Abstract
Background
Nonalcoholic fatty liver disease (NAFLD) is now recognized as a leading cause of liver dysfunction. Gastroesophageal reflux disease (GERD) is a common disorder causing symptoms that often impair patients’ quality of life. In recent years, the prevalence of both these diseases has increased, partially overlapping the rise of metabolic disorders.
Aims
We investigated whether a relation does exist between NAFLD and GERD symptoms.
Methods
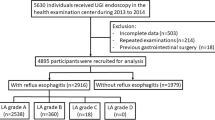
Cross-sectional study among 206 outpatients diagnosed with NAFLD and 183 controls. We collected clinical and laboratory data, assessed severity and frequency of GERD symptoms and the esophageal endoscopic pattern.
Results
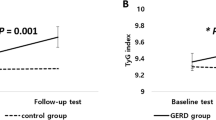
The prevalence of GERD symptoms was higher in NAFLD patients than controls (61.2 vs. 27.9 %, p < 0.001). We found a positive association between NAFLD and the experiencing of heartburn, regurgitation and belching. GERD symptoms were related to body mass index (BMI) and metabolic syndrome (MetS); a strong association persisted after adjustment for all the covariates (adjusted OR 3.49, 95 CI % 2.24–5.44, p < 0.001).
Conclusions
Our data show that the prevalence of GERD typical symptoms is higher in patients with NAFLD. GERD was associated with higher BMI and MetS, but not with age and diabetes type 2. NAFLD remained strongly associated with GERD, independently of a coexisting MetS status. Consistent with these findings, MetS can be considered a shared background, but cannot completely explain this correlation. We suggest NAFLD as an independent risk factor for GERD symptoms.
Similar content being viewed by others
References
Blachier M, Leleu H, Peck-Radosavljevic M, Valla DC, Roudot-Thoraval F. The burden of liver disease in Europe: a review of available epidemiological data. J Hepatol. 2013;58:593–608.
Tarantino G, Saldalamacchia G, Conca P, Arena A. Non-alcoholic fatty liver disease: further expression of the metabolic syndrome. J Gastroenterol Hepatol. 2007;22:293–303.
Kopec KL, Burns D. Nonalcoholic fatty liver disease: a review of the spectrum of disease, diagnosis, and therapy. Nutr Clin Pract. 2011;26:565–576.
Attar BM, Van Thiel DH. Current concepts and management approaches in nonalcoholic fatty liver disease. Sci World J. 2013;2013:481893.
Obika M, Noguchi H. Diagnosis and evaluation of nonalcoholic fatty liver disease. Exp Diabetes Res. 2012;2012:145754.
Lipan MJ, Reidenberg JS, Laitman JT. Anatomy of reflux: a growing health problem affecting structures of the head and neck. Anat Rec B New Anat. 2006;289:261–270.
Wu P, Zhao XH, Ai ZS, et al. Dietary intake and risk for reflux esophagitis: a case-control study. Gastroenterol Res Pract. 2013;2013:691026.
Ronkainen J, Agréus L. Epidemiology of reflux symptoms and GORD. Best Pract Res Clin Gastroenterol. 2013;27:325–337.
El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2013. doi:10.1136/gutjnl-2012-304269.
Camilleri M, Dubois D, Coulie B, et al. Prevalence and socioeconomic impact of upper gastrointestinal disorders in the United States: results of the US Upper Gastrointestinal Study. Clin Gastroenterol Hepatol. 2005;3:543–552.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421.
Standards of Practice Committee, Lichtenstein DR, Cash BD, et al. Role of endoscopy in the management of GERD. Gastrointest Endosc. 2007;66(2):219–24.
Krishnan B, Babu S, Walker J, Walker AB, Pappachan JM. Gastrointestinal complications of diabetes mellitus. World J Diabetes. 2013;4:51–63.
Promberger R, Lenglinger J, Riedl O, et al. Gastro-oesophageal reflux disease in type 2 diabetics: symptom load and pathophysiologic aspects—a retro-pro study. BMC Gastroenterol. 2013;13:132.
Ayazi S, Hagen JA, Chan LS, et al. Obesity and gastroesophageal reflux: quantifying the association between body mass index, esophageal acid exposure, and lower esophageal sphincter status in a large series of patients with reflux symptoms. J Gastrointest Surg. 2009;13:1440–1447.
Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143:199–211.
El-Serag HB, Graham DY, Satia JA, Rabeneck L. Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol. 2005;100:1243–1250.
