Abstract
Background
Early hospital readmission for patients with cirrhosis continues to challenge the healthcare system. Risk stratification may help tailor resources, but existing models were designed using small, single-institution cohorts or had modest performance.
Aims
We leveraged a large clinical database from the Department of Veterans Affairs (VA) to design a readmission risk model for patients hospitalized with cirrhosis. Additionally, we analyzed potentially modifiable or unexplored readmission risk factors.
Methods
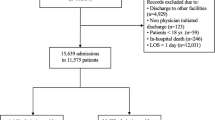
A national VA retrospective cohort of patients with a history of cirrhosis hospitalized for any reason from January 1, 2006, to November 30, 2013, was developed from 123 centers. Using 174 candidate variables within demographics, laboratory results, vital signs, medications, diagnoses and procedures, and healthcare utilization, we built a 47-variable penalized logistic regression model with the outcome of all-cause 30-day readmission. We excluded patients who left against medical advice, transferred to a non-VA facility, or if the hospital length of stay was greater than 30 days. We evaluated calibration and discrimination across variable volume and compared the performance to recalibrated preexisting risk models for readmission.
Results
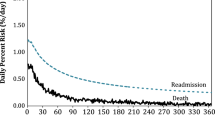
We analyzed 67,749 patients and 179,298 index hospitalizations. The 30-day readmission rate was 23%. Ascites was the most common cirrhosis-related cause of index hospitalization and readmission. The AUC of the model was 0.670 compared to existing models (0.649, 0.566, 0.577). The Brier score of 0.165 showed good calibration.
Conclusion
Our model achieved better discrimination and calibration compared to existing models, even after local recalibration. Assessment of calibration by variable parsimony revealed performance improvements for increasing variable inclusion well beyond those detectable for discrimination.






Similar content being viewed by others
References
Kim WR, Brown RS, Terrault NA, et al. Burden of liver disease in the United States: summary of a workshop. Hepatology. 2002;36:227–242.
Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2011;9:524–530.e1. quiz e60.
Asrani SK, Larson JJ, Yawn B, et al. Underestimation of liver-related mortality in the United States. Gastroenterology. 2013;145:375–382.e1-2.
Schuppan D, Afdhal NH. Liver Cirrhosis. Lancet. 2008;371:838–851.
Everhart JE, Ruhl CE. Burden of digestive diseases in the United States Part III: liver, biliary tract, and pancreas. Gastroenterology. 2009;136:1134–1144.
HCUPnet. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality, Rockville, MD. https://hcupnet.ahrq.gov. Published 2014. Accessed 5.12.2018.
Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143(1179–1187):e3.
Peery AF, Crockett SD, Barritt AS, et al. Burden of gastrointestinal, liver, and pancreatic diseases in the United States. Gastroenterology. 2015;149(1731–1741):e3.
Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2019;156(254–272):e11.
Volk ML. Hospital readmissions for decompensated cirrhosis. Clin Liver Dis. 2014;4:138–140.
Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med. 2000;160:1074–1081.
Halfon P, Eggli Y, Pêtre-Rohrbach I, et al. Validation of the potentially avoidable hospital readmission rate as a routine indicator of the quality of hospital care. Med Care. 2006;44:972–981.
Morales BPP. Early hospital readmission in decompensated cirrhosis: incidence, impact on mortality, and predictive factors. Dig Liver Dis. 2017;49:903–909.
Marchesini G, Bianchi G, Amodio P, et al. Factors associated with poor health-related quality of life of patients with cirrhosis. Gastroenterology. 2001;120:170–178.
Arguedas MR, DeLawrence TG, McGuire BM. Influence of hepatic encephalopathy on health-related quality of life in patients with cirrhosis. Dig Dis Sci. 2003;48:1622–1626.
Rakoski MO, McCammon RJ, Piette JD, et al. Burden of cirrhosis on older Americans and their families: analysis of the health and retirement study. Hepatology. 2012;55:184–191.
Bourne RB, Chesworth BM, Davis AM, et al. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63.
van Walraven C, Bennett C, Jennings A, et al. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183:E391–E402.
Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520.
Ghaoui RF. Outcomes associated with a mandatory gastroenterology consultation to improve the quality of care of patients hospitalized with decompensated cirrhosis. J Hosp Med Online. 2015;10:236–241.
