Abstract
Orthostatic hypotension (OH) is associated with increased total mortality but contribution of specific death causes has not been thoroughly explored. In this prospective study, authors followed up 32,068 individuals without baseline history of cancer or cardiovascular disease (69% men; mean age, 46 years; range, 26–61 years) over a period of 24 years. Hazard ratios (HRs) for total and cause-specific mortality associated with presence of OH and by quartiles of postural systolic blood pressure response (∆SBP) were assessed using multivariate adjusted Cox regression model. A total of 7,145 deaths (22.3%, 9.4 deaths/1,000 person-years) occurred during follow-up. Those with OH (n = 1,943) had higher risk of death due to injury (HR, 1.88; 1.37–2.57) and neurological disease (HR, 2.21; 1.39–3.51). Analogically, risk of death caused by injury and neurological disease increased across the quartiles of ∆SBP from hyper- (Q1SBP, +8.5 ± 4.7 mmHg) to hypotensive response (Q4SBP, −13.7 ± 5.7 mmHg; HR, 1.32; 1.00–1.72, and 1.84; 1.20–2.82, respectively) as did also risk of death due to respiratory disease (Q4SBP vs. Q1SBP: HR, 1.53; 1.14–2.04). In contrast, risk curve for cerebrovascular death was U-shaped with nadir in the mildly hypotensive 3rd quartile of ∆SBP (−5.0 ± 0.1 mmHg, Q3SBP vs. Q1SBP: HR, 0.75; 0.54–1.03; P for linear trend = 0.021). Additionally, cardiovascular mortality was increased among 5,805 rescreened participants (mean age, 53 years; 9.8% OH positive: HR, 1.54; 1.24–1.89, and Q4SBP vs. Q1SBP: 1.27; 1.02–1.57, respectively). In summary, increased mortality predicted by blood pressure fall on standing is associated with injuries, neurodegenerative, and respiratory diseases, as well as with cardiovascular disease in older adults. Moreover, both increase and pronounced decrease of SBP during early orthostasis indicate higher risk of cerebrovascular death.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orthostatic hypotension (OH), a relatively common manifestation of autonomic dysfunction [1–3], has been linked to increased mortality in general population [4–8]. Although it seems indisputable that OH is associated with higher all-cause mortality, specific causes of death have been only partially studied. In particular, Rose et al. [6] noticed that OH predicted both higher cardiovascular and non-cardiovascular mortality, but not cancer-related one. However, other causes of the twofold increased mortality were not explored. In parallel, authors reported that younger (<42 years) compared to older individuals with OH demonstrated a higher all-cause mortality risk, but the risk of incident coronary event and stroke was not increased in this subset of population [8].
Previous epidemiological studies concentrated mainly upon OH as a pronounced and well-defined variant of the hypotensive postural blood pressure response [9]. Meanwhile, it is still unknown which mortality pattern is followed by other types of orthostatic responses: mildly hypotensive, neutral and hypertensive. Consequently, authors decided to study specific causes of death among those with and without OH, as well as in the subsets of different postural blood pressure responses within a large middle-aged Swedish population.
Methods
Study population
The Malmö Preventive Project (MPP) is a population-based prospective cohort study in the city of Malmö, in southern Sweden [10]. The primary aim of the project was to invite large strata of the adult population to screening for cardiovascular disease (CVD). A total of 33,346 (22,444 men and 10,902 women; mean age, 45 years; range, 26–61 years) inhabitants of Malmö, born between 1921 and 1948, were examined between 1974 and 1992. The overall attendance rate was 71% (range for examined age cohorts, 64–78%) [11]. In the present study we excluded 549 participants because of missing blood pressure values, eight outliers (difference between systolic or diastolic blood pressure in supine and standing position of more than 80 mmHg), and all individuals with baseline history of CVD (myocardial infarction or stroke, n = 159) or cancer (n = 562). Thus, the study population consisted of 32,068 individuals (22,130 men and 9,938 women). An overall study design is presented in Fig. 1.
