Abstract
Background
Cirrhosis represents a significant health burden; administrative data provide an important tool for research studies.
Aims
We aimed to understand the validity of current ICD-10 codes compared to previously used ICD-9 codes to identify patients with cirrhosis and its complications.
Methods
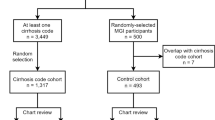
We identified 1981 patients presenting to MUSC between 2013 and 2019 with a diagnosis of cirrhosis. To validate the sensitivity of ICD codes, we reviewed the medical records of 200 patients for each associated ICD 9 and 10 codes. Sensitivity, specificity, and positive predictive value for each ICD code (individually or when combined) were calculated and univariate binary logistic models, for cirrhosis and its complications, predicted probabilities were used to calculate C-statistics.
Results
Single ICD 9 and 10 codes were similarly insensitive for detection of cirrhosis, with sensitivity ranging from 5 to 94%. However, ICD-9 code combinations (when used as either/or) had high sensitivity and specificity for the detection of cirrhosis, with the combination of either 571.5 (or 456.21) or 571.2 codes having a C-statistic of 0.975. Combinations of ICD-10 codes were only slightly less sensitive and specific than ICD-9 codes for detection of cirrhosis (K76.6, or K70.31, plus K74.60 or K74.69, and K70.30 had a C-statistic of 0.927).
Conclusions
ICD-9 and ICD-10 codes when used alone were inaccurate for identifying cirrhosis. ICD-10 and ICD-9 codes had similar performance characteristics. Combinations of ICD codes exhibited the greatest sensitivity and specificity for detection of cirrhosis, and thus should be used to accurately identify cirrhosis.

Similar content being viewed by others
Abbreviations
- AUROC:
-
Area under the receiver operating characteristic
- CT:
-
Computerized tomography
- EHR:
-
Electronic health record
- EGD:
-
Esophagogastroduodenoscopy
- HCC:
-
Hepatocellular carcinoma
- HRS:
-
Hepatorenal syndrome
- ICD:
-
International Classification of Diseases
- MRI:
-
Magnetic resonance imaging
- MUSC:
-
Medical University of South Carolina
- NPV:
-
Negative predictive value
- OASIS:
-
Outcome and assessment information set.
- PPV:
-
Positive predictive value
- SPARC:
-
Services, pricing, and application for research centers
- US:
-
Ultrasonography
- VA:
-
Veterans Affairs
References
Scaglione S, Kliethermes S, Cao G et al. The Epidemiology of Cirrhosis in the United States: A Population-Based Study. Journal of Clinical Gastroenterology. 2015;49:690–696.
Desai AP, Mohan P, Nokes B et al. Increasing Economic Burden in Hospitalized Patients with Cirrhosis: Analysis of a National Database. Clinical and Translational Gastroenterology. 2019;10:e00062.
Quan H, Li B, Saunders LD et al. Assessing Validity of ICD-9-CM and ICD-10 Administrative Data in Recording Clinical Conditions in a Unique Dually Coded Database. Health Serv Res. 2008;43:1424–1441.
Nehra MS, Ma Y, Clark C, Amarasingham R, Rockey DC, Singal AG. Use of Administrative Claims Data for Identifying Patients with Cirrhosis. J Clin Gastroenterol. 2013;47:e50-54.
Mapakshi S, Kramer JR, Richardson P, El-Serag HB, Kanwal F. Positive Predictive Value of International Classification of Diseases, 10th Revision, Codes for Cirrhosis and Its Related Complications. Clin Gastroenterol Hepatol. 2018;16:1677–1678.
Lapointe-Shaw L, Georgie F, Carlone D et al. Identifying Cirrhosis, Decompensated Cirrhosis and Hepatocellular Carcinoma in Health Administrative Data: A Validation Study. PLoS ONE. 2018;13:e0201120.
Lu M, Chacra W, Rabin D et al. Validity of an Automated Algorithm Using Diagnosis and Procedure Codes to Identify Decompensated Cirrhosis Using Electronic Health Records. Clinical Epidemiology. 2017;9:369–376.
Hayward KL, Johnson AL, McKillen BJ et al. ICD-10-AM Codes for Cirrhosis and Related Complications: Key Performance Considerations for Population and Healthcare Studies BMJ Open Gastroenterol. 2020;7.
Wade TD. Traits and Types of Health Data Repositories. Health Inf Sci Syst. 2014;2:4.
Ramrakhiani NS, Le MH, Yeo YH, Le AK, Maeda M, Nguyen MH. Validity of International Classification of Diseases, Tenth Revision, Codes for Cirrhosis. Dig Dis. 2021;39:243–246.
Burkholder DA, Moran IJ, DiBattista JV, Lok AS, Parikh ND, Chen VL. Accuracy of International Classification of Diseases-10 Codes for Cirrhosis and Portal Hypertensive Complications. Dig Dis Sci. 2022;67:3623–3631.
Dahiya M, Eboreime E, Hyde A et al. International Classification of Diseases Codes are Useful in Identifying Cirrhosis in Administrative Databases. Digestive Diseases and Sciences. 2022;67:2107–2122.
Gonzalez JJ, Dziwis J, Patel YA, Tapper EB. Identifying Ascites in Patients with Cirrhosis Using Administrative Codes and Diuretic Use: A Multicenter Study. Digestive Diseases and Sciences. 2022;67:4695–4701.
Haj M, Hart M, Rockey DC. Development of a Novel Clinical Staging Model for Cirrhosis Using the Nationwide Inpatient Sample. J Investig Med. 2018;66:992–997.
Schreiner AD, Zhang J, Durkalski-Mauldin V et al. Advanced Liver Fibrosis and the Metabolic Syndrome in a Primary Care Setting. Diabetes Metab Res Rev. 2021;37:e3452.
Sada Y, Hou J, Richardson P, El-Serag H, Davila J. Validation of Case Finding Algorithms for Hepatocellular Cancer From Administrative Data and Electronic Health Records Using Natural Language Processing. Med Care. 2016;54:e9-14.
Bloom PP, Tapper EB. The Use of Administrative Data to Investigate the Population Burden of Hepatic Encephalopathy. J Clin Med. 2020;9.
Trivedi AN, Grebla RC, Wright SM, Washington DL. Despite Improved Quality of Care in the Veterans Affairs Health System, Racial Disparity Persists for Important Clinical Outcomes. Health Aff (Millwood). 2011;30:707–715.
Jha AK. Learning From the Past to Improve VA Health Care. JAMA. 2016;315:560–561.
Funding
This project was supported, in part, by the National Institutes of Health—the National Institute of Diabetes and Digestive and Kidney Disease (Grant Number P30 DK123704—the clinical component), the National Institute of General Medical Sciences (Grant Number P20 GM 130457—support to DCR), and the National Center for Advancing Translational Sciences of the (Grant Number UL1 TR001450—support to JSO and MG and bioinformatic data gathering).
Author information
Authors and Affiliations
Contributions
AK contributed toward study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content. Email: khalifa@musc.edu. JO contributed toward study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content. Email: jobeid@musc.edu. MG contributed toward analysis and interpretation of data; statistical analysis; critical revision of the manuscript for important intellectual content. Email: gregoski@musc.edu. DR contributed toward study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; supervisory efforts. E-mail: rockey@musc.edu.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khalifa, A., Obeid, J.S., Gregoski, M.J. et al. Accurate Identification of Patients with Cirrhosis and Its Complications in the Electronic Health Record. Dig Dis Sci 68, 2360–2369 (2023). https://doi.org/10.1007/s10620-023-07876-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07876-7