Kanwal FA. Early outpatient follow-up and 30-day outcomes in patients hospitalized with cirrhosis. Hepatology. 2016;64:569–581.
Morando FM. How to improve care in outpatients with cirrhosis and ascites: a new model of care coordination by consultant hepatologists. J Hepatol. 2013;59:257–264.
Kasper EK, Gerstenblith G, Hefter G, et al. A randomized trial of the efficacy of multidisciplinary care in heart failure outpatients at high risk of hospital readmission. J Am Coll Cardiol. 2002;39:471–480.
Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4:211–218.
Amarasingham R, Patzer RE, Huesch M, et al. Implementing electronic health care predictive analytics: considerations and challenges. Health Aff (Millwood). 2014;33:1148–1154.
Ohno-Machado L, Resnic FS, Matheny ME. Prognosis in critical care. Annu Rev Biomed Eng. 2006;8:567–599.
Moons KGM, Altman DG, Vergouwe Y, et al. Prognosis and prognostic research: application and impact of prognostic models in clinical practice. BMJ. 2009;338:b606.
Van Calster B, Vickers AJ. Calibration of risk prediction models: impact on decision-analytic performance. Med Decis Making. 2015;35:162–169.
Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–1379.
van der Ploeg T, Austin PC, Steyerberg EW. Modern modelling techniques are data hungry: a simulation study for predicting dichotomous endpoints. BMC Med Res Methodol. 2014;14:137.
Steyerberg EW, Borsboom GJJM, van Houwelingen HC, et al. Validation and updating of predictive logistic regression models: a study on sample size and shrinkage. Stat Med. 2004;23:2567–2586.
Orman ES, Ghabril M, Emmett TW, et al. Hospital readmissions in patients with cirrhosis: a systematic review. J Hosp Med. 2018;13(7):490–495.
Berman KT. Incidence and predictors of 30-day readmission among patients hospitalized for advanced liver disease.[Erratum appears in Clin Gastroenterol Hepatol. 2011 Jul; 9(7):625 Note: vuppalanch, Raj [corrected to Vuppalanchi, Raj]. Clin Gastroenterol Hepatol. 2011;9:254–259.
Singal AGR. An automated model using electronic medical record data identifies patients with cirrhosis at high risk for readmission. Clin Gastroenterol Hepatol. 2013;11(1335–1341):e1.
Bajaj JSR. The 3-month readmission rate remains unacceptably high in a large North American cohort of patients with cirrhosis. Hepatology. 2016;64:200–208.
Volk ML, Tocco RS, Bazick J, et al. Hospital re-admissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107:247–252.
Tapper EBF. Standard assessments of frailty are validated predictors of mortality in hospitalized patients with cirrhosis. Hepatology. 2015;62:584–590.
Hickey GL, Grant SW, Murphy GJ, et al. Dynamic trends in cardiac surgery: why the logistic EuroSCORE is no longer suitable for contemporary cardiac surgery and implications for future risk models. Eur J Cardiothorac Surg. 2013;43:1146–1152.
Minne L, Eslami S, de Keizer N, et al. Effect of changes over time in the performance of a customized SAPS-II model on the quality of care assessment. Intensive Care Med. 2012;38:40–46.
Davis SE, Lasko TA, Chen G, et al. Calibration drift in regression and machine learning models for acute kidney injury. J Am Med Inform Assoc. 2017;24:1052–1061.
Toll DB, Janssen KJM, Vergouwe Y, et al. Validation, updating and impact of clinical prediction rules: a review. J Clin Epidemiol. 2008;61:1085–1094.
Moons KGM, Kengne AP, Grobbee DE, et al. Risk prediction models: II. External validation, model updating, and impact assessment. Heart. 2012;98:691–698.
Van Calster B, Nieboer D, Vergouwe Y, et al. A calibration hierarchy for risk models was defined: from utopia to empirical data. J Clin Epidemiol. 2016;74:167–176.
Van Hoorde K, Van Huffel S, Timmerman D, et al. A spline-based tool to assess and visualize the calibration of multiclass risk predictions. J Biomed Inform. 2015;54:283–293.
Nezic D, Borzanovic M, Spasic T, et al. Calibration of the EuroSCORE II risk stratification model: is the Hosmer–Lemeshow test acceptable any more? Eur J Cardiothorac Surg. 2013;43:206.