Baseline examination
The mailed invitation contained instructions to abstain from food, alcohol and tobacco for 12 h prior to the examination, which was performed by trained nurses in the morning. Participants were, however, allowed to drink water ad libitum. Blood pressure was measured using the auscultatory method with a mercury sphygmomanometer and an appropriately sized cuff placed around the right arm supported at the level of the heart. The first blood pressure reading was taken twice after 10 min rest in the supine position. Then, the participants were asked to stand up and the second blood pressure measurement was taken twice in the standing position between 1 and 3 min of standing. The mean value of two readings was recorded for each position and rounded to nearest 5 mmHg. The body-mass index (BMI) was calculated as weight in kg divided by height squared in meters. Blood samples were collected from the antecubital vain and analyzed by standard methods at the Department of Clinical Chemistry, Malmö University Hospital. At the end, the participants were asked to fill in a self-administered questionnaire focused on personal and familiar history of CVD, hypertension, diabetes, cancer, smoking habits, and lifestyle patterns. The following questions were relevant to the history of myocardial infarction, stroke, and cancer, if the answer was yes: “Have you ever been hospitalized for myocardial infarction/stroke?” or “Have you ever had/do you have cancer?” Antihypertensive treatment was defined as a positive answer to the following question: “Do you take medication for high blood pressure?”, but data on particular types of antihypertensive agents were not collected. Those who confirmed regular or occasional current smoking were classified as smokers. Alcohol intake was dichotomized by drinking behavior (problematic, non-problematic), and socioeconomic status was divided into low (manual worker) and high (non-manual worker) according to previously applied method [12]. A detailed description of recruitment and screening procedures may be found elsewhere [10, 13]. The health service authority of Malmö approved and funded the screening program. All participants gave informed consent.
Definitions of clinical characteristics
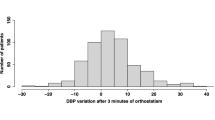
OH was defined according to the international consensus criteria as a decrease in systolic blood pressure (SBP) ≥20 mm Hg and/or decrease in diastolic blood pressure (DBP) ≥10 mm Hg within three minutes of standing [14].
Orthostatic (postural) SBP response (ΔSBP) was defined as standing SBP—supine SBP. Diabetes was defined as fasting plasma glucose ≥7.0 mmol/l, or current pharmacological treatment of diabetes, or self-reported history of diabetes [15].
Retrieval of end-points
All study participants were followed from the baseline examination until the death, emigration from Sweden, or 31 December 2006. Authors applied linkage of the unique 10-digit personal identification number with the Swedish National Cause of Death Register. The primary diagnosis retrieved from the register was considered valid for the specific cause of death as applied in previous studies [13, 16]. The International Classification of Diseases (ICD)-8 codes were converted to ICD-9 codes, if applicable. The causes of deaths were classified into CVD (ICD-9 codes 390–459, ICD-10; I00–I99), cancer (ICD-9 codes 140–239, ICD-10; C00–C99), injury (ICD-9 codes 800–999, ICD-10; V, W, X, Y), respiratory diseases (ICD-9 codes 460–519, ICD-10; J), digestive system diseases (ICD-9 codes 520–579, ICD-10; K), neurological diseases (ICD-9 codes 320–389, ICD-10; G, H), and other causes of death. Death due to ischemic heart disease was defined as 410–414 or I20–I22 according to ICD-9 and ICD-10, whereas death due to cerebrovascular disease as 430–438, or I60–I69, respectively.
Those who emigrated from Sweden before 31 December 2006, and had been event-free at the time of emigration (n = 624, 1.9%), were censored at the date of emigration. The mean follow-up time was 23.5 ± 6.2 years.
