Abstract
Vascular tissue banking has been carried out in Brussels for over 30 years in compliance with EU and Swiss tissue banking regulations. A total of 2.765 vascular tissue donations were performed in Belgian, French, Netherlands and Suisse transplant centres: 547(20%), 1.013(37%) and 1.205(43%) during the first, second and third periods, respectively. 85% and 18% increase in donations during the second and third decades compared to previous one, were remarkable. Of the 7.066 evaluated vascular tissues, 2.407(227, 921 and 1.259) were discarded (34.1%), whereas 4.659(523, 1.861 and 2.275) accepted (65.9%) during the respective period. Of the 92 donated veins, 44(47.8%) were discarded and 48(52.2%) accepted. Allografts available for clinical application were stored in vapours of liquid nitrogen. A total of 4.636 allografts were delivered and transplanted for cases of infection (58%), critical limb ischaemia (16%) and congenital cardiac surgery (15%). Thirty veins were implanted. The progressive increases in donations of 20%, 37% and 43% and in transplantations of 20.8%, 34.6% and 45% during the first, second and third periods, respectively, were remarkable. Complications were reported after transplantation and these included acute rejection of two femoral arteries one month after transplantation. We conclude that the donation and transplantation of cryopreserved vascular allografts was stable with a progressive increase over time. Allografts were used predominantly for the treatment of infection, limb salvage for critical ischaemia and for neonates and infants with congenital cardiac malformation. Immune related rejection was observed. This should be a subject of future investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
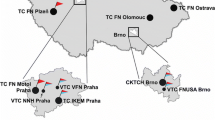
Vascular tissue banking has been conducted in Brussels over the last 30 years in a well-organized network of donation and transplantation of heart valves and vascular allografts (Goffin 1998; Verhelst 2000; Vogt 1995; Jashari 2004, 2013). After having launched a project of vascular tissue banking in 1991, donated arteries were first received by the end of the same year. First cryopreserved vascular allografts (CVAs) were allocated to the University Hospital of Leuven, Belgium, and implanted on January 10, 1992 by Professor Nevelsteen (for the treatment of infected aorto-bifemoral prosthetic graft), (Jashari 2004). Since then, the enthusiasm of vascular surgeons has grown progressively for the clinical use of CVAs in certain patient populations (Dodd 2010). Further, the legislation for organ donation in the European Union (EU) and Switzerland enabled the harvesting of vascular tissues in addition to organ recovery during multiorgan donation procedures. Over time, several bone banks were established in our TE network of cooperation that performed harvesting of femoral arteries (FA) for our TE concomitantly with the femoral bones (Jashari 2004, 2013), further increasing the number of procured tissues. Therefore, the cooperation network for donation and transplantation, established by our tissue establishment (TE), has similarly grown over time. This cooperation facilitated the creation of a large pool of arteries, with a diversity of types, sizes and lengths of allografts that were ready for clinical application. Gradually, an increasing number of surgeons have been considering human vascular tissues as the first choice for the treatment of vascular infection and critical limb ischaemia in cases where the autologous graft is missing (Verhelst 2000; Vogt 1995; Nevelsteen 1995, 1998).
The main goal of these TEs was the acquisition, preparation, testing and storage of cardiovascular tissues for clinical use. A quality controlled CVAs were made available for local surgical teams, but also for surgeons at other Institutions (Dodd 2010; Ben Ahmed 2018; Kieffer 2004; Buzi 2005, Spacek 2019; Dimitrievska 2018; Guevarra 2021; Furlogh 2019). Our TE, as an international nonprofit organization, has established a large international donation and transplantation cooperation and has distributed a remarkable number of CVAs in EU countries and elsewhere (Vogt 1995, 1996; Jashari 2004, 2013; Goffin 2000).
The implementation of tissue banking procedures, as well as early and midterm results of clinical use of allografts carried out by our TE, were already reported by our group (Goffin 1998; Jashari 2004, 2013). Moreover, in 2013 we reviewed our activity of 20 years (Jashari 2013). This study included our allocation algorithm, implantation results and complications for the indexed period.
