Abstract
Background/Aims
Hemorrhage is a serious complication of endoscopic retrograde cholangiopancreatography (ERCP). However, there is a lack of comparative studies on immediate and delayed hemorrhage. The present study aims to explore the relevant risk factors of immediate and delayed hemorrhage of ERCP and compare the similarities and differences.
Methods
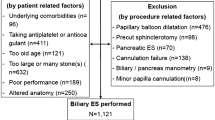
ERCP cases conducted by our hospital between January 2017 and January 2020 were selected for retrospective analysis. Then age, gender, basic disease, laboratory examinations, and other relevant clinical information were collected for the analysis.
Results
A total of 1009 ERCP cases were included in the present study. Among these cases, 76 patients were in the immediate hemorrhage group, 28 patients were in the delayed hemorrhage group, and 905 patients were in the non-hemorrhage group. The univariate analysis revealed that choledocholithiasis, pre-cut, and endoscopic papillary sphincterotomy (EST) were risk factors for immediate hemorrhage, while cholangitis, jaundice, coronary heart disease, pre-cut, high postoperative lipase at four hours and amylase at 24 h, high postoperative leukocyte, urea, bilirubin, low postoperative platelet counts and fibrinogen, and prolonged prothrombin time (PT) and thrombin time (TT) were risk factors for delayed hemorrhage. The logistic regression analysis revealed that EST, pre-cut, and activated partial thromboplastin time (APTT) were independent risk factors for immediate hemorrhage, while high amylase at 24 h after ERCP, high postoperative urea, prolonged TT, and coronary heart disease were independent risk factors for delayed hemorrhage.
Conclusions
Pre-cut was a common risk factor for immediate and delayed hemorrhage, while other risk factors were different.
Similar content being viewed by others
Data availability
The data were collected by checking medical records in the medical management system of Renmin Hospital of Wuhan University. The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
References
Ukkonen M, Siiki A, Antila A, et al. Safety and efficacy of acute endoscopic retrograde cholangiopancreatography in the elderly. Dig Dis Sci. 2016;61:3302–3308. https://doi.org/10.1007/s10620-016-4283-2.
Lu Y, Chen L, Jin Z, Bie LK, Gong B. Is ERCP both effective and safe for common bile duct stones removal in octogenarians? A comparative study. Aging Clin Exp Res. 2016;28:647–652
Salminen P, Lainn S, Gullichsen R. Severe and fatal complications after ERCP: analysis of 2555 procedures in a single experienced center. Surg Endosc. 2008;22:1965–1970
Afridi F, Rotundo L, Feurdean M, Ahlawat S. Trends in post-therapeutic endoscopic retrograde cholangiopancreatography gastrointestinal hemorrhage, perforation and mortality from 2000 to 2012: a nationwide study. Digestion. 2019;2018:1–9
Talukdar R. Complications of ERCP. Best Pract Res Clin Gastroenterol. 2016;30:793–805
Kahaleh M, Freeman M. Prevention and management of post-endoscopic retrograde cholangiopancreatography complications. Clin Endosc. 2012;45:305–312
Ferreira LEVVC, Baron TH. Post-sphincterotomy bleeding: who, what, when, and how. Am J Gastroenterol. 2007;102:2850–2858
Dumonceau JM, Kapral C, Aabakken L, et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2020;52:127–149
Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446–454
Katsinelos P, Lazaraki G, Chatzimavroudis G, et al. Risk factors for therapeutic ERCP-related complications: an analysis of 2715 cases performed by a single endoscopist. Ann Gastroenterol. 2014;27:65–72
Jayaraj M, Mohan BP, Dhindsa BS, et al. Periampullary diverticula and ERCP outcomes: a systematic review and meta-analysis. Dig Dis Sci. 2019;64:1364–1376. https://doi.org/10.1007/s10620-018-5314-y.
