Abstract
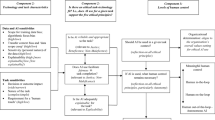
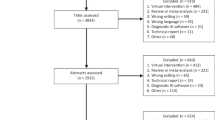
This study seeks to improve the safety of clinical care provided in operating rooms (OR) by examining how characteristics of both the physical environment and the procedure affect surgical team movement and contacts. We video recorded staff movements during a set of surgical procedures. Then we divided the OR into multiple zones and analyzed the frequency and duration of movement from origin to destination through zones. This data was abstracted into a generalized, agent-based, discrete event simulation model to study how OR size and OR equipment layout affected surgical staff movement and total number of surgical team contacts during a procedure. A full factorial experiment with seven input factors – OR size, OR shape, operating table orientation, circulating nurse (CN) workstation location, team size, number of doors, and procedure type – was conducted. Results were analyzed using multiple linear regression with surgical team contacts as the dependent variable. The OR size, the CN workstation location, and team size significantly affected surgical team contacts. Also, two- and three-way interactions between staff, procedure type, table orientation, and CN workstation location significantly affected contacts. We discuss implications of these findings for OR managers and for future research about designing future ORs.







Similar content being viewed by others
Availability of data and material
Data used within this research is protected under an IRB protocol approved by the Medical University of South Carolina.
Code availability
Simulation models were developed in AnyLogic and are available upon request.
References
Joseph A, Khoshkenar A, Taaffe KM, Catchpole K, Machry H, Bayramzadeh S (2019) Minor flow disruptions, traffic-related factors and their effect on major flow disruptions in the operating room. BMJ Qual Saf 28(4):276–283. https://doi.org/10.1136/bmjqs-2018-007957
Joseph A, Bayramzadeh S, Zamani Z, Rostenberg B (2018) Safety, performance, and satisfaction outcomes in the operating room: A literature review. HERD: Health Environments Research & Design Journal 11(2):137–150. https://doi.org/10.1177/1937586717705107
Denton B, Viapiano J, Vogl A (2007) Optimization of surgery sequencing and scheduling decisions under uncertainty. Health Care Manag Sci 10(1):13–24. https://doi.org/10.1007/s10729-006-9005-4
Gupta D, Denton B (2008) Appointment scheduling in health care: Challenges and opportunities. IIE Trans 40(9):800–819
Erdogan SA, Denton BT (2011) Surgery planning and scheduling. In Wiley encyclopedia of operations research and management science
May JH, Spangler WE, Strum DP, Vargas LG (2011) The surgical scheduling problem: Current research and future opportunities. Prod Oper Manag 20(3):392–405. https://doi.org/10.1111/j.1937-5956.2011.01221.x
Cardoen B, Demeulemeester E, Beliën J (2010) Operating room planning and scheduling: A literature review. Eur J Oper Res 201(3):921–932. https://doi.org/10.1016/j.ejor.2009.04.011
Zhu S, Fan W, Yang S, Pei J, Pardalos PM (2019) Operating room planning and surgical case scheduling: A review of literature. J Comb Optim 37(3):757–805. https://doi.org/10.1007/s10878-018-0322-6
Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM (2007) Disruptions in surgical flow and their relationship to surgical errors: An exploratory investigation. Surgery 142(5):658–665. https://doi.org/10.1016/j.surg.2007.07.034
Barie PS, Eachempati SR (2005) Surgical site infections. Surg Clin North Am, 85(6):1115–1135, viii-ix doi:https://doi.org/10.1016/j.suc.2005.09.006
Lynch RJ, Englesbe MJ, Sturm L, Bitar A, Budhiraj K, Kolla S et al (2009) Measurement of foot traffic in the operating room: Implications for infection control. Am J Med Qual 24(1):45–52. https://doi.org/10.1177/1062860608326419