This paper is a review of vascular tissue banking during the last decade (2012–2021) compared with the two previous periods (1992–2011). The donation and transplantation activity showed remarkable evolution with permanently increasing dynamics. Complications of vascular allografts are evaluated, commented and compared with the data from the previous periods. Furthermore, our activity was compared with the data published in the literature, reporting the activity of some other institutions. Also, some new clinical indications to the use of vascular allografts, observed during the last period, are discussed.
Material and methods
The donor selection criteria, harvesting, processing, preparation, storage and distribution of CVAs, have previously been reported by our TE (Goffin 1998; Jashari 2013). Briefly, donors of vascular tissues are selected by age (males up to 55 years and females up to 60 years), along with an evaluation of the past medical history: viral, bacterial and other transmissible diseases (Zika, Ebola COVID-19), autoimmune and degenerative diseases, diseases of unknown aetiology, malignant diseases and known medical treatment, including radio- and chemotherapy), as well as detailed assessment of the cardio-vascular status (arteriosclerotic disease or its predisposing factors, such as diabetes mellitus, smoking history or history of drug abuse). Our TE supplies the procurement centre with detailed instructions concerning the donation and harvesting of tissues as well as packaging and shipment material including the blood collection tubes (for the donor’s serology testing). The local transplant coordinator carries out the initial donor assessment, and informs our TE staff, discussing the donor acceptability for vascular tissues (Goffin 1998).
Upon arrival at the TE, the packaging and transport conditions of the retrieved material are verified by the responsible technical person. The blood samples are also controlled for conformity with good practice rules and then centrifuged and separated for serology controls (classical serology testing: HIV, HBV, HCV, HTLV, syphilis and other tests if necessary; NAT testing: HIV, HBV and HCV) and sent to the responsible laboratory for testing. The remaining volume of plasma and serum is stored in the serotheek for eventual later use, if necessary (Jashari 2013).
The donated human body substances are then processed in the class «A» cleanroom with vertical laminar flow and a class B/C background, as previously reported (Goffin 2000; Jashari 2010, 2011). The tissues are evaluated for transport conditions, for morphological alterations (atheroma, calcification, wall thickening), and (eventual) iatrogenic lesions that might occur during harvesting (cuts, haematomas, tears, media disruption); then, they are measured (proximal and distal diameter and length). The tissues, fulfilling the quality criteria for clinical use, are subsequently incubated in an antibiotic cocktail containing vancomycin, lincomycin and polimyxin B in RPMI solution (Roswell Park Memorial Institute, USA) for 20–48 h at + 4 °C (Jashari 2010, 2011). At the beginning of processing and before the final packaging for cryopreservation, samples of tissues and liquid (transport/preservation solutions) are taken, mixed, injected in the blood culture bottles and incubated for 14 days in an automated blood culture system (BD BACTEC FX) for the detection of eventual bacterial (aerobic, anaerobic) and fungal contamination (Jashari 2021). In addition, from each morphologically acceptable vessel, samples are collected from the proximal and distal sections for histological assessment of micromorphology (cells, extracellular matrix), presence of infection and eventual malignant infiltration (Jashari 2013). The allografts are immersed in a cryopreservation solution of 10% dimethyl sulfoxide (DMSO) in RPMI, subsequently cryopreserved using a computer controlled program, carried out in Planner 560–16 and finally stored in liquid nitrogen vapours at approximately − 178 °C, in a permanently monitored storage tank until their distribution for implantation (Jashari 2010, 2011).
The medical responsible person of the TE (Medical Director), after having analysed all donor information, shipment conditions and quality assessment reports, makes a final statement for the release of each suitable allograft for clinical application. The allograft, ready for clinical use, is placed in a storage tank until its shipment to the implanting centre. According to the EU Directive, the shelf life of cryopreserved allografts is 5 years. Past this time, the cryopreserved allograft is destroyed, if not used.