Szary NM, Al-Kawas FH. Complications of endoscopic retrograde cholangiopancreatography: how to avoid and manage them. Gastroenterol Hepatol (N Y). 2013;9:496–504
Mallery JS, Baron TH, Dominitz JA, et al. Complications of ERCP. Gastrointest Endosc. 2003;57:633–638
Tsai MC, Wang CC, Wang YT, et al. Major bleeding risk of endoscopic sphincterotomy versus endoscopic papillary balloon dilatation in hemodialysis patients. Saudi J Gastroenterol. 2019;25:106–112
Kim SB, Kim KH, Kim TN. Safety and efficacy of endoscopic retrograde cholangiopancreatography for choledocholithiasis in long-term dialysis: a propensity score analysis. Dig Dis Sci. 2018;63:3141–3146. https://doi.org/10.1007/s10620-018-5112-6.
Inamdar S, Berzin TM, Berkowitz J, et al. Decompensated cirrhosis may be a risk factor for adverse events in endoscopic retrograde cholangiopancreatography. Liver Int. 2016;36:1457–1463
Mashiana HS, Dhaliwal AS, Sayles H, et al. Endoscopic retrograde cholangiopancreatography in cirrhosis—a systematic review and meta-analysis focused on adverse events. World J Gastro Endosc. 2018;10:354–366
Leal C, Prado V, Colan J, et al. Adverse events and acute chronic liver failure in patients with cirrhosis undergoing endoscopic retrograde cholangiopancreatography: a multicenter matched-cohort Study. Am J Gastroenterol. 2019;114:89–97
Navaneethan U, Njei B, Zhu X, et al. Safety of ERCP in patients with liver cirrhosis: a national database study. Endosc Int Open. 2017;5:E303–E314
Adler DG, Haseeb A, Francis G, et al. Efficacy and safety of therapeutic ERCP in patients with cirrhosis: a large multicenter study. Gastrointest Endosc. 2016;83:353–359
Ambrus RB, Svendsen LB, Hillingso JG, Hansen ML, Achiam MP. Post-endoscopic retrograde cholangiopancreaticography complications in liver transplanted patients, a single-center experience. Scand J Surg. 2015;104:86–91
Balderramo D, Bordas JM, Sendino O, et al. Complications after ERCP in liver transplant recipients. Gastrointest Endosc. 2011;74:285–294
Husing A, Cicinnati VR, Maschmeier M, et al. Complications after endoscopic sphincterotomy in liver transplant recipients: a retrospective single-centre study. Arab J Gastroenterol. 2015;16:46–49
Sanna C, Saracco GM, Reggio D, et al. Endoscopic retrograde cholangiopancreatography in patients with biliary complications after orthotopic liver transplantation: outcomes and complications. Transplant Proc. 2009;41:1319–1321
Glomsaker T, Hoff G, Kvaloy JT, et al. Patterns and predictive factors of complications after endoscopic retrograde cholangiopancreatography. Brit J Surg. 2013;100:373–380
Hung TH, Tseng CW, Chen YC, et al. Endoscopic papillary balloon dilation decreases the risk of bleeding in cirrhotic patients compared with endoscopic biliary sphincterotomy: a national population-based study. Medicine (Baltimore). 2019;98:e16529
Navaneethan U, Konjeti R, Lourdusamy V, et al. Precut sphincterotomy: efficacy for ductal access and the risk of adverse events. Gastrointest Endosc. 2015;81:924–931
Kim JH, Yang MJ, Hwang JC, Yoo BM. Usefulness of 4-h post-ERCP serum amylase and lipase levels for prediction of post-ERCP pancreatitis. J Gastroen Hepatol. 2015;30:241–241
Minakari M, Sebghatollahi V, Sattari M, Fahami E. Serum amylase and lipase levels for prediction of postendoscopic retrograde cholangiopancreatography pancreatitis. J Res Med Sci. 2018;23:54
Funding
The authors declare no funding resource in this study.
Author information
Authors and Affiliations
Contributions
XLY, YZ, XYW, and TD were responsible for the preparation and design of the experiment, XLY and YZ were responsible for the collection of data, XYW, XLY, and YZ analyzed the data, TD and XLY jointly completed the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of institutional research committee and with the 1964 Helsinki declaration and its later amendments. For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ye, X., Zhang, Y., Wan, X. et al. Analysis of Risk Factors in Endoscopic Retrograde Cholangiopancreatography-Related Immediate and Delayed Hemorrhage. Dig Dis Sci 66, 4467–4474 (2021). https://doi.org/10.1007/s10620-020-06815-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06815-0