Abstract
Aim
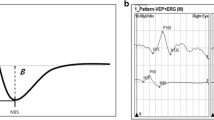
Dysfunction of the retinal ganglion cells (RGC) can be detected by the pattern electroretinogram (PERG) as a reduction of the N95 amplitude, a decrease of the ratio between N95 and P50 amplitude and/or a shortening of P50 peak time. Additionally, the slope from the top of the P50 towards the N95 (P50–N95 slope) is less steep than in control subjects. The aim of the study was to quantitatively evaluate this slope in large field PERGs in controls and patients with RGC dysfunction due to optic neuropathy.
Subjects and methods
Large field (21.6°X27.8°) PERGs and optical coherence tomography (OCT) data from 30 eyes of the 30 patients with different types of clinically confirmed optic neuropathies, and with P50 amplitudes within normal limits and abnormal PERG N95 were retrospectively analysed and compared to 30 healthy eyes of 30 control subjects. The P50-N95 slope was analysed with a linear regression from 50 to 80 ms after the stimulus reversal.
Results
The patients with optic neuropathy exhibited a significant reduction of the N95 amplitude (p < 0.001) and N95/P50 ratio (p < 0.001), the P50 peak time was mildly shorter (p = 0.03). The P50–N95 slope was significantly less steep in eyes with optic neuropathies (− 0.089 ± 0.029 vs. − 0.220 ± 0.041, p < 0.001). Thickness of temporal RNFL and the P50–N95 slope appeared to be the most sensitive and specific parameters for detecting RGC dysfunction (AUC = 1.0).
Conclusions
The slope between the P50 and N95 waves of a large field PERG is considerably less steep in patients with RGC dysfunction and could thus be an efficient biomarker, particularly in the diagnosis of early or borderline cases.






Similar content being viewed by others
References
Bach M, Brigell MG, Hawlina M, Holder GE, Johnson MA, McCulloch DL, Meigen T, Viswanathan S (2013) ISCEV standard for clinical pattern electroretinography (PERG): 2012 update. Doc Ophthalmol 126(1):1–7
Holder GE (2001) The pattern electroretinogram. In: Fishman GA, Birch DG, Holder GE, Brigell MG (eds) Electrophysiologic testing in disorders of the retina, optic nerve, and visual pathway, ophthalmology monograph 2, 2nd edn. The Foundation of the American Academy of Ophthalmology, San Francisco, pp 197–235
Holder GE (2001) The pattern electroretinogram and an integrated approach to visual pathway diagnosis. Prog Retin Eye Res 20:531–561
Robson AG, Nilsson J, Li S, Jalali S, Fulton AB, Tormene AP, Holder GE, Brodie SE (2018) ISCEV guide to visual electrodiagnostic procedures. Doc Ophthalmol 136(1):1–26
Ryan S, Arden GB (1988) Electrophysiological discrimination between retinal and optic nerve disorders. Doc Ophthalmol 68:247–255
Viswanathan S, Frishman LJ, Robson JG (2000) The uniform field and pattern ERG in macaques with experimental glaucoma: removal of spiking activity. Invest Ophthalmol Vis Sci 41:2797–2810
Majander A, Robson AG, João C, Holder GE, Chinnery PF, Moore AT, Votruba M, Stockman A, Yu-Wai-Man P (2017) The pattern of retinal ganglion cell dysfunction in Leber hereditary optic neuropathy. Mitochondrion 36:138–149
Holder GE (1997) The pattern electroretinogram in anterior visual pathway dysfunction and its relationship to the pattern visual evoked potential: a personal clinical review of 743 eyes. Eye 11(6):924–934
Holder GE (1991) The incidence of abnormal pattern electroretinography in optic nerve demyelination. Electroencephalogr Clin Neurophysiol 78:18–26
Froehlich J, Kaufman DI (1993) The pattern electroretinogram: N95 amplitudes in normal subjects and optic neuritis patients. Electroencephalogr Clin Neurophysiol 88:83–91
Almarcegui C, Dolz I, Alejos MV, Fernandez FJ, Valdizan JR, Honrubia FM (2001) Pattern electroretinogram in anterior ischemic optic neuropathy. Rev Neurol 32:18–21
Berninger TA, Heider W (1990) Pattern electroretinograms in optic neuritis during the acute stage and after remission. Graefes Arch Clin Exp Ophthalmol 228:410–414
Holder GE (1987) Significance of abnormal pattern electroretinography in anterior visual pathway dysfunction. Br J Ophthalmol 71:166–171
Parmar DN, Sofat A, Bowman R, Bartlett JR, Holder GE (2000) Prognostic value of the pattern electroretinogram in chiasmal compression. Br J Ophthalmol 84:1024–1026
Ziccardi L, Sadun F, De Negri AM, Barboni P, Savini G, Borrelli E, La Morgia C, Carelli V, Parisi V (2013) Retinal function and neural conduction along the visual pathways in affected and unaffected carriers with Leber’s hereditary optic neuropathy. Investig Ophthalmol Vis Sci 54(10):6893–6901