Vascular and cardiac surgeons from our network of collaboration and from abroad have been requesting the cryopreserved allografts on the basis of the patient’s clinical indication and state of urgency. Usually, the graft that best matches the patient’s situation is proposed, and the release statement, is sent to the surgeon. This statement includes a description of the morphology and function and the summary of the quality control results of the allograft and donor. The surgeon, after evaluating the proposed allograft and finding it suitable for his or her patient, signs it for acceptance and sends it back to the TE for approval, notating the date and time of planned implantation. The TE handles the shipment of allografts to the implanting centre (Goffin 2000, Jashari 2010). The implanting surgeon is requested to evaluate the quality of the allograft at the moment of implantation through a dedicated form (“traceability sheet of implantation”) that is then sent back to our TE. To obtain the critical opinion of implanting surgeons, they are requested to evaluate each allograft at the moment of implantation by completing this document and sending it back to our TE.
For this study, our Institutional database was reviewed, and the donor and tissue records were analysed. Additionally, clinical indications for the use of allografts are assessed and compared. Also, the feedback of the implanting surgeons, are taken into consideration as to assess the quality of allografts after their thawing for clinical use.
Results
Donations and harvesting
In total, 2.765 batches of vessels (predominantly arteries) were harvested and sent to our TE from the Belgian, French, Suisse and Dutch organ and tissue donation centres over a span of 30 years: 547 (20%), 1.013 (37%) and 1.205 (43%) during the respective first, second and third periods. This makes an increase of 85.2% and 18.8% during the second and third periods, respectively, compared to the previous period (Fig. 1a, b).
Discarded versus accepted tissues
A considerable number of vascular tissues were discarded during processing for a diversity of reasons, such as morphology, contamination, histology or other factors, as highlighted in Table 1. Out of 750, 2.782 and 3.534 or total of 7.066 arteries evaluated during the first, second and third decades, 227 (30.3%), 921 (33.1%) and 1.259 (35.6%) were discarded (with a total of 2. 407 discarded tissues or 34.1%). Consecutively, a total of 4.659 vascular tissues (65.9%), or 523 (69.7%), 1.861 (66.9%) and 2.275 (64.4%) were accepted and stored during the first, second and third periods, respectively (Fig. 2). The progressive augmentation of discarded tissues was remarkable. As contamination problems became an important issue in our TE during the third period, the discard rate increased from 31% in the second period to 44.1% in the last decade (Table 1).
Only 92 venous donations were received over the period of 30 years, of which 44 (47.8%) were discarded and 48 (52.2%) were prepared and stored. Only 30 of them were distributed and implanted.
Clinical application of vascular allografts
Overall, 4.636 quality-controlled vascular allografts were distributed for clinical application, spread as follows: 946 (20%), 1.605 (35%) and 2.085 (45%) during the first, second and third periods, respectively. There was an augmentation of implantations, namely 66.5% and 28.2% during the second and third periods, respectively, compared to the previous period. Figure 3a, b highlight the progress of the dynamics of implantations per period, whereas Fig. 4 shows the implantations per type of allograft over time. It is obvious that the femoral arteries (FA) were predominantly implanted vessels with 2.520 implantations, followed by descending thoracic aortas (AD) with 655 implantations and nonvalvular pulmonary conduit (nVPC) with 643 implantations. Slightly less distributed vessels were the iliac arteries (IA) and the abdominal aorta with bifurcation (ABif) with 334 and 317 implantations, respectively, and ascending thoracic aortas (AA/Arch) with 138 implantations. Our TE has distributed a limited number of venous allografts (30 cryopreserved veins were sent for transplantation only during the last period).
The users of vascular allografts predominantly comprised the surgical teams of the donation centres that we have been cooperating with (in Belgium, France and Switzerland). Nevertheless, a considerable number of CVAs were implanted by other, nonsupplying centres, predominantly for emergency situations (infected vascular prostheses or mycotic aneurysms with a septic state and bleeding complications or critical limb ischemia, who were at risk for limb amputation). Table 3 highlights the clinical indications for the use of vascular allografts distributed by our TE.
Complications
Several technical errors have occurred over time (1.8% of all discarded vessels over 30 years, or 1.6% only during the last period). Among these errors, we recorded failure of cryopreservation, inappropriate temperature recording by the logger during the allograft shipment, falling of the tissue during manipulation and loss during shipment. In the majority of cases, these errors led unfortunately to severe damage and elimination of allograft.