Salassa TE, Swiontkowski MF (2014) Surgical attire and the operating room: Role in infection prevention. J Bone Joint Surg 96(17):1485–1492
Brandt C, Hott U, Sohr D, Daschner F, Gastmeier P, Rüden H (2008) Operating room ventilation with laminar airflow shows no protective effect on the surgical site infection rate in orthopedic and abdominal surgery. Ann Surg 248(5):695–700
McHugh S, Hill A, Humphreys H (2015) Laminar airflow and the prevention of surgical site infection. More harm than good? The Surgeon 13(1):52–58
Smith EB, Raphael IJ, Maltenfort MG, Honsawek S, Dolan K, Younkins EA (2013) The effect of laminar air flow and door openings on operating room contamination. J Arthroplasty 28(9):1482–1485
Perez P, Holloway J, Ehrenfeld L, Cohen S, Cunningham L, Miley GB et al (2018) Door openings in the operating room are associated with increased environmental contamination. Am J Infect Control 46(8):954–956
Barr S, Topps A, Barnes N, Henderson J, Hignett S, Teasdale R et al (2016) Northwest breast surgical research collaborative. Infection prevention in breast implant surgery: A review of the surgical evidence, guidelines and a checklist. Eur J Surg Oncol 42(5):591–603
Panahi P, Stroh M, Casper DS, Parvizi J, Austin MS (2012) Operating room traffic is a major concern during total joint arthroplasty. Clin Orthop Relat Res 470(10):2690–2694
Bédard M, Pelletier-Roy R, Angers-Goulet M, Leblanc P-A, Pelet S (2015) Traffic in the operating room during joint replacement is a multidisciplinary problem. Can J Surg 58(4):232
Sadrizadeh S, Tammelin A, Ekolind P, Holmberg S (2014) Influence of staff number and internal constellation on surgical site infection in an operating room. Particuology 13:42–51
Taaffe K, Lee B, Ferrand Y, Fredendall L, San D, Salgado C et al (2018) The influence of traffic, area location, and other factors on operating room microbial load. Infect Control Hosp Epidemiol 39(4):391–397
Stocks GW, O'Connor DP, Self SD, Marcek GA, Thompson BL (2011) Directed air flow to reduce airborne particulate and bacterial contamination in the surgical field during total hip arthroplasty. J Arthroplast 26(5):771–776
Taaffe K, Allen R, Fredendall L, Shehan M, Stachnik MG, Smith T et al (2020) Simulating the effects of operating room staff movement and door opening policies on microbial load. Infection Control and Hospital Epidemiology:1–5. https://doi.org/10.1017/ice.2020.1359
Way TJ, Long A, Weihing J, Ritchie R, Jones R, Bush M et al (2013) Effect of noise on auditory processing in the operating room. J Am Coll Surg 216(5):933–938
Katz JD (2014) Noise in the operating room. Anesthesiol J Am Soc Anesthesiologists 121(4):894–898
Hasfeldt D, Laerkner E, Birkelund R (2010) Noise in the operating room–what do we know? A review of the literature. J Perianesth Nurs 25(6):380–386. https://doi.org/10.1016/j.jopan.2010.10.001
Palmer G, Abernathy J, Swinton G, Allison D, Greenstein J, Shappell S et al (2013) Realizing improved patient care through human-centered operating room design: a human factors methodology for observing flow disruptions in the cardiothoracic operating room. Anesthesiology 119(5):1066–1077
Wahr JA, Prager RL, Abernathy J, Martinez EA, Salas E, Seifert PC et al (2013) Patient safety in the cardiac operating room: Human factors and teamwork a scientific statement from the american heart association. Circulation 128(10):1139–1169
Ahmad N, Hussein AA, Cavuoto L, Sharif M, Allers JC, Hinata N et al (2016) Ambulatory movements, team dynamics and interactions during robot-assisted surgery. BJU Int 118(1):132–139. https://doi.org/10.1111/bju.13426
Bayramzadeh S, Joseph A, Allison D, Shultz J, Abernathy J, Group ROS (2018) Using an integrative mock-up simulation approach for evidence-based evaluation of operating room design prototypes. Applied Ergonomics 70:288–299
Neyens DM, Bayramzadeh S, Catchpole K, Joseph A, Taaffe K, Jurewicz K et al (2019) Using a systems approach to evaluate a circulating nurse’s work patterns and workflow disruptions. Appl Ergon 78:293–300
