Abstract
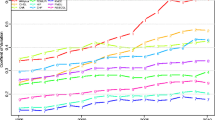
Despite the huge attention on the long average hospital length of stay (LOS) in Japan, there are limited empirical studies on the impacts of the payment systems on LOS. In order to shed new light on this issue, we focus on the fact that reimbursement for hospital care is linked to the number of patient bed-days, where a “day” is defined as the period from one midnight to the next. This “midnight-to-midnight” definition may incentivize health care providers to manipulate hospital acceptance times in emergency patients, as patients admitted before midnight would have an additional day for reimbursement when compared with those admitted after midnight. We test this hypothesis using administrative data of emergency transportations in Japan from 2008 to 2011 (N = 2,146,498). The results indicate that there is a significant bunching in the number of acceptances at the emergency hospital around midnight; the number heaps a few minutes before midnight, but suddenly drops just after midnight. Given that the occurrence of emergency episode is random and the density is smooth during nighttime, bunching in the number of hospital acceptances around midnight suggests that hospital care providers shift the hospital acceptance times forward by hurrying-up to accept the patients. This manipulation clearly leads to longer LOS by one bed-day. In addition, the manipulation is observed in the prefectures where private hospitals mainly provide emergency medical services, suggesting hospital ownership is associated with the manipulation of hospital acceptance time.







Similar content being viewed by others
Notes
Ikegami and Campbell (1995) argue that the long LOS in Japan does not lead to high costs, for several reasons. For example, they note that the number of new admission per capita is low in Japan partly because of the country’s high utilization rates for outpatient care, and that the total daily reimbursement rate for hospital care is also kept low.
In Noguchi and Shimizutani (2011), patients who no longer require acute medical care but remain hospitalized for more than 180 days are defined as “socially hospitalized” patients.
Note that Noguchi et al. (2008) use the Tokai Acute Myocardial Infarction Study, which is not nationally representative, but their data seem to be the most comprehensive data on the mortality of AMI patients in Japan.
The results from empirical studies on the impact of payment systems on physician behavior are mixed: although some studies have reported a strong link between payment systems and health care provision (Delattre and Dormont 2003; Devlin and Sarma 2008; Shafrin 2010; van Dijk et al. 2013), others have found no such associations (Hadley et al. 1979; Grytten and Sorensen 2001).
Echevin and Fortin (2014) investigated the effects of alternative payment systems on LOS and the probability of readmission by exploiting the introduction of a new reimbursement scheme in Quebec.
This description is based on the Japanese system. The U.S. Medicare and Medicaid system excludes the day of discharge and death from the calculation of bed-days. A new rule for reimbursements in the U.S. also uses the number of midnights to assign inpatient status. In 2014, the Centers for Medicare and Medicaid Services introduced a “2-midnight rule”. Under this rule, Medicare Part A covers hospitalizations of 2 midnights (“2 days”) or longer; in contrast, stays shorter than 2 midnights are regarded as outpatient episodes for observation, and are therefore not covered by Medicare Part A (Sheehy et al. 2013).
Since patients are generally discharged during morning hours (e.g., 8 a.m. to 12 a.m.), hospitals cannot also manipulate the date of discharge.
A general summary of the Japanese EMS system is also provided in Kitamura et al. (2010).
There are currently 266 emergency critical care centers located throughout Japan. Not all are government-owned, but the prefectural governments are generally responsible for the management of these centers.
Unfortunately, our data did not include the time of symptom onset. Many previous studies such as Smolderen et al. (2010) and Mooney et al. (2014) define “prehospital transport time” as the period from the onset of symptoms to arrival at the hospital, whereas others such as Kleindorfer et al. (2006) and Kitamura et al. (2014) investigated the determinants of the time from the emergency call to arrival at the hospital. On this point, see Online Appendix B.
For hospitals with a high level of nursing staff, the basic per-diem reimbursement is 15,910 JPY, and they typically receive additional reimbursement in the amount of 4500 JPY. Since this additional reimbursement is not paid for once a patient’s LOS exceeds 30 days, the total basic reimbursement per bed-day is 20,410 (= 15,910 + 4500) JPY for patients with a short LOS and 15,910 JPY for those with a long LOS.