Statistical analysis
The relationship between OH, quartiles of ∆SBP and all-cause mortality was assessed by the Kaplan–Meier method and the log-rank test. The hazards risks for total and cause-specific mortality according to OH status, or, alternatively, by quartiles of ∆SBP were investigated using Cox proportional hazards models. The proportional hazards assumption was assessed graphically in a univariate model. Two Cox regression models were applied: a basic Model 1 adjusted for age and gender, and a more comprehensive Model 2 adjusted additionally for traditional risk factors for OH and mortality: BMI, SBP, resting heart rate, antihypertensive treatment, diabetes, total cholesterol and current smoking [8]. In Model 2, authors excluded individuals with missing data on BMI (n = 5) and total cholesterol (n = 58). In additional adjustment, alcohol intake and socioeconomic status were entered into the Model 2, and analyses were repeated. Those with the unspecified socioeconomic status were excluded (n = 2,512), of these 10.4% were OH positive. Finally, authors performed Cox regression analysis according to Model 1 and 2 on a subset of MPP cohort (n = 6,109), which was rescreened after approximately 6 years from baseline, including orthostatic BP measurements (Fig. 1).
Potential interactions between OH and age or gender on cause-specific mortality were evaluated by including interaction terms in the multivariate model. All analyses were performed using SPSS statistical software version 17.0 for Windows (SPSS Inc., Chicago, IL). All tests were two-sided whereby P < 0.05 was considered statistically significant for non-interaction terms, and P < 0.10 for interaction terms.
Results
Out of 32,068 individuals included in the present study, 1,943 (6.1%) met the diagnostic criteria of OH at baseline, whereas 570 among 5,805 participants (9.8%) were found to have OH during rescreening program. The baseline characteristics of MPP cohort and the rescreened subset of study population according to OH status were published previously [8, 17]. As can be seen in Table 1, nearly one third of study participants (Q2SBP, n = 10,123) demonstrated a neutral orthostatic SBP response (i.e. no difference between supine and standing SBP), which resulted in a disproportional partition of study sample into quartiles. Those with hypotensive response (Q4SBP) were older, had higher SBP and DBP, and higher proportions of women, patients with diabetes and of those receiving antihypertensive treatment. Figure 2 illustrates the cumulative all-cause mortality during follow-up by quartiles of ∆SBP. The Kaplan–Meier curves for the total mortality by OH status corresponded to authors’ previous publication [8] and were not shown (log-rank test, P ≤ 0.001 for both). As can be seen in Table 2, total mortality and mortality rate were higher among those with as compared to those without OH (14.1 vs. 9.1 deaths per 1,000 person-years). A similar trend was observed across the quartiles of ∆SBP (Q1SBP vs. Q4SBP: 8.1 vs. 12.3 deaths per 1,000 person-years). As shown in Table 3, OH was predictive of four specific causes of death in the Cox regression analysis according to Model 1: CVD, injuries, respiratory and neurological diseases. However, after further adjustment for traditional risk factors (Model 2), only death due to injury and neurological disease (in 16/20 cases diagnosed as neurodegenerative disease) were predicted by OH. There were two potential interactions between OH and age: on death due to cancer (P = 0.001) and neurological disease (P = 0.082). In a subgroup analysis authors found that cancer-related mortality was significantly increased in the youngest stratum of study population (<42 years, n = 9,357; HR, 1.66; 95% CI: 1.03–2.69, P = 0.039), whereas risk of death due to neurological disease was highest among the oldest study participants (>48 years, n = 11,830; HR, 2.87, 95% CI: 1.64–5.08, P < 0.001). There was no potential interaction between OH and gender.