Jurewicz KA, Neyens DM, Catchpole K, Joseph A, Reeves ST, Abernathy JH 3rd (2021) Observational study of anaesthesia workflow to evaluate physical workspace design and layout. Br J Anaesth 126(3):633–641. https://doi.org/10.1016/j.bja.2020.08.063
Lee K (2015) Designing the OR of the future. Healthcare Design Magazine (September). Accessed June 2022. Retrieved from https://www.healthcaredesignmagazine.com/trends/construction-engineering/designing-or-future/
Thiele RH, Huffmyer JL, Nemergut EC (2008) The “six sigma approach” to the operating room environment and infection. Best Pract Res Clin Anaesthesiol 22(3):537–552
Cohen T, Cabrera J, Sisk O, Welsh K, Abernathy J, Reeves S et al (2016) Identifying workflow disruptions in the cardiovascular operating room. Anaesthesia 71(8):948–954. https://doi.org/10.1111/anae.13521
Bayramzadeh S, Joseph A, San D, Khoshkenar A, Taaffe K, Jafarifiroozabadi R et al (2018) The impact of operating room layout on circulating nurse’s work patterns and flow disruptions: A behavioral mapping study. HERD 11(3):124–138. https://doi.org/10.1177/1937586717751124
Taaffe K, Joseph A, Khoshkenar A, Machry H, Allison D, Reeves ST et al (2021) Proactive evaluation of an operating room prototype: A simulation-based modeling approach. J Patient Saf 17(8):e1833–e1839. https://doi.org/10.1097/pts.0000000000000693
Brailsford SC, Eldabi T, Kunc M, Mustafee N, Osorio AF (2019) Hybrid simulation modelling in operational research: A state-of-the-art review. Eur J Oper Res 278(3):721–737. https://doi.org/10.1016/j.ejor.2018.10.025
Kim D-H, Juhn J-H (1997) System dynamics as a modeling platform for multi-agent systems. Paper presented at the The 15th International Conference of the System Dynamics Society
Schieritz, N., & GroBler, A. (2003, 6-9 Jan. 2003). Emergent structures in supply chains - a study integrating agent-based and system dynamics modeling. Paper presented at the 36th Annual Hawaii International Conference on System Sciences
Sevkli M, Lenny Koh SC, Zaim S, Demirbag M, Tatoglu E (2008) Hybrid analytical hierarchy process model for supplier selection. Ind Manag Data Syst 108(1):122–142. https://doi.org/10.1108/02635570810844124
Chahal K, Eldabi T (2008, 7–10 Dec. 2008) Applicability of hybrid simulation to different modes of governance in uk healthcare. Paper presented at the 2008 Winter Simulation Conference
Santos VHd, Kotiadis K, Scaparra MP (2020, 14–18 Dec. 2020) A review of hybrid simulation in healthcare. Paper presented at the 2020 Winter Simulation Conference (WSC)
Barach PR, Rostenberg B (2015) Design of cardiac surgery operating rooms and the impact of the built environment. In: Barach PR, Jacobs JP, Lipshultz SE, Laussen PC (eds) Pediatric and congenital cardiac care: Volume 2: Quality improvement and patient safety, vol 2. Springer, London, London, pp 411–424
Gerbrands A, Albayrak A, Kazemier G (2004) Ergonomic evaluation of the work area of the scrub nurse. Minim Invasive Ther Allied Technol 13(3):142–146
Helbing D, Molnár P (1995) Social force model for pedestrian dynamics. Phys Rev E 51(5):4282–4286. https://doi.org/10.1103/physreve.51.4282
Alanis R, Ingolfsson A, Kolfal B (2013) A markov chain model for an ems system with repositioning. Prod Oper Manag 22(1):216–231. https://doi.org/10.1111/j.1937-5956.2012.01362.x
Budge S, Ingolfsson A, Erkut E (2009) Technical note—approximating vehicle dispatch probabilities for emergency service systems with location-specific service times and multiple units per location. Oper Res 57(1):251–255. https://doi.org/10.1287/opre.1080.0591
Sastry S, Culler D, Howard M, Roosta T, Zhu B, Taneja J, et al. (2006, 15–19 May 2006) Instrumenting wireless sensor networks for real-time surveillance. Paper presented at the Proceedings 2006 IEEE International Conference on Robotics and Automation, 2006. ICRA 2006.
