publications: “‘Long hauler’, if the phrase is still unfamiliar, refers to someone who has not recovered after a COVID infection or who has long COVID—a multisystem syndrome with myriad symptoms ranging from profound exhaustion to cognitive impairment. Both “long hauler” and “long COVID” were terms coined by patients—itself a unique phenomenon; diseases are usually named by the doctors who discover them. Although long COVID is caused by a novel virus, post-infection disease is not new. Think of post-polio syndrome and AIDS.”
Thus, in this short review, we will show a typical case of long COVID, provide a few definitions of long COVID, discuss its epidemiology, pathogenesis and main clinical manifestations as well as the very few therapeutic options we may have.
A typical case of long COVID
Although case reports in review article usually originate from clinical journals, we find a simple, very vivid description of a young boy suffering from than a year after acute COVID-19 (Fig. 2). As most infected people, he expected to get better in a few days—but got sicker and sicker, with a multitude of signs and symptoms originating from other than the respiratory system: not only nausea, general fatigue, but headaches, and what scared him the most—‘faltering memory’… In most long COVID case reports, the latter is referred to as ‘brain fog’ that affects both young and old patients. Although his parents took him to many doctors and clinics, nobody could provide any meaningful, effective treatment. Only after more than a year, he started to regain his good physical condition and mental well-being.
Definitions of long COVID
It may not be surprising that a disease or syndrome, with such a complex presentation, involving virtually all organs of the body, does not have a uniformly accepted definition. And it’s not from lack of trying, e.g., the NIH, WHO and other prominent national and international organizations offered their definitions. The initial, most widely used definition was ‘New signs and symptoms occurring 4–8 weeks after recovering from the acute stage of COVID-19’ (Fig. 3). But since the presenting signs of long COVID are so nonspecific, e.g., similar to the poorly understood, often used and criticised ‘chronic fatigue’, experts soon realized that long COVID should be a diagnosis by exclusion, e.g., all other possible cardiac, pulmonary, gastrointestinal and neurologic causes must be eliminated. Furthermore, a seminal French study, published in January 2022, involving more than 3000 patients invoked another important and objective diagnostic criterion: patients must have an early positive PCR or antigen SARS-CoV-2 test to label their condition as ‘long COVID’ (Slomski 2022). Thus, the most wide definition nowadays is: presenting signs and symptoms and/or NEW malaise continuing after 4 weeks, after laboratory-proven acute COVID-19 infection, despite therapeutic attempts.
Since long COVID is not a simple disease that has clear etiology, pathogenesis and clinical course, but a complex disorder involving many organs at the same time, it’s appropriate to call this long COVID syndrome (LCS). In this context, it’s similar to the ‘stress syndrome’, as originally described by Hans Selye based on his seminal animal experiments (Selye 1936), subsequently expanded by numerous clinical observational and investigational studies (Selye 1976; Szabo et al. 2012). Another similarity to the ‘stress syndrome’ may be that as the mechanisms of biological stress response were poorly understood 60–70 years ago, its neuroendocrine molecular and cellular pathogenesis is well described nowadays. Hopefully, we do not have to wait for such a long time to gain insights into the pathogenesis of LCS.
Pathogenesis of long COVID
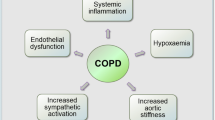
A recent short review article contained a subtitle: “Long COVID: A frequent syndrome with unclear pathogenesis” (Yavropoulou et al. 2022). This is indeed a short and crisp assessment of our sad situation with the understanding of the molecular and cellular mechanisms of long COVID. The little we know so far about the pathogenesis is summarized in Fig. 4. Namely, we know from the early research on the mechanisms of acute COVID-19 that the initial cellular targets are the epithelial cells lining the nose, bronchi and alveolar sacs in the lung. These cells represent the entry point of the SARC-Co-2 in the organism, but surprisingly, despite being the original targets, the virus entry was followed only by mild inflammation, contrary to the clinical presentation of initial SARS and MERS that were associated with severe pneumonia and bronchitis.