These include university hospitals and some national hospitals.
Fire stations in Tokyo are managed by an organization independent of the national government, and as such are not included in the FDMA database.
These classifications do not correspond to diagnostic group classification such as ICD-10. As is shown in Online Appendix B, 72% of emergency calls are due to “disease”.
We found that our main results were largely unaffected for shorter (from 22:00 to 2:00) and longer time intervals (from 20:00 to 4:00). These results are available on request.
If there is an irregular increase of the emergency calls from 0:00 to 0:04 (Fig. 2a), ambulance crews soon have to go to the next place in the same time. Thereby, there may be a rushing on the acceptance of the emergency patients. However, emergency crews cannot change the timing of hospital acceptances to just before midnight after receiving the emergency calls from 0:00 to 0:04. Thus, irregular increases of emergency calls from 0:00 to 0:04 do not account for the bunching of hospital acceptances around midnight.
31,276 − 30,475 = 801.
We appreciate Dr. Ryosuke Ikeda, Dr. Takefumi Osaka, Dr. Nobuo Sakata, and Dr. Takashi Shiga for letting us know of these examples. In addition, we thank the many fire station staff members who responded to our questions.
The width of the CIs appears to depend on the number of observations in each bin, but the point estimates also exhibited no irregular reductions in the number of hospital acceptances in the time interval from 0:00 to 0:04.
There is also a growing body of literature addressing the association between hospital ownership and quality of care (Perotin et al. 2013). Here, we contribute to the literature on the association between hospital ownership and the extent of financial motivations.
As in the total sample results, the existence of manipulation was determined from an irregular deviation of the number of hospital arrivals in the 5-minute interval from 0:00 to 0:04.
The database includes Fukushima and Miyagi prefectures, which suffered immense damage during the 2011 Great East Japan Earthquake. We examined the manipulation at the monthly level and found no trend breaks before and after the disaster.
The t value is calculated as the difference between the actual number and the mean counterfactual number, normalized by the standard error.
Ju¨rges and K¨oberlein (2015) also found that the upcoding was selective as physicians were more likely to upcode DRGs when treating newborns with poor health conditions and high expected health care costs.
In general, the coinsurance rate in Japan is 30% for patients aged from school age to 69 years and 10% for those aged 70 years and older. In addition, the total amount of copayment per month exceeds monthly stop-loss limits.
References
Bayindir, E. E. (2012). Hospital ownership type and treatment choices. Journal of Health Economics, 31(2), 359–370.
Brunt, C. S. (2015). Medicare part b intensity and volume offset. Health Economics, 24(8), 1009–1026.
Chetty, R., Friedman, J. N., Olsen, T., & Pistaferri, L. (2011). Adjustment costs, firm responses, and micro vs. macro labor supply elasticities: Evidence from danish tax records. The Quarterly Journal of Economics, 126(2), 749–804.
Dafny, L. S. (2005). How do hospitals respond to price changes? American Economic Review, 95(5), 1525–1547.
Delattre, E., & Dormont, B. (2003). Fixed fees and physician-induced demand: A panel data study on french physicians. Health Economics, 12(9), 741–754.
Devlin, R. A., & Sarma, S. (2008). Do physician remuneration schemes matter? the case of canadian family physicians. Journal of Health Economics, 27(5), 1168–1181.
Dranove, D. (1988). Demand inducement and the physicians/patient relationship. Economic Inquiry, 26(2), 281–298.
Echevin, D., & Fortin, B. (2014). Physician payment mechanisms, hospital length of stay and risk of readmission: Evidence from a natural experiment. Journal of Health Economics, 36(1), 112–124.
Einav, L., Finkelstein, A., & Schrimpf, P. (2013). The response of drug expenditures to non-linear contract design: evidence from medicare part D. NBER Working Papers 19393, National Bureau of Economic Research, Inc. http://ideas.repec.org/p/nbr/nberwo/19393.html.
Ellis, R. P., & McGuire, T. G. (1986). Provider behavior under prospective reimbursement: Cost sharing and supply. Journal of Health Economics, 5(2), 129–151.
FDMA. (2010). Annual surveys on emergency transportation and rescue operations in 2010
FDMA. (2012). Annual surveys on emergency transportation and rescue operations. http://www.fdma.go.jp/neuter/topics/fieldList9_3.html. Accessed March 26, 2014.