Shah RC, Roy S, Jain S, Brunette W (2003, 11–11 May 2003) Data mules: Modeling a three-tier architecture for sparse sensor networks. Paper presented at the Proceedings of the First IEEE International Workshop on Sensor Network Protocols and Applications, 2003.
Levinson D, Chen W (2005) Paving new ground: A markov chain model of the change in transportation networks and land use. In: David ML, Kevin JK (eds) Access to destinations. Emerald Group Publishing Limited, pp 243–266
Yu G, Hu J, Zhang C, Zhuang L, Song J (2003) Short-term traffic flow forecasting based on markov chain model. Paper presented at the Intelligent Vehicles Symposium
Howell DC (2013) Statistical methods for psychology, 8th edn. Wadsworth Cengage Learning, Belmont, CA
Fox J (2016) Applied regression analysis and generalized linear models, 3 edn. SAGE Publications, 816pp
Rosopa PJ, Schaffer MM, Schroeder AN (2013) Managing heteroscedasticity in general linear models. Psychol Methods 18(3):335–351. https://doi.org/10.1037/a0032553
Young RS, O’Regan DJ (2010) Cardiac surgical theatre traffic: Time for traffic calming measures? Interact Cardiovasc Thorac Surg 10(4):526–529
McCalman J, Paton R, Siebert S (2016) Change management: A guide to effective implementation, 4th edn. Sage Publications, 288pp
Acknowledgements
The authors would like to thank the RIPCHD.OR Study Group for their contribution to the work supporting the effort in this study.
Funding
Research was supported by the Agency for Healthcare Research and Quality [grant number P30HS0O24380, 2015], as well as the Harriet and Jerry Dempsey Professorship in Industrial Engineering at Clemson University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This research received IRB approval from the Medical University of South Carolina.
Conflicts of interest/Competing interests
The authors have no relevant financial or non-financial interests to disclose.
The authors have no conflicts of interest to declare that are relevant to the content of this article.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
The authors have no financial or proprietary interests in any material discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix 1: Table 6
Appendix 2: Zone Visits Selection Procedure
-
Step 1 – Remove zone visits with short durations:
Starting with the full dataset of zone visits, discard all entries where the zone visit is less than 15 seconds, as this is a pass-through visit only. This will avoid considering such visits as destinations in the final path, since there was no sustained activity observed there in the video recordings.
-
Step 2 – Remove transient zone visits:
Discard all remaining transitional and doorway zone visits from the travel path of a subject since these cannot be conceptually considered destination zones. The associated duration of these zone visits is assigned to the nearest functional zone (distances are measured between the central points of two zones). The video recordings of the 23 procedures indicate that the occurrence of activities in these zones is low, and a reassignment of activity greater than 15 seconds occurred less than 6% of the time. (This reduced the zone count from 19 to 13 zones, each contained in at least one group in the next step.)
-
Step 3a – Aggregate zones into zone groups:
Based on proximity and functionality, identify zone groups where an opportunity exists to select a single zone to represent activity. These zone groupings do not need to be mutually exclusive. The zone groups identified for the OR in Figure 1 are:
-
Group 1.CN Workstation, Support Zone 1, Support Zone 5
-
Group 2.Support Zone 2, Supply Zone 1, Support Zone 3
-
Group 3.Supply Zone 2, Surgeon Workstation, Anesthesia Workstation
-
Group 4.Surgical Table 1, Foot of Table
-
Group 5.Surgical Table 2, Foot of Table, Anesthesia Workstation
-
Group 6.Supply Zone 2, Support Zone 3, Anesthesia Workstation
-
Step 3b – Aggregate zone visits within zone groups:
For each subset of consecutive zone visits within a zone group, identify and denote the zone visit with the longest duration as the destination zone. All durations of the other zone visits of the subset are assigned to the destination zone, and the zone visits are removed from the dataset.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Taaffe, K., Ferrand, Y.B., Khoshkenar, A. et al. Operating room design using agent-based simulation to reduce room obstructions. Health Care Manag Sci 26, 261–278 (2023). https://doi.org/10.1007/s10729-022-09622-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-022-09622-3