The main mortality trends found among those with OH were confirmed by stratification of study participants according to quartiles of postural BP response. As presented in Table 4, subset of population characterized by a pronounced hypotensive response (Q4SBP, −13.7 ± 5.7 mmHg) had highest total mortality (HR, 1.13; 95% CI: 1.06–1.21). Risk of death caused by both injury and neurological disease increased across the quartiles of ∆SBP, being for the latter and for Q4SBP similar to that observed among OH positive individuals (HR, 1.84; 95% CI: 1.20–2.82 vs. 2.21; 1.39–3.51, respectively). In contrast, those with hypertensive BP response (Q1SBP, +8.5 ± 4.7 mmHg) had significantly lower risk of death due to respiratory disease (mainly represented by chronic obstructive pulmonary disease) as compared to the other quartiles of ∆SBP (Q4SBP vs. Q1SBP: HR, 1.53; 95% CI: 1.14–2.04). Moreover, authors noted a U-shaped risk curve for cerebrovascular death with a nadir in the 3rd quartile of ∆SBP (Q3SBP, −5.0 ± 0.1 mmHg; HR, 0.75; 95% CI: 0.54–1.03; P for linear trend = 0.021). There was one potential interaction between quartiles of ∆SBP and age: on cancer-related mortality (P = 0.031). In a subgroup analysis, the pronounced hypotensive response was predictive of cancer-related mortality within the middle age stratum (42–48 years, n = 10,881, Q4SBP vs. Q1SBP: HR, 1.25; 95% CI: 1.04–1.49; P for linear trend 0.067), whereas among youngest study participants (≤42 years) the highest risk was observed in the 3rd but not 4th quartile (Q3SBP vs. Q1SBP: HR, 1.23; 95% CI: 0.91–1.67, and Q4SBP vs. Q1SBP: HR, 0.96; 95% CI: 0.67–1.39; P for linear trend 0.69).
Additional adjustments for socioeconomic status and alcohol intake did not change the main results and only slightly attenuated mortality risk associated with OH (injuries, HR: 1.74; 95% CI: 1.20–2.53; neurological, 2.00, 1.18–3.36), and Q4SBP (injuries, HR: 1.21; 95% CI: 0.89–1.64; neurological, 1.68; 1.05–2.69, respiratory, 1.46; 1.05–2.04).
As shown in Table 5, results obtained from the subsidiary analysis on the rescreened subset of MPP cohort were essentially consistent with the main findings. However, the relative mortality risk conferred by presence of hypotensive response at rescreening (i.e. OH positive or Q4SBP) was in general higher than that at baseline, both for all and specific causes of death. Furthermore, the hypotensive response at rescreening independently predicted higher cardiovascular mortality, in contrast to the baseline status (OH positive, HR, 1.54; 95% CI: 1.24–1.89; P ≤ 0.001, and Q4SBP vs. Q1SBP: HR, 1.27; 95% CI: 1.02–1.57, P for linear trend = 0.021, respectively).
Discussion
Orthostatic haemodynamic impairment is generally regarded as a troublesome clinical condition, especially in elderly, chronically ill, neurological, and polymorbid patients [18–20], and surprisingly little is known about its prevalence and consequences in general population. In particular, association between OH and the cause-specific mortality remains largely unexplored. To our knowledge, this is the first study to report that injuries and neurological diseases may be etiologically related to the increased mortality among middle-aged individuals with often asymptomatic OH. Moreover, a statistical evidence could be also demonstrated for respiratory diseases (for the quartile with the most pronounced hypotensive SBP response) and cancer (in younger individuals aged <48 years). The main findings are discussed below in regard to specific diagnostic categories:
Cardiovascular disease
The association between prevalent OH and long-term mortality due to CVD (or ischemic heart disease only), reported previously by other authors in the ARIC cohort [6], was remarkably attenuated after adjustment for conventional risk factors. These results were most probably an effect of a strong correlation between OH and CV risk factors, which in turn predict increased mortality mediated by CVD. Except for total cholesterol, all other covariates entered into the more comprehensive model are known to be independent determinants of both OH [8] and cardiovascular morbidity, such as myocardial infarction and stroke [21, 22]. Taking into account conventional risk factors might thus efficiently explain why individuals with OH were prematurely affected by CVD and died. However, in the rescreened subset of study population, characterized by similar mean age as that in the ARIC cohort (53 vs. 54 years) the hypotensive orthostatic response was independently predictive of cardiovascular mortality. Consequently, presence of impaired orthostatic BP response in a more advanced age may be a stronger cardiovascular risk factor than the same phenomenon among relatively younger individuals.