Fukuoka, Y., Dracup, K., Rankin, S. H., Froelicher, E. S., Kobayashi, F., Hirayama, H., et al. (2005). Prehospital delay and independent/interdependent construal of self among Japanese patients with acute myocardial infarction. Social Science and Medicine, 60(9), 2025–2034.
Fushimi, K. (2006). Prospective payment system for acute inpatient care in Japan (in Japanese: Kyuseiki nyuin iryo no houkatsu shiharai seido no shikumi to sono tekiyou). Financial Review, 80, 33–73.
Grytten, J., & Sorensen, R. (2001). Type of contract and supplier-induced demand for primary physicians in norway. Journal of Health Economics, 20(3), 379–393.
Hadley, J., Holahan, J., & Scanlon, W. (1979). Can fee-for-service reimbursement coexist with demand creation? Inquiry, 16(3), 247–258.
He, D., & Mellor, J. M. (2012). Hospital volume responses to medicare’s outpatient prospective payment system: Evidence from florida. Journal of Health Economics, 31(5), 730–743.
Hennig-Schmidt, H., Selten, R., & Wiesen, D. (2011). How payment systems affect physicians’provision behaviour—an experimental investigation. Journal of Health Economics, 30(4), 637–646.
Hosoda, T., Fujita, T., & Tanihata, T. (2005). Follow-up study on the emergency patients. Journal of Health and Welfare Statistics, 52(6), 27–34. in Japanese.
Ikegami, N., & Campbell, J. C. (1995). Medical care in Japan. New England Journal of Medicine, 333(19), 1295–1299.
Innami, I. (2009). A study on the socially hospitalized patients [in Japanese: Shakaiteki Nyuin no Kenkyu]. Tokyo: Toyo Keizai Inc.
Jacobson, M., Earle, C. C., Price, M., & Newhouse, J. P. (2010). How medicare’s payment cuts for cancer chemotherapy drugs changed patterns of treatment. Health Affairs, 27(9), 1391–1399.
Jürges, H., & Köberlein, J. (2015). What explains DRG upcoding in neonatology? The roles of financial incentives and infant health. Journal of Health Economics, 43, 13–26.
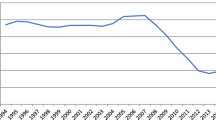
Kato, N., Kondo, M., Okubo, I., & Hasegawa, T. (2014). Length of hospital stay in Japan 1971–2008: Hospital ownership and cost-containment policies. Health Policy, 115(2–3), 180–188.
Kitamura, T., Iwami, T., Kawamura, T., Nagao, K., Tanaka, H., & Hiraide, A. (2010). Nationwide public-access defibrillation in Japan. New England Journal of Medicine, 362(11), 994–1004.
Kitamura, T., Iwami, T., Kawamura, T., Nishiyama, C., Sakai, T., Tanigawa-Sugihara, K., et al. (2014). Ambulance calls and prehospital transportation time of emergency patients with cardiovascular events in Osaka city. Acute Medicine and Surgery, 1(3), 135–144.
Kleindorfer, D. O., Lindsell, C. J., Broderick, J. P., Flaherty, M. L., Woo, D., Ewing, I., et al. (2006). Community socioeconomic status and prehospital times in acute stroke and transient ischemic attack: Do poorer patients have longer delays from 911 call to the emergency department? Stroke, 37(6), 1508–1513.
Lindrooth, R. C., & Weisbrod, B. A. (2007). Do religious nonprofit and for-profit organizations respond differently to financial incentives? The hospice industry. Journal of Health Economics, 26(2), 342–357.
Mendelson, A., Kondo, K., Damberg, C., et al. (2017). The effects of pay-for-performance programs on health, health care use, and processes of care: A systematic review. Annals of Internal Medicine, 166(5), 341–353.
Ministry of Health L, Welfare. (2014). Materials for central social insurance medical council (in Japanese; cyuui kyou shiryou. http://www.mhlw.go.jp/file/05-Shingikai-12404000-Hokenkyoku-Iryouka/0000041708.pdf. (in Japanese).