Ierardi E, Rosania R, Zotti M, et al. Metabolic syndrome and gastro-esophageal reflux: a link towards a growing interest in developed countries. World J Gastrointest Pathophysiol. 2010;1:91–96.
Lee YC, Yen AM, Tai JJ, et al. The effect of metabolic risk factors on the natural course of gastro-oesophageal reflux disease. Gut. 2009;58:174–181.
Festi D, Scaioli E, Baldi F, et al. Body weight, lifestyle, dietary habits and gastroesophageal reflux disease. World J Gastroenterol. 2009;15:1690–1701.
Jung HS, Choi MG, Baeg MK, et al. Obesity is associated with increasing esophageal acid exposure in Korean patients with gastroesophageal reflux disease symptoms. J Neurogastroenterol Motil. 2013;19:338–343.
Hajar N, Castell DO, Ghomrawi H, Rackett R, Hila A. Impedance pH confirms the relationship between GERD and BMI. Dig Dis Sci. 2012;57:1875–1879.
Fox M, Barr C, Nolan S, Lomer M, Anggiansah A, Wong T. The effects of dietary fat and calorie density on esophageal acid exposure and reflux symptoms. Clin Gastroenterol Hepatol. 2007;5:439–444.
Wu JC, Mui LM, Cheung CM, Chan Y, Sung JJ. Obesity is associated with increased transient lower esophageal sphincter relaxation. Gastroenterology. 2007;132:883–889.
Shapiro M, Green C, Bautista JM, et al. Assessment of dietary nutrients that influence perception of intra-oesophageal acid reflux events in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2007;25:93–101.
Lacy BE, Carter J, Weiss JE, et al. The effects of intraduodenal nutrient infusion on serum CCK, LES pressure, and gastroesophageal reflux. Neurogastroenterol Motil. 2011;23(7):631–e256.
Holloway RH, Lyrenas E, Ireland A, Dent J. Effect of intraduodenal fat on lower oesophageal sphincter function and gastro-oesophageal reflux. Gut. 1997;40:449–453.
Altomare A, Ma J, Guarino MP, et al. Platelet-activating factor and distinct chemokines are elevated in mucosal biopsies of erosive compared with non-erosive reflux disease patients and controls. Neurogastroenterol Motil. 2012;24(10):943–e463.
Souza RF, Huo X, Mittal V, et al. Gastroesophageal reflux might cause esophagitis through a cytokine-mediated mechanism rather than caustic acid injury. Gastroenterology. 2009;137:1776–1784.
Mönkemüller K, Wex T, Kuester D, et al. Interleukin-1beta and interleukin-8 expression correlate with the histomorphological changes in esophageal mucosa of patients with erosive and non-erosive reflux disease. Digestion. 2009;79:186–195.
Rieder F, Cheng L, Harnett KM, et al. Gastroesophageal reflux disease-associated esophagitis induces endogenous cytokine production leading to motor abnormalities. Gastroenterology. 2007;132:154–165.
Yoshida N, Uchiyama K, Kuroda M, et al. Interleukin-8 expression in the esophageal mucosa of patients with gastroesophageal reflux disease. Scand J Gastroenterol. 2004;39:816–822.
Isomoto H, Saenko VA, Kanazawa Y, et al. Enhanced expression of interleukin-8 and activation of nuclear factor kappa-B in endoscopy-negative gastroesophageal reflux disease. Am J Gastroenterol. 2004;99:589–597.
Ma J, Altomare A, de la Monte S, et al. HCl-induced inflammatory mediators in esophageal mucosa increase migration and production of H2O2 by peripheral blood leukocytes. Am J Physiol Gastrointest Liver Physiol. 2010;299:G791–G798.
Tutuian R, Castell DO. Review article: complete gastro-oesophageal reflux monitoring—combined pH and impedance. Aliment Pharmacol Ther. 2006;24:27–37.
McGown C, Birerdinc A, Younossi ZM. Adipose tissue as an endocrine organ. Clin Liver Dis. 2014;18:41–58.
Coelho M, Oliveira T, Fernandes R. Biochemistry of adipose tissue: an endocrine organ. Arch Med Sci. 2013;9:191–200.
Kwon H, Pessin JE. Adipokines mediate inflammation and insulin resistance. Front Endocrinol. 2013;4:71.
Haase J, Weyer U, Immig K, et al. Local proliferation of macrophages in adipose tissue during obesity-induced inflammation. Diabetologia. 2013. doi:10.1007/s00125-013-3139-y.