In 2013 we reported the issue of not using allografts despite thawing in the operating room. This issue remains an important challenge for TEs, as some surgeons, because the process is time consuming, prefer to thaw the allograft prior to starting the surgical procedure. However, the strategy might change over the course of the procedure (for any reason). In those cases, the allograft is lost and may no longer be used (Jashari 2013). In the first two periods, 36 cases of this complication were reported over 20 years. During the last decade, this complication appeared less frequently than previously, being reported in 10 cases. As this practice can provoke an unnecessary decrease in the availability of allografts (also leading to financial problems), the implanting teams are systematically warned not to open the transport container before the surgeon decides to use it. If the allograft is thawed but not used, our recommendation is to discard the allograft.
The temporary storage of cryopreserved allografts in the implanting center is not recommend by our TE. Therefore, if prior to starting the surgical procedure the surgeon is not sure whether the allograft will be used, he or she is advised not to open the transport container or DS until the final decision is made. If the allograft is not implanted and the dry-shipper remained sealed, the allograft is safely returned back to the TE and further stored in a storage tank. Nevertheless, in some cases, the sealing of the DS is broken at the implanting center although the allograft has not been used. In these cases, the temperature logger, which records the temperature inside the DS continuously, reveals if the temperature has increased and for how long. In these cases, we accept the allograft back into stock only if the temperature during the whole trajectory of shipment was constantly below − 130 °C. Otherwise, it is no longer suitable for clinical application.
If 2 or more allografts are shipped in the same DS, a “cryoguard™ ” is placed in the cardboard box with the allografts that change their colour once the temperature rises above − 130 °C. In this case, all returned allografts must be destroyed or used for validation procedures. In no case may they be used for clinical application.
Unfortunately, some vascular allografts, after shipment to the implanting centre, have been stored locally at − 80 °C when not used immediately. As these freezers are not always appropriately monitored for the temperature fluctuation, our TE do not take any responsibility for the quality of these allografts and we strongly warn against this practice. In contrast, our recommendation is not to store cryopreserved allografts in the implanting centres.
Complications immediately after implantation
Some immediate allograft ruptures with severe bleeding, were reported by the implanting surgeons in the beginning of our experience (Nevelsteen 1998, Verhels 2000). Following the investigation of these events, we concluded that these complications appeared due to the inappropriately thawing of the allografts. Our TE has established a strict and validated thawing protocol. Therefore, the thawing instructions provided with each allograft have to be strictly followed in the implanting centres. Similarly, the antiseptic measures during thawing must be strictly respected. During the last period, we have not recorded any thawing complication.
Few complications were reported by some implanting surgeons during the follow-up period. The most stunning complication was an acute rejection of 2 FAs after implantation in a young patient, treated for an infected vascular prosthetic graft of the femoro-popliteal region (Soquet 2015).These allografts, procured from the same donor, were prepared and distributed by our TE. Due to multiple aneurysm formation, both allografts had to be explanted only one month after implantation. Histological examination of the explanted allografts showed massive T-cell infiltration and subtotal necrosis of the arterial wall with multiple ruptures, associated with pseudoaneurysms and intramural haematomas. The allografts were the seat of acute cellular rejection. There were no microorganisms detected in the explanted allografts. Following explanation of the failed allografts, arterial reconstruction was performed with two new cryopreserved femoral arteries (again delivered by our TE). These arteries were well tolerated, without any aneurysmal degeneration or thrombosis after 1 year of follow-up.
Discussion
Alexis Carrel reported successful experimental transplantation of venous autografts and allografts for arterial reconstruction at the beginning of the last century. The work of Carrel and Guthrie from that period was widely reported in the world medical literature. Carrel stored the venous and arterial segments for several days to weeks in the Locke’s solution and used them for vascular tissue transplantation in animals (Carrel 1908). For his work in the field of organ and tissue transplantation, in 1912, Carrel was honoured with the Nobel Prize for Physiology and Medicine. Important clinical advances followed closely on the heels of Carrel's discoveries (Harrison 1976).