Holder GE, Votruba M, Carter AC, Bhattacharya SS, Fitzke FW, Moore AT (1999) Electrophysiological findings in dominant optic atrophy (DOA) linking to the OPA1 locus on chromosome 3q 28-qter. Doc Ophthalmol 95:217–228
Jarc-Vidmar M, Tajnik M, Brecelj J, Fakin A, Sustar M, Naji M, Stirn-Kranjc B, Glavač D, Hawlina M (2015) Clinical and electrophysiology findings in Slovene patients with leber hereditary optic neuropathy. Doc Ophthalmol 130(3):179–187
Tekavčič Pompe M, Perovšek D, Šuštar M (2020) Chromatic visual evoked potentials indicate early dysfunction of color processing in young patients with demyelinating disease. Doc Ophthalmol 141(2):157–168
Brecelj J (2014) Visual electrophysiology in the clinical evaluation of optic neuritis, chiasmal tumours, achiasmia, and ocular albinism: an overview. Doc Ophthalmol 129(2):71–84
Hawlina M, Konec B (1992) New noncorneal HK-loop electrode for clinical electroretinography. Doc Ophthalmol 81(2):253–259
Lenassi E, Robson AG, Hawlina M, Holder GE (2012) The value of two-field pattern electroretinogram in routine clinical electrophysiologic practice. Retina 32(3):588–599
Holder GE (2004) Electrophysiological assessment of optic nerve disease. Eye 18(11):1133–1143
Froehlich J, Kaufman DI (1993) The pattern electroretinogram: N95 amplitudes in normal subjects and optic neuritis patients. Electroencephalogr Clin Neurophysiol Evoked Potentials Sect 88(2):83–91
Atilla H, Tekeli O, Örnek K, Batioglu F, Elhan AH, Eryilmaz T (2006) Pattern electroretinography and visual evoked potentials in optic nerve diseases. J Clin Neurosci 13(1):55–59
Sihota R, Sony P, Gupta V, Dada T, Singh R (2006) Diagnostic capability of optical coherence tomography in evaluating the degree of glaucomatous retinal nerve fiber damage. Invest Ophthalmol Vis Sci 47(5):2006–2010
Hood DC, Anderson S, Rouleau J, Wenick AS, Grover LK, Behrens MM, Odel JG, Lee AG, Kardon RH (2008) Retinal nerve fiber structure versus visual field function in patients with ischemic optic neuropathy: a test of a linear model. Ophthalmology 115(5):904–910
Kardon R (2011) The role of the macula OCT scan in neuro-ophthalmology. J Neuroophthalmol 31(4):353–361
Aggarwal D, Tan O, Huang D, Sadun AA (2012) Patterns of ganglion cell complex and nerve fiber layer loss in nonarteritic ischemic optic neuropathy by Fourier-domain optical coherence tomography. Investig Ophthalmol Vis Sci 53(8):4539–4545
Kanamori A, Nakamura M, Yamada Y, Negi A (2012) Longitudinal study of retinal nerve fiber layer thickness and ganglion cell complex in traumatic optic neuropathy. Arch Ophthalmol 130(8):1067–1069
Kupersmith MJ, Garvin MK, Wang JK, Durbin M, Kardon R (2016) Retinal ganglion cell layer thinning within one month of presentation for optic neuritis. Mult Scler J 22(5):641–648
Kupersmith M, Garvin M, Wang JW, Durbin M, Kardon R (2016) Retinal ganglion cell layer thinning within one month of presentation for non-arteritic anterior ischemic optic neuropathy. Investig Ophthalmol Vis Sci 57(8):3588–3593
Britze J, Pihl-Jensen G, Frederiksen JL (2017) Retinal ganglion cell analysis in multiple sclerosis and optic neuritis: a systematic review and meta-analysis. J Neurol 264(9):1837–1853
Park KA, Kim J, Oh SY (2014) Analysis of spectral domain optical coherence tomography measurements in optic neuritis: differences in neuromyelitis optica, multiple sclerosis, isolated optic neuritis and normal healthy controls. Acta Ophthalmol 92(1):e57–65
Miki A, Endo T, Morimoto T, Matsushita K, Fujikado T, Nishida K (2015) Retinal nerve fiber layer and ganglion cell complex thicknesses measured with spectral-domain optical coherence tomography in eyes with no light perception due to nonglaucomatous optic neuropathy. Jpn J Ophthalmol 59(4):230–235
Funding
The study was done within the framework of research programme P3-0333 of Slovenian Research Agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Statement on the welfare of animals
This research did not involve any animal subjects.
Ethical approval
This research received an approval from Slovenian National Medical Ethics Committee (No. 0120-53/2022/4). For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sustar Habjan, M., Brecelj, J. & Hawlina, M. Analysis of the slope between P50 and N95 waves of the large field pattern electroretinogram as an additional indicator of ganglion cell dysfunction. Doc Ophthalmol 147, 77–88 (2023). https://doi.org/10.1007/s10633-023-09937-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-023-09937-8