Mooney, M., McKee, G., Fealy, G., Brien, F. O., O’Donnell, S., & Moser, D. (2014). A randomized controlled trial to reduce prehospital delay time in patients with acute coronary syndrome (ACS). The Journal of Emergency Medicine, 46(4), 495–506.
Motohashi, T., Hamada, H., Lee, J., Sekimoto, M., & Imanaka, Y. (2013). Factors associated with prolonged length of hospital stay of elderly patients in acute care hospitals in Japan: A multilevel analysis of patients with femoral neck fracture. Health Policy, 111(1), 60–67.
Nawata, K., Nitta, A., Watanabe, S., & Kawabuchi, K. (2006). An analysis of the length of stay and effectiveness of treatment for hip fracture patients in Japan: Evaluation of the 2002 revision of the medical service fee schedule. Journal of Health Economics, 25(4), 722–739.
Noguchi, H., & Shimizutani, S. (2011). The determinants of exit from institutions and the price elasticity of institutional care: Evidence from Japanese micro-level data. Journal of the Japanese and International Economies, 25(2), 131–142.
Noguchi, H., Shimizutani, S., & Masuda, Y. (2008). Regional variations in medical expenditure and hospitalization days for heart attack patients in Japan: Evidence from the Tokai acute myocardial study (TAMIS). International Journal of Health Care Finance and Economics, 8(2), 123–144.
OECD. (2015). Health at a glance 2015. http://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2015_health_glance-2015-en.
Perotin, V., Zamora, B., Reeves, R., Bartlett, W., & Allen, P. (2013). Does hospital ownership affect patient experience? An investigation into public-private sector differences in England. Journal of Health Economics, 32(3), 633–646.
Shafrin, J. (2010). Operating on commission: Analyzing how physician financial incentives affect surgery rates. Health Economics, 19(5), 562–580.
Sheehy, A., Graf, B., Gangireddy, S., Formisano, R., & Jacobs, E. (2013). “observation status” for hospitalized patients: Implications of a proposed medicare rules change. JAMA Internal Medicine, 173(21), 2004–2006.
Shigeoka, H., & Fushimi, K. (2014). Supplier-induced demand for newborn treatment: Evidence from Japan. Journal of Health Economics, 35, 162–178.
Silverman, E., & Skinner, J. (2004). Medicare upcoding and hospital ownership. Journal of Health Economics, 23(2), 369–389.
Smolderen, K., Spertus, J., Nallamothu, B., et al. (2010). Health care insurance, financial concerns in accessing care, and delays to hospital presentation in acute myocardial infarction. JAMA, 303(14), 1392–1400.
van Dijk, C. E., van den Berg, B., Verheij, R. A., Spreeuwenberg, P., Groenewegen, P. P., & de Bakker, D. H. (2013). Moral hazard and suppier-induced demand: Empirical evidence in general practice. Health Economics, 22(3), 340–352.
Werner, R. M., Kolstad, J. T., Stuart, E. A., & Polsky, D. (2011). The effect of pay-for-performance in hospitals: Lessons for quality improvement. Health Affairs, 30(4), 690–698.
Yip, W. C. (1998). Physician response to medicare fee reductions: Changes in the volume of coronary artery bypass graft (cabg) surgeries in the medicare and private sectors. Journal of Health Economics, 17(6), 675–699.
Acknowledgements
We thank the Fire and Disaster Management Agency of Japan for allowing access to administrative records of emergency transportations. Although this project was supported by the Institute for Health Economics and Policy, the views expressed in this paper do not necessarily reflect the official views of the institute. We gratefully acknowledge the helpful suggestions and comments from Rei Goto at the annual meeting of the Japanese Economic Association and from Minah Kang at the Tri-Country Joint Health Economics Symposium held in Taipei. We also thank Michihito Ando, Dr. Ryosuke Ikeda, Dr. Takefumi Osaka, Dr. Nobuo Sakata and Dr. Takashi Shiga for their advice. We would like to thank the two anonymous reviewers for their suggestions and comments. All errors are our own.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Takaku, R., Yamaoka, A. Payment systems and hospital length of stay: a bunching-based evidence. Int J Health Econ Manag. 19, 53–77 (2019). https://doi.org/10.1007/s10754-018-9243-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-018-9243-2