In the years 90 s, the structured vascular tissue banking started in Europe with the establishment of several TEs that were cooperating with organ donation networks. The purpose of these TEs was the acquisition, procurement, preparation, quality control and storage of vascular allografts aimed at clinical application. Our TE in Brussels was one of the first organized vascular TEs in Europe, located in Brussels. It involved a large donation and transplantation network from several EU countries and Switzerland. In 2013 we reported data from 20 years of our activity, showing stable performance with progressive augmentation of donation and transplantation. This paper reports the implantation of 2.506 arterial segments in 1.600 patients between 1992 and 2010 (Jashari 2013).
In the present study we report on 4.636 CVAs distributed by our TE in a large network of implantation within the EU member states and abroad. The number of implanted allograft has increased progressively over the three reported periods. Figures 3a, b and Table 2 highlight the implantation activity per period and per type of allograft. We observe an augmentation of 170% and 129% during second and third period. The femoral arteries were the predominant type of vascular allograft distributed by our TE.
Nonetheless, the number of discarded tissues has also increased progressively over the last 10 years, mainly due to the contamination of tissues. One of the reasons for this increased rate of contamination was the increase in harvested abdominal vessels (abdominal aortic bifurcation, iliac arteries and some veins) at our request following the increase of needs for vascular tissues, expressed by implanting surgeons. Furthermore, there was an increased interest of abdominal oncology surgeons for some short segments of iliac arteries. As the iliac vessels are harvested at the end of organ recovery for transplantation, the risk of contamination is present due to prolonged exposure of the donor abdominal cavity to the environment of operating room (sometimes more than 5–6 h). Additionally, leakage from the intestines might occur due to unrecognized microtrauma during abdominal organ recovery.
Another reason for the increased contamination of tissues was the relocation of our TE to another hospital in 2015. The laboratory of the new Hospital faced some difficulties in adapting its procedures to the bacteriology tests required by the tissue banking rules. Consequently, soon after moving to the new facility, we observed a sharp increase of contaminations. The contamination became almost prominent reason for discarding tissues with respective 44.7%, 47%, 53.9 and 40.8% rates compared to those of all reasons for discarding tissues in 2015, 2016, 2018 and 2019 (Table 1). Therefore, we decided to implement a closed system for bacteriology testing (the BD BACTEC FX blood culture system), which was validated during 2017 and 2018 and implemented for the routine sterility testing in May 2019 (Jashari 2021).
The availability of arterial allografts is variable, depending on donation (there are periods with high and periods with low volume of donations). In the other hand, there is also important variability in implantations as the indications for the use of arterial allografts are predominantly the emergency situations, such as an infection with septic state of the patient, or cases with the critical limb ischemia and amputation risk, necessitating an urgent intervention. These cases, if multiple in a short interval, might provoke a serious decrease of availability of allografts with as consequence, important stock shortage. Nevertheless, almost all requests for the vascular allografts, arriving from our transplantation network, were met systematically and immediately. However, in some cases, the proposed combination of vessels for construction of composite grafts (AD-IA-FA) could not be always possible. In those cases, a discussion with the implanting surgeon is necessary in order to find the best solution (“hybrid procedure” using a prosthetic graft in the proximal segment, continued with the arterial allografts distally, where the diameter of native artery is smaller) or temporary delay of surgery (if possible) until the suitable allografts are released by the TE.
There is no recommendation from the EU Directives and the National Competent Authorities (NCA) for reporting the long-term results after allograft implantation. In contrast, the notification regarding all serious adverse events (SAEs) and reactions (SARs) including the corrective and preventive measures taken by the TE, is mandatory and has to be reported to the NCA. Nevertheless, for a better understanding of the performance and durability of implanted tissues, in the past, some mid- and long-term follow-up studies have been performed and published in cooperation with the implanting centres.