Another important finding in this diagnostic group was a trend toward U-shaped curve for quartiles of ∆SBP and cerebrovascular mortality, in concordance with previous reports [23, 24]. Thus, a neutral or a slightly hypotensive SBP response during orthostatic challenge may play a protective role against cerebrovascular lesion.
Injuries
One of the most consistent findings in this study was the relationship between OH and injury-related deaths. Haemodynamic impairment during orthostasis is a well-known risk factor of traumatic falls among neurologically ill and elderly patients [2, 25]. The mean age of the studied population was, however, only about 45 years. We propose that some of injuries were provoked by a temporary impairment of the cerebral circulation when the haemodynamic reserve between minimal BP needed for maintenance of cerebral perfusion (usually SBP ≥ 60–70 mm Hg) [26] and the actual value of BP was compressed by the orthostatic drop. Some patients with asymptomatic impairment of orthostatic BP regulation may not be aware of the problem until the first episode of sudden onset dizziness or syncope occurs. Interestingly, the best predictor of injury-related death was the standard OH definition, which suggests that the magnitude of BP fall is a crucial factor behind this association.
Neurological diseases
Neurological etiology was found to be another factor associated with increased mortality in individuals with OH and a pronounced postural decrease of SBP (Q4SBP). This finding is not at all surprising taking into account a strong etiological relationship between OH and neurodegenerative diseases, such as Parkinson’s disease and primary autonomic failure [27]. Thus, in some participants, subclinical neurodegenerative process may have already been present at baseline and the orthostatic challenge was sensitive enough to detect the accompanying autonomic dysfunction. Notably, the risk of fatal neurological disease was higher among older participants (≥48 years), and in the rescreened subset of cohort, confirming that postural BP drop is more often related to neurogenic OH with advancing older [28].
Respiratory diseases
Association between postural BP response and mortality due to a respiratory disease (mainly chronic obstructive pulmonary disease, COPD) was a surprising finding. We know that smoking is associated with OH [8]. However, after adjustment for current smoking the predictive role of postural SBP and MAP response remained statistically significant. These results suggest that autonomic dysfunction is associated with a higher risk of developing terminal lung disease. Among the proposed predictors of increased mortality in COPD there are no parameters that can be directly linked to OH or autonomic dysfunction [29]. On the other hand, some authors claim that spirometry alone is not a good predictor of mortality in COPD, and other parameters, such as low BMI, dyspnoea, and exercise capacity are often included in the mortality risk score systems [30]. Interestingly, low BMI is also an independent determinant of OH [8]. Moreover, in patients with COPD, cardiac autonomic dysfunction (reduced heart rate variability) was found to be correlated with lower BMI, reduced level of physical activity in daily life, and impairment of respiratory and peripheral muscle condition [31]. In orthostatic blood pressure dysregulation a similar pattern has been observed: a sympathetic hyperactivity associated with reduced variability of the parasympathetic nervous system [32]. Thus, the common pathway for the orthostatic blood pressure drop and increased risk of respiratory-related mortality might be a chronically altered autonomic function signaled by lower BMI, worse exercise tolerance, and more subtle markers, such as reduced heart rate variability. Unfortunately, given the available cohort data, authors were not able to confirm this hypothesis.
Cancer
The relevance of the association between cancer-related mortality and hypotensive BP response in younger adults is unclear and might suggest that haemodynamic postural impairment (and subclinical autonomic disorders), if acting long enough, can favor carcinogenesis through unspecified biologically active substances, whose plasma or tissue activity is altered by a chronically increased sympathetic tonus and reduced parasympathetic reactivity. However, such hypothesis would require further studies to be confirmed.
