Abstract
Background
A target-controlled infusion (TCI) of a propofol system uses a pharmacokinetic model to achieve and maintain a selected target blood propofol concentration. The aim of this study was to assess whether the propofol TCI system could be safely used by gastroenterologists in patients undergoing endoscopic resection including endoscopic submucosal dissection (ESD) and endoscopic mucosal resection (EMR) compared with a manually controlled infusion (MCI) system.
Methods
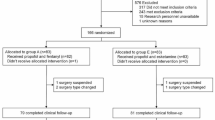
A total of 431 patients undergoing therapeutic endoscopy (178 ESD and 253 EMR) were consecutively included from November 2011 to August 2014. The patients were divided into the MCI (271) and TCI (160) propofol infusion groups. We compared adverse event rates in MCI and TCI groups and assessed independent risk factors for adverse events.
Results
The total sedation-related adverse event rate was 5.8 % (25/431). Most of the events were minor, and the rate of major events was 0.5 % (2/431). There was no significant difference in adverse event rate between the MCI and TCI groups [5.5 % (15/271) vs. 6.3 % (10/160); P = 0.759]. In univariate analysis, the propofol infusion time was significantly associated with adverse events (94.88 vs. 59.45 min, P = 0.017). In the multivariate analysis, there were no significant factors associated with adverse events. TCI was not an independent risk factor for adverse events despite the fact that the TCI had a longer duration of infusion and higher total infusion dose (95 % CI, 0.343–2.216; P = 0.773).
Conclusions
TCI of propofol by gastroenterologists may provide safe sedation in patients undergoing ESD and EMR under careful respiratory monitoring.
Similar content being viewed by others
References
Chung IK, Lee JH, Lee SH, et al. Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc. 2009;69:1228–1235.
Ono H, Kondo H, Gotoda T, et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225–229.
White M, Kenny GN. Intravenous propofol anaesthesia using a computerised infusion system. Anaesthesia. 1990;45:204–209.
Qadeer MA, Vargo JJ, Khandwala F, Lopez R, Zuccaro G. Propofol versus traditional sedative agents for gastrointestinal endoscopy: a meta-analysis. Clin Gastroenterol Hepatol. 2005;3:1049–1056.
Garewal D, Powell S, Milan SJ, Nordmeyer J, Waikar P. Sedative techniques for endoscopic retrograde cholangiopancreatography. Cochrane Database Syst Rev. 2012;6:CD007274.
Sethi S, Wadhwa V, Thaker A, et al. Propofol versus traditional sedative agents for advanced endoscopic procedures: a meta-analysis. Dig Endosc. 2014;26:515–524.
Leslie K, Clavisi O, Hargrove J. Target-controlled infusion versus manually-controlled infusion of propofol for general anaesthesia or sedation in adults. Cochrane Database Syst Rev. 2008;16:CD006059.
Gillham MJ, Hutchinson RC, Carter R, Kenny GN. Patient-maintained sedation for ERCP with a target-controlled infusion of propofol: a pilot study. Gastrointest Endosc. 2001;54:14–17.
Yamagata T, Hirasawa D, Fujita N, et al. Efficacy of propofol sedation for endoscopic submucosal dissection (ESD): assessment with prospective data collection. Intern Med. 2011;50:1455–1460.
Chiang MH, Wu SC, You CH, et al. Target-controlled infusion vs. manually controlled infusion of propofol with alfentanil for bidirectional endoscopy: a randomized controlled trial. Endoscopy. 2013;45:907–914.
Imagawa A, Hata H, Nakatsu M, et al. A target-controlled infusion system with bispectral index monitoring of propofol sedation during endoscopic submucosal dissection. Endosc Int Open. 2015;3:E2–E6.
Fanti L, Agostoni M, Casati A, et al. Target-controlled propofol infusion during monitored anesthesia in patients undergoing ERCP. Gastrointest Endosc. 2004;60:361–366.
Mazanikov M, Udd M, Kylanpaa L, et al. A randomized comparison of target-controlled propofol infusion and patient-controlled sedation during ERCP. Endoscopy. 2013;45:915–919.
Manyam SC, Gupta DK, Johnson KB, et al. When is a bispectral index of 60 too low? Rational processed electroencephalographic targets are dependent on the sedative-opioid ratio. Anesthesiology. 2007;106:472–483.