Results of implanted cryopreserved arterial allografts
The arterial allografts distributed by our institution have been the subject of some studies by several authors (Verhelst 2000; Vogt 1995, 1996; Nevelsteen 1995, 1998; Soquet 2015). A considerable number of these allografts was used for the treatment of vascular infections (55.3%, 67.6% and 57.8% of all implanted vessels during the respective first, second and third periods), such as prosthetic graft infection, mycotic aneurysms, infected native arteries, entero-vascular fistulas and pseudoaneurysms at the level of vascular anastomoses (Table 3).
Vogt et al. compared the results of cryopreserved vascular allografts, prepared and distributed by our TE, with vascular prostheses in a series of patients presenting with mycotic aneurysm of the native aorta or infection of vascular prosthesis (Vogt 1995). This study showed superior outcomes in patients treated with CVAs in terms of disease-related survival, freedom from reoperation, duration of ICU stay, hospitalization, duration of postoperative antibiotic therapy, incidence of complications and elimination of infection. According to this study, the use of CVAs is advantageous for prosthetic grafts employed to treat fungal aneurysms and infected vascular grafts.
Also, several studies from other TEs and their implantation networks have demonstrated an increased resistance of vascular allografts against infection, comparable to abovementioned findings.
In one of the early European publications, Mestres and colleagues reported promising outcomes of CVAs in the reduction of hospitalization, patency of allografts and a lower rate of reinfection and rupture (Mestres 1995).
Leseche reported the long-term results with the arterial allografts for the treatment of infected native abdominal aorta or prosthetic graft (Leseche 2001). No persistent or recurrent infection was observed, and none of the patients received long term (> 3 months) antibiotic therapy. The 3 year primary and secondary allograft patency rates were 81% and 96%, respectively. This study concluded that the management of abdominal aortic infection with cryopreserved arterial allograft is a useful option. Interestingly, the allografts used in this study were not cryopreserved by the controlled rate cooling (currently, a standard cryopreservation procedure of the cardio-vascular TEs worldwide), but only stored in the preservation medium and directly frozen in a deep freezer at − 80 °C until their use. The preservation and storage method implemented in this study does not comply with the currently used method worldwide, although few TEs still use routinely this «unusual» practice. Nevertheless, it would be interesting to compare the long-term durability of these to the allografts cryopreserved by controlled rate freezing, as mentioned above.
A similar study was published recently and reported a series of patients treated with arterial allografts either for native abdominal aortic or for prosthetic graft infection (Ben Ahmed 2018). The survival rates were 75%, 64% and 54% at 1, 3 and 5 years, respectively. Late reinfection during the follow-up appeared in 4% of patients. The primary patency rates of the allograft were 100%, 96% and 96% at 1, 3 and 5 years, respectively. The authors of this study concluded that, although the prognosis of native or prosthetic aortic graft infection is poor, the treatment of infection with cryopreserved arterial allograft offers acceptable results.
So far, this study appears to show the best results with the use of CVAs to treat vascular infection.
Harlander-Locke advocates the use of cryopreserved aortic allografts for aortic reconstitution after removal of infected prosthetic grafts or for aortic procedures at high risk for graft infection, due to increased resistance of vascular allografts against infection (Harlander-Locke 2014). The 5 year rates of freedom from graft-related complications, graft explant and limb loss were 80%, 88%, and 97%, respectively. Primary graft patency was 97% at 5 years, and patient survival was 75% at 1 year and 51% at 5 years. The results of this study demonstrate that cryopreserved aortic allografts enable aortic reconstruction in the setting of infection or those with a high risk for infection, with lower early and long-term morbidity and mortality than other, non-allograft treatment options. This procedure is associated with low rates of aneurysm formation, recurrent infection, aortic blowout, and limb loss. The authors recommend CVAs as the first-choice treatment for aortic infection.
Finally, a review paper published at the European Journal of Vascular and Endovascular Surgery reported the use of CVAs for arterial reconstruction after aorto-iliac infection. This review included 31 published studies with 1.377 operated patients (Antonopoulos 2019). It reports good results including: early (30 day) mortality (14.9%) and allograft-related complications (29.,5%) such as peri-anastomotic rupture/allograft disruption (5.9%), aneurysmal degeneration/allograft dilation (5%), pseudoaneurysms (3%), allograft thrombotic/stenotic complications (12.2%), peri-anastomotic infection (3.3%) and allograft-related reoperations (23.5%) with a late mortality of 19%. Further, the allograft related reoperation rate during follow up was 25%. This review concludes that the use of cryopreserved arterial allografts for arterial reconstruction after aorto-iliac infection appears to be a safe and durable.
