Abstract
Background
Glycated hemoglobin A1c (HbA1c) is routinely used to diagnose and monitor type 2 diabetes mellitus (T2DM) in cirrhotic patients. Remarkably, HbA1c may be falsely low in such patients.
Aims
We assessed the diagnostic and monitoring yield of HbA1c in cirrhotic patients with T2DM (DM-Cirr) and without T2DM (NoDM-Cirr).
Methods
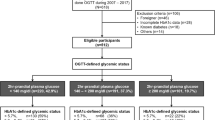
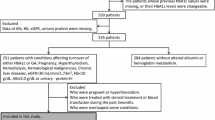
We conducted a composite study allocating 21 NoDM-Cirr into a cross-sectional module and 16 DM-Cirr plus 13 controls with T2DM only (DM-NoCirr) into a prospective cohort. Oral glucose tolerance test (OGTT) was performed in NoDM-Cirr. DM-Cirr and DM-NoCirr were matched by sex, age, BMI, and T2DM treatment and studied with continuous glucose monitoring (CGM). Percent deviations from target, low/high blood glucose indexes (LBGI/HBGI) were calculated from CGM, as well as the average daily risk range (ADRR) as a marker of glucose variability.
Results
Overall, HbA1c and OGTT diagnostic yield agreed in 12 patients (57%, ρ = 0.45, p < 0.03). CGM captured 3463 glucose determinations in DM-Cirr and 4273 in DM-NoCirr (p = 0.42). Regression analysis showed an inferior association between HbA1c and CGM in DM-Cirr (R2 = 0.52), when compared to DM-NoCirr (R2 = 0.94), and fructosamine did not improve association for DM-Cirr (R2 = 0.31). Interestingly, cirrhosis and Child–Turcotte–Pugh class accounted for HbA1c variance (p < 0.05). Patients in DM-Cirr were less frequently within target glucose (70–180 mg/dL), but at higher risk for hyperglycemia (HBGI > 9) when compared to DM-NoCirr, and they also showed higher glucose variability (ADRR 13.9 ± 2.5 vs. 8.9 ± 1.8, respectively, p = 0.03).
Conclusion
HbA1c inaccurately represents chronic glycemia in patients with cirrhosis, likely in relation to increased glucose variability.





Similar content being viewed by others
Abbreviations
- T2DM:
-
Type 2 diabetes mellitus
- NoDM-Cirr:
-
Cirrhosis but no T2DM
- DM-Cirr:
-
Cirrhosis and T2DM
- DM-NoCirr:
-
T2DM without cirrhosis
- OGTT:
-
Oral glucose tolerance test
- HbA1c:
-
Glycated hemoglobin A1c
- CGM:
-
Continuous glucose monitors
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- TIPS:
-
Transjugular intrahepatic portosystemic shunt
- BMI:
-
Body mass index
- INR:
-
International normalized ratio
- NGSP:
-
National Glycohemoglobin Standardization Program
- NPO:
-
Nothing by mouth
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- MELD:
-
Model for end-stage liver disease
- MELD-Na:
-
MELD-sodium
- LBGI:
-
Low blood glucose index
- HBGI:
-
High blood glucose index
- ADRR:
-
Average daily risk range
- HOMA-IR:
-
Homeostatic model assessment for insulin resistance
- 95% CI:
-
Confidence interval
References
Hashiba M, Ono M, Hyogo H, et al. Glycemic variability is an independent predictive factor for development of hepatic fibrosis in nonalcoholic fatty liver disease. PloS ONE. 2013;8:e76161.
Schiaffini R, Liccardo D, Alisi A, et al. Early glucose derangement detected by continuous glucose monitoring and progression of liver fibrosis in nonalcoholic fatty liver disease: an independent predictive factor? Horm Res Paediatr. 2016;85:29–34.
Elkrief L, Rautou PE, Sarin S, Valla D, Paradis V, Moreau R. Diabetes mellitus in patients with cirrhosis: clinical implications and management. Liver Int. 2016;36:936–948.
Huang JF, Yu ML, Dai CY, et al. Reappraisal of the characteristics of glucose abnormalities in patients with chronic hepatitis C infection. Am J Gastroenterol. 2008;103:1933–1940.
Garvey P, Murphy N, Flanagan P, et al. Disease outcomes in a cohort of women in Ireland infected by hepatitis C-contaminated anti-D immunoglobulin during 1970s. J Hepatol. 2017;67:1140–1147.