Strengths and limitations of the study
Strength of this study lies in a large number and similar ethnic background of the studied cohort, long follow-up, and access to an end-point register with a high case ascertainment. The main limitation is the fact that standing blood pressure was recorded between the 1st and 3rd min after assuming an upright position and we may have, therefore, missed those with initial (<1 min) [33] and delayed (>3 min) orthostatic hypotension [34]. Moreover, OH was assessed in the whole cohort only once between baseline and end-point.
Conclusions
Among middle-aged individuals the increased risk of mortality independently conferred by impairment of orthostatic blood pressure regulation is associated with injuries, neurodegenerative, and respiratory diseases. Furthermore, both increase and pronounced decrease of systolic blood pressure during early orthostasis indicate a higher risk of death due to cerebrovascular disease, whereas blood pressure decrease on standing in the advanced age seems to be also an independent predictor of higher cardiovascular mortality.
Abbreviations
- OH:
-
Orthostatic hypotension
- MPP:
-
Malmö Preventive Project
- CVD:
-
Cardiovascular disease
- BMI:
-
Body-mass index
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- ICD:
-
International Classification of Diseases
- IHD:
-
Ischaemic heart disease
- COPD:
-
Chronic obstructive pulmonary disease
References
Goldstein DS, Robertson D, Esler M, Straus SE, Eisenhofer G. Dysautonomias: clinical disorders of the autonomic nervous system. Ann Intern Med. 2002;137:753–63.
Goldstein DS, Sharabi Y. Neurogenic orthostatic hypotension: a pathophysiological approach. Circulation. 2009;119:139–46.
Mansoor GA. Orthostatic hypotension due to autonomic disorders in the hypertension clinic. Am J Hypertens. 2006;19:319–26.
Masaki KH, Schatz IJ, Burchfiel CM, Sharp DS, Chiu D, Foley D, et al. Orthostatic hypotension predicts mortality in elderly men: the Honolulu Heart Program. Circulation. 1998;98:2290–5.
Luukinen H, Koski K, Laippala P, Kivela SL. Prognosis of diastolic and systolic orthostatic hypotension in older persons. Arch Intern Med. 1999;159:273–80.
Rose KM, Eigenbrodt ML, Biga RL, Couper DJ, Light KC, Sharrett AR, et al. Orthostatic hypotension predicts mortality in middle-aged adults: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2006;114:630–6.
Verwoert GC, Mattace-Raso FU, Hofman A, Heeringa J, Stricker BH, Breteler MM, et al. Orthostatic hypotension and risk of cardiovascular disease in elderly people: the Rotterdam study. J Am Geriatr Soc. 2008;56:1816–20.
Fedorowski A, Stavenow L, Hedblad B, Berglund G, Nilsson PM, Melander O. Orthostatic hypotension predicts all-cause mortality and coronary events in middle-aged individuals (The Malmo Preventive Project). Eur Heart J. 2010;31:85–91.
Benvenuto LJ, Krakoff LR. Morbidity and mortality of orthostatic hypotension: implications for management of cardiovascular disease. Am J Hypertens. 2011;24:135–44.
Trell E. Community-based preventive medical department for individual risk factor assessment and intervention in an urban population. Prev Med. 1983;12:397–402.
Nilsson P, Berglund G. Prevention of cardiovascular disease and diabetes: lessons from the Malmo Preventive Project. J Intern Med. 2000;248:455–62.
Hedblad B, Jonsson S, Nilsson P, Engstrom G, Berglund G, Janzon L. Obesity and myocardial infarction—vulnerability related to occupational level and marital status. A 23-year follow-up of an urban male Swedish population. J Intern Med. 2002;252:542–50.
Berglund G, Nilsson P, Eriksson KF, Nilsson JA, Hedblad B, Kristenson H, et al. Long-term outcome of the Malmo preventive project: mortality and cardiovascular morbidity. J Intern Med. 2000;247:19–29.
The definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. J Auton Nerv Syst. 1996;58:123–4.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53.
Seshasai SR, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364:829–41.