According to the studies discussed above, several complications were inevitable, particularly in the early postoperative period, as a consequence of severe infection (sepsis, bleeding tendency, allograft rupture, suture loss). Nevertheless, all these studies concluded that the treatment of vascular infection with the use of CVAs was advantageous compared to prosthetic vascular grafts in terms of early and late reinfection, thrombosis and postoperative death.
Results of implanted cryopreserved venous allografts
Banking of venous allografts was not a priority of our TE, as the vascular surgeons of our collaboration network were primarily interested in the use of arterial allografts. Only during the last period, were a total of 92 veins donated (on our request) and only 30 venous allografts were distributed for implantations. Veins were harvested together with abdominal organs and aortic bifurcations. They were sent to our TE for processing, quality control, cryopreservation and storage. Currently, we are still storing several veins, although we have only occasional requests for their implantation.
Regarding the indications, in the first instance, the venous allografts were aimed at venous reconstruction during or after liver transplantation, in cases of vascular complications. When the transplantation procedure is uneventful, the harvested veins and aortic bifurcation, are transferred to our TE for processing, storage and quality control (under tissue regulation). No saphenous veins were harvested, processed and stored by our TE during the reported periods.
Currently, the banking procedures for veins are identical to the techniques used for processing of arterial tissues. Several studies have reported quite controversial results after the arterial reconstruction using the cryopreserved venous allografts.
The surgical community in Belgium and in our implantation network did not show a particular interest for this type of vascular tissues, probably due to the disappointing results reported in the world literature after the use of allogenic veins as arterial substitutes (Axthelm 1976; Ochsner 1984; Walker 1993). According to the data from the literature, venous allografts have been clinically used over several decades, mainly for the treatment of infection and critical limb ischemia in absence of autologous venous grafts, which are considered as the «gold standard» for these indications. Reported patency of venous allografts and limb salvage have ranged from good to poor.
Early enthusiasm for the clinical use of venous allografts was based largely on the clinical report by Tice and Santoni, describing the excellent intermediate-term patency of implanted venous allografts (Tice 1976). This paper reported the technique of procurement, preparation and storage of venous allografts including the quality tests. Veins were appropriately labelled, then stored at − 50 °C until their clinical use.
According to several authors, about 20–30% of all vascular patients do not have an adequate saphenous vein for vascular bypass due to previous phlebitis, surgical removal or anatomic variations (Axthelm 1979). Furthermore, as many of the TEs often do not have arterial allografts available in their stock for a variety of problems, the interest surged in the use of saphenous vein allografts (whether fresh, antibiotic stored at + 4 °C or cryopreserved) for arterial reconstruction.
Walker reported a series of lower extremity arterial reconstructions with cryopreserved saphenous vein allografts because of the absence of autologous veins (Walker 1993). In this study, 39 patients with critical limb ischaemia received a lower extremity bypass graft. There were 35 femorotibial reconstructions, three below-the-knee femoropopliteal reconstructions, and one femoropedal reconstructions. Twenty-five grafts (64%) were constructed with cryopreserved vein only, whereas 14 (36%) were composite grafts (10 constructed with polytetrafluoroethylene, one with Dacron, and three with spliced native saphenous veins). The mean follow-up was 9 months. There were 12 early graft occlusions and an additional 17 late failures, resulting in a primary cumulative graft patency rates of 67%, 56%, 43%, 28%, and 14% at 1, 3, 6, 12, and 18 months, respectively. Salvages of failed grafts resulted in secondary cumulative graft patency rates of 87%, 77%, 61%, 46%, and 37% at these same intervals. There was no significant difference in primary and secondary graft patency rates related to diabetes, ABO graft/donor compatibility, graft composition or orientation, indication for surgery, state of the outflow tract or site of distal anastomosis. Limb salvage was attained in 24 (67%) of the 36 limbs. The overall performance of cryopreserved saphenous vein allografts in early follow-ups was disappointing.