Pencina MJ, Peterson ED. Moving from clinical trials to precision medicine: the role for predictive modeling. JAMA. 2016;315:1713–1714.
Parikh RB, Kakad M, Bates DW. Integrating predictive analytics into high-value care: the dawn of precision delivery. JAMA. 2016;315:651.
Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff Proj Hope. 2014;33:1203–1211.
Beste LA, Leipertz SL, Green PK, et al. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US Veterans, 2001–2013. Gastroenterology. 2015;149(1471–1482):e5.
Nehra MS, Ma Y, Clark C, et al. Use of administrative claims data for identifying patients with cirrhosis. J Clin Gastroenterol. 2013;47:e50–e54.
Re VL, Lim JK, Goetz MB, et al. Validity of diagnostic codes and liver-related laboratory abnormalities to identify hepatic decompensation events in the Veterans Aging Cohort Study. Pharmacoepidemiol Drug Saf. 2011;20:689–699.
Kanwal F, Kramer JR, Buchanan P, et al. The quality of care provided to patients with cirrhosis and ascites in the Department of Veterans Affairs. Gastroenterology. 2012;143:70–77.
Vincent P, Larochelle H, Lajoie I, et al. Stacked denoising autoencoders: learning useful representations in a deep network with a local denoising criterion. J Mach Learn Res. 2010;11:3371–3408.
Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE). 2014 Measures updates and specifications report hospital-level 30-day risk-standardized readmission measures. 2014:61. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures.html. Accessed 19.12.2018.
Brown SH, Lincoln MJ, Groen PJ, et al. VistA—U.S. Department of Veterans Affairs national-scale HIS. Int J Med Inf. 2003;69:135–156.
VA National Drug File—Data.gov. https://catalog.data.gov/dataset/va-national-drug-file-may-2015. Accessed 13.06.2017.
Lee DD, Seung HS. Learning the parts of objects by non-negative matrix factorization. Nature. 1999;401:788–791.
Lin X, Boutros PC. NNLM: Fast and versatile non-negative matrix factorization. 2016. https://cran.r-project.org/web/packages/NNLM/index.html. Accessed 25.04.2017.
Tibshirani R. Regression shrinkage and selection via the Lasso. J R Stat Soc Ser B. 1994;58:267–288.
Steyerberg EW, Eijkemans MJC, Harrell FE, et al. Prognostic modelling with logistic regression analysis: a comparison of selection and estimation methods in small data sets. Stat Med. 2000;19:1059–1079.
Steyerberg EW. Clinical Prediction Models: A Practical Approach to Development, Validation, and Updating. Berlin: Springer; 2008.
Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387.
Finazzi S, Poole D, Luciani D, et al. Calibration belt for quality-of-care assessment based on dichotomous outcomes. PLoS ONE. 2011;6:e16110.
Nattino G, Finazzi S, Bertolini G. A new calibration test and a reappraisal of the calibration belt for the assessment of prediction models based on dichotomous outcomes. Stat Med. 2014;33:2390–2407.
Pencina MJ, D’Agostino RB, D’Agostino RB, et al. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–172.
Kerr KF, Wang Z, Janes H, et al. Net reclassification indices for evaluating risk-prediction instruments: a critical review. Epidemiol Camb Mass. 2014;25:114–121.
Jiang X, Osl M, Kim J, et al. Calibrating predictive model estimates to support personalized medicine. J Am Med Inform Assoc. 2012;19:263–274.
Le SS. Could adherence to quality of care indicators for hospitalized patients with cirrhosis-related ascites improve clinical outcomes? Am J Gastroenterol. 2016;111:87–92.
Yang Y-YL. Identification of diuretic non-responders with poor long-term clinical outcomes: a 1-year follow-up of 176 non-azotaemic cirrhotic patients with moderate ascites. Clin Sci. 2011;121:509–521.
Gaduputi VC. Prognostic significance of hypokalemia in hepatic encephalopathy. Hepatogastroenterology. 2014;61:1170–1174.
Rassameehiran SM. Predictor of 90-day readmission rate for hepatic encephalopathy. South Med J. 2016;109:365–369.
Brown CL, Hammill BG, Qualls LG, et al. Significant morbidity and mortality among hospitalized end-stage liver disease patients in medicare. J Pain Symptom Manag. 2016;52(412–419):e1.