Fedorowski A, Stavenow L, Hedblad B, Berglund G, Nilsson PM, Melander O. Consequences of orthostatic blood pressure variability in middle-aged men (The Malmo Preventive Project). J Hypertens. 2010;28:551–9.
Gupta V, Lipsitz LA. Orthostatic hypotension in the elderly: diagnosis and treatment. Am J Med. 2007;120:841–7.
Low PA, Singer W. Management of neurogenic orthostatic hypotension: an update. Lancet Neurol. 2008;7:451–8.
Maule S, Papotti G, Naso D, Magnino C, Testa E, Veglio F. Orthostatic hypotension: evaluation and treatment. Cardiovasc Hematol Disord Drug Targets. 2007;7:63–70.
Khot UN, Khot MB, Bajzer CT, Sapp SK, Ohman EM, Brener SJ, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898–904.
Allen CL, Bayraktutan U. Risk factors for ischaemic stroke. Int J Stroke. 2008;3:105–16.
Kario K, Eguchi K, Hoshide S, Hoshide Y, Umeda Y, Mitsuhashi T, et al. U-curve relationship between orthostatic blood pressure change and silent cerebrovascular disease in elderly hypertensives: orthostatic hypertension as a new cardiovascular risk factor. J Am Coll Cardiol. 2002;40:133–41.
Yatsuya H, Folsom AR, Alonso A, Gottesman RF, Rose KM. Postural changes in blood pressure and incidence of ischemic stroke subtypes: the ARIC study. Hypertension. 2011;57:167–73.
Chang NT, Yang NP, Chou P. Incidence, risk factors and consequences of falling injuries among the community-dwelling elderly in Shihpai, Taiwan. Aging Clin Exp Res. 2010;22:70–7.
van Beek AH, Claassen JA, Rikkert MG, Jansen RW. Cerebral autoregulation: an overview of current concepts and methodology with special focus on the elderly. J Cereb Blood Flow Metab. 2008;28:1071–85.
Freeman R. Clinical practice. Neurogenic orthostatic hypotension. N Engl J Med. 2008;358:615–24.
Low PA. Prevalence of orthostatic hypotension. Clin Auton Res. 2008;18(Suppl 1):8–13.
Puhan MA, Garcia-Aymerich J, Frey M, ter Riet G, Anto JM, Agusti AG, et al. Expansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO index. Lancet. 2009;374:704–11.
Celli BR, Cote CG, Lareau SC, Meek PM. Predictors of survival in COPD: more than just the FEV1. Respir Med. 2008;102(Suppl 1):S27–35.
Camillo CA, Pitta F, Possani HV, Barbosa MV, Marques DS, Cavalheri V, et al. Heart rate variability and disease characteristics in patients with COPD. Lung. 2008;186:393–401.
Sato Y, Ichihashi K, Kikuchi Y, Shiraishi H, Momoi MY. Autonomic function in adolescents with orthostatic dysregulation measured by heart rate variability. Hypertens Res. 2007;30:601–5.
Wieling W, Krediet CT, van Dijk N, Linzer M, Tschakovsky ME. Initial orthostatic hypotension: review of a forgotten condition. Clin Sci (Lond). 2007;112:157–65.
Gibbons CH, Freeman R. Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology. 2006;67:28–32.
Acknowledgments
This work was supported by grants from the Swedish Medical Research Council, the Swedish Heart and Lung Foundation, the Medical Faculty of Lund University, Skåne University Hospital, the Albert Påhlsson Research Foundation, the Crafoord Foundation, the Ernhold Lundströms Research Foundation, the Region Skåne, the Hulda and Conrad Mossfelt Foundation, the King Gustaf V and Queen Victoria Foundation, the Wallenberg Foundation, and the Lennart Hanssons Memorial Fund.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Fedorowski, A., Hedblad, B. & Melander, O. Early postural blood pressure response and cause-specific mortality among middle-aged adults. Eur J Epidemiol 26, 537–546 (2011). https://doi.org/10.1007/s10654-011-9578-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-011-9578-1