Jepsen P, Watson H, Andersen PK, Vilstrup H. Diabetes as a risk factor for hepatic encephalopathy in cirrhosis patients. J Hepatol. 2015;63:1133–1138.
Singh S, Singh PP, Singh AG, Murad MH, Sanchez W. Anti-diabetic medications and the risk of hepatocellular cancer: a systematic review and meta-analysis. Am J Gastroenterol. 2013;108:881–891.
Piano S, Morando F, Carretta G, et al. Predictors of early readmission in patients with cirrhosis after the resolution of bacterial infections. Am J Gastroenterol. 2017;112:1575–1583.
Gonzalez HC, Duarte-Rojo A. Virologic cure of hepatitis C: impact on hepatic fibrosis and patient outcomes. Curr Gastroenterol Rep. 2016;18:32.
Nathan DM, Turgeon H, Regan S. Relationship between glycated haemoglobin levels and mean glucose levels over time. Diabetologia. 2007;50:2239–2244.
D’Amico G, Pasta L, Morabito A, et al. Competing risks and prognostic stages of cirrhosis: a 25-year inception cohort study of 494 patients. Aliment Pharmacol Ther. 2014;39:1180–1193.
American Diabetes A. 2. Classification and diagnosis of diabetes. Diabetes Care. 2017;40:S11–S24.
Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–1495.
Altman DG, Gardner MJ. Calculating confidence intervals for regression and correlation. Br Med J (Clin Res Ed). 1988;296:1238–1242.
Clarke W, Kovatchev B. Statistical tools to analyze continuous glucose monitor data. Diabetes Technol Ther. 2009;11:S45–S54.
Monaghan M, Younge TB, McCarter R, Cogen FR, Streisand R. Average daily risk range (ADRR) in young children with type 1 diabetes. J Diabetes Sci Technol. 2014;8:70–73.
Roglic G, World Health Organization. Global Report on Diabetes. Geneva, Switzerland: World Health Organization; 2016:86.
Mokdad AA, Lopez AD, Shahraz S, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145.
Pattullo V, Duarte-Rojo A, Soliman W, et al. A 24-week dietary and physical activity lifestyle intervention reduces hepatic insulin resistance in the obese with chronic hepatitis C. Liver Int. 2013;33:410–419.
Haraguchi M, Miyaaki H, Ichikawa T, et al. Glucose fluctuations reduce quality of sleep and of life in patients with liver cirrhosis. Hepatol Int. 2017;11:125–131.
Ochi T, Kawaguchi T, Nakahara T, et al. Differences in characteristics of glucose intolerance between patients with NAFLD and chronic hepatitis C as determined by CGMS. Sci Rep. 2017;7:10146.
Kishimoto M, Noda M. Verification of glycemic profiles using continuous glucose monitoring: cases with steroid use, liver cirrhosis, enteral nutrition, or late dumping syndrome. J Med Invest. 2015;62:1–10.
Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ. Translating the A1C assay into estimated average glucose values. Diabetes Care. 2008;31:1473–1478.
Lahousen T, Hegenbarth K, Ille R, et al. Determination of glycated hemoglobin in patients with advanced liver disease. World J Gastroenterol. 2004;10:2284–2286.
Kim WR, Biggins SW, Kremers WK, et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. New Engl J Med. 2008;359:1018–1026.
Gallagher EJ, Le Roith D, Bloomgarden Z. Review of hemoglobin A(1c) in the management of diabetes. J Diabetes. 2009;1:9–17.
Sartore G, Chilelli NC, Burlina S, Lapolla A. Association between glucose variability as assessed by continuous glucose monitoring (CGM) and diabetic retinopathy in type 1 and type 2 diabetes. Acta Diabetol. 2013;50:437–442.
Shah AG, Lydecker A, Murray K, et al. Use of the FIB4 index for non-invasive evaluation of fibrosis in nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7:1104–1112.
Acknowledgment
We would like to thank Dr. Peter Goulden from the Division of Endocrinology and Metabolism for his kind advice and support during conception and implementation of the study.
Funding
This study was funded in full by a Diabetes Research Grant from the Sturgis Foundation and the University of Arkansas for Medical Sciences College of Medicine Clinician Scientist Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors have nothing to disclose
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of our Institutional Review Board (UAMS IRB) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Addepally, N.S., George, N., Martinez-Macias, R. et al. Hemoglobin A1c Has Suboptimal Performance to Diagnose and Monitor Diabetes Mellitus in Patients with Cirrhosis. Dig Dis Sci 63, 3498–3508 (2018). https://doi.org/10.1007/s10620-018-5265-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5265-3