Blüher M. Adipose tissue dysfunction contributes to obesity related metabolic diseases. Best Pract Res Clin Endocrinol Metab. 2013;27:163–177.
Harwood HJ Jr. The adipocyte as an endocrine organ in the regulation of metabolic homeostasis. Neuropharmacology. 2012;63:57–75.
Braunersreuther V, Viviani GL, Mach F, Montecucco F. Role of cytokines and chemokines in non-alcoholic fatty liver disease. World J Gastroenterol. 2012;18:727–735.
Jarrar MH, Baranova A, Collantes R, et al. Adipokines and cytokines in non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2008;27:412–421.
García-Galiano D, Sánchez-Garrido MA, Espejo I, et al. IL-6 and IGF-1 are independent prognostic factors of liver steatosis and non-alcoholic steatohepatitis in morbidly obese patients. Obes Surg. 2007;17:493–503.
Karbownik-Lewinska M, Szosland J, et al. Direct contribution of obesity to oxidative damage to macromolecules. Neuro Endocrinol Lett. 2012;33:453–461.
Palmieri VO, Grattagliano I, Portincasa P, Palasciano G. Systemic oxidative alterations are associated with visceral adiposity and liver steatosis in patients with metabolic syndrome. J Nutr. 2006;136:3022–3026.
Furukawa S, Fujita T, Shimabukuro M, et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004;114:1752–1761.
Kim YJ, Kim EH, Hahm KB. Oxidative stress in inflammation-based gastrointestinal tract diseases: challenges and opportunities. J Gastroenterol Hepatol. 2012;27:1004–1010.
Erbil Y, Türkoglu U, Barbaros U, et al. Oxidative damage in an experimentally induced gastric and gastroduodenal reflux model. Surg Innov. 2005;12:219–225.
Wetscher GJ, Hinder RA, Bagchi D, et al. Reflux esophagitis in humans is mediated by oxygen-derived free radicals. Am J Surg. 1995;170(6):552–556; discussion 556–557.
Farhadi A, Fields J, Banan A, Keshavarzian A. Reactive oxygen species: are they involved in the pathogenesis of GERD, Barrett’s esophagus, and the latter’s progression toward esophageal cancer? Am J Gastroenterol. 2002;97:22–26.
Oh TY, Lee JS, Ahn BO, et al. Oxidative damages are critical in pathogenesis of reflux esophagitis: implication of antioxidants in its treatment. Free Radic Biol Med. 2001;30:905–915.
Basaranoglu M, Basaranoglu G, Sentürk H. From fatty liver to fibrosis: a tale of “second hit”. World J Gastroenterol. 2013;19:1158–1165.
Jaeschke H. Reactive oxygen and mechanisms of inflammatory liver injury: present concepts. J Gastroenterol Hepatol. 2011;26:173–179.
Seki S, Kitada T, Sakaguchi H, et al. Clinicopathological significance of oxidative cellular damage in non-alcoholic fatty liver diseases. Hepatol Res. 2005;33:132–134.
Chalasani N, Deeg MA, Crabb DW. Systemic levels of lipid peroxidation and its metabolic and dietary correlates in patients with nonalcoholic steatohepatitis. Am J Gastroenterol. 2004;99:1497–1502.
Van de Wier B, Balk JM, Haenen GR, et al. Elevated citrate levels in non-alcoholic fatty liver disease: the potential of citrate to promote radical production. FEBS Lett. 2013;587:2461–2466.
Duseja A, Chawla YK. Obesity and NAFLD: the role of bacteria and microbiota. Clin Liver Dis. 2014;18:59–71.
Miele L, Cammarota G, Vero V, et al. Non-alcoholic fatty liver disease is associated with high prevalence of gastro-oesophageal reflux symptoms. Dig Liver Dis. 2012;44:1032–1036.
Fujikawa Y, Tominaga K, Fujii H, et al. High prevalence of gastroesophageal reflux symptoms in Patients with non-alcoholic fatty liver disease associated with serum levels of triglyceride and cholesterol but not simple visceral obesity. Digestion. 2012;86:228–237.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Catanzaro, R., Calabrese, F., Occhipinti, S. et al. Nonalcoholic Fatty Liver Disease Increases Risk for Gastroesophageal Reflux Symptoms. Dig Dis Sci 59, 1939–1945 (2014). https://doi.org/10.1007/s10620-014-3113-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3113-7