Deitelzweig SA. Hyponatremia-associated healthcare burden among US patients hospitalized for cirrhosis. Adv Ther. 2013;30:71–80.
Bariya M, Nyein HYY, Javey A. Wearable sweat sensors. Nat Electron. 2018;1:160.
Seal KH, Cohen G, Waldrop A, et al. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: implications for screening, diagnosis and treatment. Drug Alcohol Depend. 2011;116:93–101.
Bajaj JS, Wade JB, Gibson DP, et al. The multi-dimensional burden of cirrhosis and hepatic encephalopathy on patients and caregivers. Am J Gastroenterol. 2011;106:1646–1653.
Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. Jama. 2011;306:1688–1698.
Janssen KJM, Moons KGM, Kalkman CJ, et al. Updating methods improved the performance of a clinical prediction model in new patients. J Clin Epidemiol. 2008;61:76–86.
Kappen TH, Vergouwe Y, van Klei WA, et al. Adaptation of clinical prediction models for application in local settings. Med Decis Making. 2012;32:E1–E10.
Vergouwe Y, Nieboer D, Oostenbrink R, et al. A closed testing procedure to select an appropriate method for updating prediction models. Stat Med. 2017;36:4529–4539.
Kuzniewicz MW, Puopolo KM, Fischer A, et al. A quantitative, risk-based approach to the management of neonatal early-onset sepsis. JAMA Pediatr. 2017;171:365–371.
Amarasingham R, Patel PC, Toto K, et al. Allocating scarce resources in real-time to reduce heart failure readmissions: a prospective, controlled study. BMJ Qual Saf. 2013;22:998–1005.
Cronin PR, Greenwald JL, Crevensten GC, et al. Development and implementation of a real-time 30-day readmission predictive model. AMIA Annu Symp Proc. 2014;2014:424–431.
Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174:1095–1107.
Brock J, Mitchell J, Irby K, et al. Association between quality improvement for care transitions in communities and rehospitalizations among medicare beneficiaries. JAMA. 2013;309:381–391.
Gheorghiade M, Vaduganathan M, Fonarow GC, et al. rehospitalization for heart failure: problems and perspectives. J Am Coll Cardiol. 2013;61:391–403.
Tapper EBF. A quality improvement initiative reduces 30-day rate of readmission for patients with cirrhosis. Clin Gastroenterol Hepatol. 2016;14:753–759.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139.
Acknowledgments
JK was supported by the Department of Veterans Affairs, Office of Academic Affiliations, Advanced Fellowship Program in Medical Informatics, and the Department of Biomedical Informatics, Vanderbilt University, Nashville, TN. GC was supported by the NIH Precision Medicine Initiative Cohort Program Data and Research Support Center (1U2COD023196). MEM, GC, and SBH were supported by Veterans Health Administration Health Services Research & Development (HSR&D) Investigator Initiated Research (IIR 13-052). Support for SED was provided by National Library of Medicine (5T15LM007450).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We wish to confirm for all authors that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Fig. 7 and Tables 6, 7, 8, 9, 10, 11, 12, and 13.
NRI Results Expanded
The net reclassification index compares our primary model against each established model with values > 0 indicating improved prediction performance. Performance is shown for two use cases: (a) identifying patients at very low risk of readmission, < 10%, and (b) finding very high-risk patients, > 40% risk of readmission. Our model shows improved overall performance and outcome-specific performance (readmission versus no readmission). The outcome-specific NRI can be interpreted as the change in true positive rate for predicting readmission (or conversely improvement in the true negative rate for predicting no readmission).
When assessing our model’s performance at identifying low-risk patients (predicted probability of readmission within 30 days < 10%), the NRI shows significant improvement compared to all three extant models for the Berman, Bajaj, and Singal. The improvement was primarily driven by the model’s ability to identify patients who were not readmitted. When identifying high-risk patients (predicted probability of readmission within 30 days > 40%), the event-specific NRI for high-risk patients, i.e., predicting readmission accurately, was significantly better for our model compared to the Berman, Bajaj, and Singal.
Rights and permissions
About this article
Cite this article
Koola, J.D., Ho, S.B., Cao, A. et al. Predicting 30-Day Hospital Readmission Risk in a National Cohort of Patients with Cirrhosis. Dig Dis Sci 65, 1003–1031 (2020). https://doi.org/10.1007/s10620-019-05826-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05826-w