Chung F, Chan VW, Ong D. A post-anesthetic discharge scoring system for home readiness after ambulatory surgery. J Clin Anesth. 1995;7:500–506.
Sasaki T, Tanabe S, Azuma M, et al. Propofol sedation with bispectral index monitoring is useful for endoscopic submucosal dissection: a randomized prospective phase II clinical trial. Endoscopy. 2012;44:584–589.
Tackley RM, Lewis GT, Prys-Roberts C, Boaden RW, Dixon J, Harvey JT. Computer controlled infusion of propofol. Br J Anaesth. 1989;62:46–53.
Fanti L, Gemma M, Agostoni M, et al. Target controlled Infusion for non-anaesthesiologist propofol sedation during gastrointestinal endoscopy: the first double blind randomized controlled trial. Dig Liver Dis. 2015;47:566–571.
Fanti L, Agostoni M, Arcidiacono PG, et al. Target-controlled infusion during monitored anesthesia care in patients undergoing EUS: propofol alone versus midazolam plus propofol. A prospective double-blind randomised controlled trial. Dig Liver Dis. 2007;39:81–86.
Passot S, Servin F, Allary R, et al. Target-controlled versus manually-controlled in fusion of propofol for direct laryngoscopy and bronchoscopy. Anesth Analg. 2002;94:1212–1216. table of contents.
Sakaguchi M, Higuchi H, Maeda S, Miyawaki T. Dental sedation for patients with intellectual disability: a prospective study of manual control versus Bispectral Index-guided target-controlled infusion of propofol. J Clin Anesth. 2011;23:636–642.
Seifert H, Schmitt TH, Gultekin T, Caspary WF, Wehrmann T. Sedation with propofol plus midazolam versus propofol alone for interventional endoscopic procedures: a prospective, randomized study. Aliment Pharmacol Ther. 2000;14:1207–1214.
Moerman AT, Struys MM, Vereecke HE, Herregods LL, De Vos MM, Mortier EP. Remifentanil used to supplement propofol does not improve quality of sedation during spontaneous respiration. J Clin Anesth. 2004;16:237–243.
Chen SC, Rex DK. Review article: registered nurse-administered propofol sedation for endoscopy. Aliment Pharmacol Ther. 2004;19:147–155.
Overley CA, Rex DK. A nursing perspective on sedation and nurse-administered propofol for endoscopy. Gastrointest Endosc Clin N Am. 2004;14:325–333.
Tohda G, Higashi S, Sakumoto H, Sumiyoshi K, Kane T. Efficacy and safety of nurse-administered propofol sedation during emergency upper endoscopy for gastrointestinal bleeding: a prospective study. Endoscopy. 2006;38:684–689.
Heuss LT, Peter S. Propofol use by gastroenterologists-the European experience. Gastrointest Endosc Clin N Am. 2008;18:727–738, ix.
Rex DK, Deenadayalu V, Eid E. Gastroenterologist-directed propofol: an update. Gastrointest Endosc Clin N Am. 2008;18:717–725, ix.
Rex DK, Deenadayalu VP, Eid E, et al. Endoscopist-directed administration of propofol: a worldwide safety experience. Gastroenterology. 2009;137:1229–1237. ; quiz 1518–1229.
Gotoda T, Kusano C, Nonaka M, et al. Non-anesthesiologist administrated propofol (NAAP) during endoscopic submucosal dissection for elderly patients with early gastric cancer. Gastric Cancer. 2014;17:686–691.
Sieg A, Beck S, Scholl SG, et al. Safety analysis of endoscopist-directed propofol sedation: a prospective, national multicenter study of 24441 patients in German outpatient practices. J Gastroenterol Hepatol. 2014;29:517–523.
Dumonceau JM, Riphaus A, Beilenhoff U, et al. European curriculum for sedation training in gastrointestinal endoscopy: position statement of the European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastroenterology and Endoscopy Nurses and Associates (ESGENA). Endoscopy. 2013;45:496–504.
Acknowledgments
This research was supported by Hallym University Research Fund 2014 (HURF-2014-58).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Seo, S.I., Ryu, J.Y., Kang, S.S. et al. Safety of Target-Controlled Propofol Infusion by Gastroenterologists in Patients Undergoing Endoscopic Resection. Dig Dis Sci 61, 3199–3206 (2016). https://doi.org/10.1007/s10620-016-4256-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4256-5