On the other hand, severe COVD-19 patients suffered from a rapidly developing lung edema, i.e., accumulation of fluid in the alveolar spaces that are normally filled only with air, since the venous blood is oxygenated there before returning to the heart for distribution of oxygenated blood to our organs. Such a rapidly developing pulmonary edema could come only from increased vascular permeabilities, i.e., from arterioles, capillaries and venules surrounding the alveolar sacs, as illustrated in Fig. 4. Mechanistically, increased vascular permeability is usually triggered by a sudden release of histamine from nearby mast cells or of vascular endothelial growth actor (VEGF) which is usually stored/bound to heparin in the adjacent loose connective tissue. Not too many people know that the initial name of VEGF was VPF (vascular permeability factor) which on a molar basis is more potent than histamine to cause vascular leakage (Dvorak et al. 1995). VPF/VEGF receptors, flt-1 and kdr, are overexpressed by endothelial cells that line the microvessels that supply alveoli, and because of these pathogenic elements, numerous clinical reports showed the beneficial effects of bevacizumab, an anti-VPF/VEGF in treating patients with severe forms of COVID-19, and new clinical trials are still ongoing (Pang et al. 2021; Sahebnasagh et al. 2021).
Figures 4 and 5 also illustrate the transition of vascular-based elements into the development of long COVID, like the cytokine storm, fibrin clots on the damaged capillary endothelial cells that attract platelets, over which fibrin fibres to form thrombus. The additional pathogenic factor in long COVID is that this microthrombi may get dislodged and form microemboli distributed all over the body, creating ischemic microinfarcts in several organs, especially in the brain that may lead to impairment in brain functions that patients may experience in the form of ‘brain fog’. Furthermore, recently SARS-Co-2 aggregates have been identified in organs other than the lungs, e.g., in brain, kidney, muscle, peripheral nerves, adrenal cortex (Weixel 2022). Thus, mechanistically, “COVID-19 is, in the end, an endothelial disease” (Libby and Luscher 2020), as some of us were proposing from the very beginning of this pandemic, in part because of the similar, critical role of vascular factors in the cellular and molecular pathogenesis of gastrointestinal (GI) ulceration (Szabo 2020, 2021).
Epidemiology of long COVID
The data on the epidemiology of long COVID is still evolving, but we know from early reports that the initial prevalence (i.e., the total number of long COVID patents in a given population, e.g., hospital, city, country) in 2020 was 3–30% among COVID-19 patients. Recent data from the UK demonstrate that 2.5% of the entire population experience various forms of long COVID. We now also know that prior vaccination offers some protection against LCS, but it may still occur even in 25% of fully vaccinated people! The recent Israeli data (Kreier 2022), based on the self-reported vaccination status, fully vaccinated participants who had acute COVID-19 offered considerable protection (Fig. 6). A very recent cross-sectional study involving 16, 091 participants from the USA 14.7% reported continued COVID-19 symptoms more than 2 months after acute illness (Perlis et al. 2022). This study also “suggests that long COVID is prevalent and associated with female gender and older age, while risk may be diminished by completion of primary vaccination series prior to infection.”
There are no reliable data on the incidence, i.e., the frequency of new cases in a given community, during a fixed time period (e.g., 1 year), probably due to study design difficulties and the relatively short period that is available for data collection in this new pandemic.
Treatment possibilities
The best approach to eliminate any disease is the etiologic treatment, like antibiotics for most infectious diseases. In the long COVID syndrome, with multiple organ involvements, as the pooled prevalence indicates (Fig. 7), our pharmacologic approaches are restricted and often not very successful, especially since even with modern, specific anti-SARS-Co-2 viral drugs, the elimination of etiologic agents has not brought on permanent improvements for long COVID patients. Most likely the lack of success is due to the fact that the initial organ damage in the lungs, vascular system and the poorly understood cytokine storm is percolating in the background. Furthermore, symptoms may be new onset, following initial recovery from an acute COVID-19 episode, or persist from the initial illness. These symptoms may also fluctuate or relapse over time, making treatment choices very difficult that leads to frustration both in patients and clinicians. In addition, symptoms may affect various organ systems and not necessarily organs where the preceding viral infection occurred.
Furthermore, since COVID-19 is a multi-organ damage with a substantial inflammatory component in its pathogenesis, nevertheless NSAID therapy did not show substantial benefits, neither in acute nor in long COVID. On the other hand, glucocorticoids, which as part of their anti-inflammatory action, also decrease vascular permeability, showed benefits in multiple patient populations. As expected, the synthetic glucocorticoid dexamethasone, which is about 20 times more potent than the natural cortisol, was the most widely used synthetic corticosteroid (The RECOVERY Collaborative Group 2021).
Thus, in conclusion, the long COVID syndrome is not only that it is poorly understood in its pathogenesis, but it poses major challenges in treatment choices. Hopefully, new and intensive clinical and basic research during the next few years will bring major improvements in our understanding of the development, mechanisms and treatment of long COVID.
Data availability
The data used to support the finding are cited within the article.
Abbreviations
- COVID-19:
-
Coronavirus disease-2019
- LCS:
-
Long COVID syndrome
- MERS:
-
Middle east respiratory syndrome
- NIH:
-
National Institutes of Health
- PCR:
-
Polymerase chain reaction
- SARS:
-
Severe acute respiratory syndrome
- SARS-CoV-2:
-
Severe acute respiratory syndrome-coronavirus 2
- VPF/VEGF:
-
Vascular permeability factor/vascular endothelial growth factor
- WHO:
-
World Health Organization
References
Dvorak HF, Detmar M, Claffey KP, Nagy JA, Van der Water L, Senger DL (1995) Vascular permeability factor/vascular endothelial growth actor: an important mediator pf angiogenesis in malignancy and inflammation. Int Arch Allergy Immunol 107:233–235
Kreier F (2022) Long-COVID symptoms less likely in vaccinated people, Israeli data say. Nature. https://doi.org/10.1038/d41586-022-00177-5
Libby P, Luscher T (2020) COVID-19 is, in the end, an endothelial disease. Eur Heart J 41:3038–3044
Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, Villapol S (2021) More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep 11:16144
Ochoa S (2022) How patients wrote ‘the first textbook’ on long COVID. Los Angeles Times, Nov. 16
Pang J, Xu F, Aondio G, Li Y, Fumagalli A, Lu M (2021) Efficacy and tolerability of bevacizumab in patients with severe Covid-19. Nat Commun 12:814. https://doi.org/10.1038/s41467-021-21085-8
Perlis RH, Santillana M, Ognyanova K, Safarpour A, Trujillo KL, Simonson MD, Green J, Quintana A, Druckman J, Baum MA, Lazer D (2022) Prevalence and correlates of long COVID symptoms among US adults. JAMA Network Open 5(10):e2238804
Prior R (2022) The Long Haul: solving the puzzle of the pandemic’s long haulers and how they are changing healthcare forever. Post Hill Press-Simon & Schuster, New York, p 336
Sahebnasagh A, Nabavi SM, Kashani HRK, Abdollahian S, Habtemariam S, Rezabakhsh A (2021) Anti-VEGF agents: as appealing targets in the setting of COVID-19 treatment in critically ill patients. Intern Immunopharmacol 191:108257
Selye H (1936) A syndrome produced by diverse nocuous agents. Nature 138:132
Selye H (1976) Stress in health and disease. Butterworth’s Inc., Boston
Slomski A (2022) Belief in having had COVID-19 linked with long COVID symptoms. JAMA 327(1):26. https://doi.org/10.1001/jama.2021.23318
Szabo S, Tache Y, Somogyi A (2012) The legacy of Hans Selye and the origins of stress research: a retrospective 75 years after his landmark “letter” in Nature. Stress 15:472–478
Szabo S (2020) COVID-19: new disease and chaos with panic, associated with stress. Med Sci 59:41–62
Szabo S (2021) Vascular endothelial injury: common element in the cellular and molecular pathogenesis of GI ulceration and COVID-19. In: Proceedings of the 14th international conference cell/tissue injury and cytoprotection/cytoprotection. PECS, Hungary, p 12
The RECOVERY Collaborative Group (2021) Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 384:693–704
Weixel N (2022) Study suggests coronavirus lingers in organs for months. https://thehill.com/policy/healthcare/587391-study-suggests-coronavirus-lingers-in-organs-for-months/
Yavropoulou MP, Tsokos GC, Chrousos GP, Sfikakis PP (2022) Protracted stress-induced hypocortisolemia may account for the clinical and immune manifestations of Long COVID. Clin Immunol 245:109133. https://doi.org/10.1016/j.clim.2022.109133
Acknowledgements
No grant support was used to prepare this manuscript.
Funding
No funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Szabo, S., Zayachkivska, O., Hussain, A. et al. What is really ‘Long COVID’?. Inflammopharmacol 31, 551–557 (2023). https://doi.org/10.1007/s10787-023-01194-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-023-01194-0