Ochsner reported the largest early experience with the clinical use of venous allografts with 129 saphenous vein allografts implanted in 91 patients (58% in the femoropopliteal, tibial, or peroneal artery; 29.5% in the aortocronary artery; 10% in the pulmonary artery and 0.8% were used for an arteriovenous fistula, a carotid-subclavian artery, and a brachial-radial artery. The cumulative patency rate showed that while 50% of venous allografts were occluded within 1 year, 60% of the remaining allografts continued to be functional for more than 5 years. Microscopic observation of failed grafts revealed a prominent mononuclear cell infiltrate with allograft necrosis, compatible with the immunologic rejection reaction (Ochsner 1984).
The outcome of venous allografts is variable and unpredictable. Therefore, the use of allogenic saphenous veins is suitable only when the autologous tissue or an arterial allografts are unavailable (Ochsner 1984).
Use of cryopreserved allografts in paediatric cardiac surgery
For the reconstruction of the aortic arch in newborn patients and children, our institution distributed 643 allografts or approximately 15% of all distributed CVAs (during the second and third periods) and approximately 10% during the first period. Many paediatric cardiac surgeons consider the cryopreserved allogenic nonvalvular pulmonary conduit (nVPC) as a “gold standard” for the repair of hypoplastic left heart syndrome (HLHS) or arch interruption (Amri 2022; Lewis 2020; van Beynum 2021). Our TE distributed 46, 220 and 377 nVPCs during the first, second and third periods, respectively, presenting an increase of 478% in the second and 171% in the third period compared to the previous period.
To date, we do not have structured follow-up data regarding implanted nVPCs in paediatric cardiac patients, as the number of implanting centers is too large and the numbers of implantations per center are relatively small. Nevertheless, the feedback forms sent to our TE immediately after their use did not reveal important problems during and immediately after implantation. However, to evaluate the durability of this allograft type for the abovementioned indications, a multi-centric study including the different operation techniques and implanting surgeons, might provide valuable information for the TEs. As the number of implanted allografts of this type is not negligible, this should be a subject of the future studies of our TE.
Few papers have reported the treatment of hypoplastic aortic arch and/or aortic coarctation using an allograft patch of the pulmonary trunk (nVPC). Amri reported a cohort of 76 patients (neonates and infants) who underwent aortic arch reconstruction using an allograft patch. There was no 30 day mortality. Three patients (3.95%) died in the hospital after 30 days. The median follow-up was 35 months, whereas the 5 years survival was 93.4%. The rate of reintervention on the aortic arch was 9.2% (Amri 2022).
Lewis reviewed 124 consecutive paediatric patients who underwent corrective surgery for congenital heart defects with excellent results. The 15 year survival and 15 year freedom from reintervention in the area of patch reconstruction were 83.9% and 89.2%, respectively. The rates of mortality (0%), cardiac transplantation (0%), and reoperation (0.8%) attributable to the area of patch reconstruction, were very low. The authors considered the allograft patches harvested from PA branches to be an effective material for reconstruction of the aorta in small children. Long-term results showed no risk of aneurysm formation and low rates of stenosis formation (Lewis 2020).
The paediatric cardiac surgery group of Rotterdam has reported on 36 patients who underwent aortic arch repair, either with pulmonary allograft or with tissue engineered bovine pericardium (CardioCel). Restenosis was documented during the first year of life in 23% of the allograft group with 70% in the CardioCel group. After superior results of the human nVPC compared to decellularized bovine pericardial patch in this study, the authors of this study stopped using the engineered bovine pericardial patch, considering human nVPC the best option thus far for aortic arch reconstruction in neonates and infants (van Beynum 2021).
Some other indications for vascular allografts
For vascular reconstruction following malignant invasion from the surrounding organs (mainly stomach, pancreas, liver, or intestines), 1.3%, 0.4% and 3.2% of all implanted vascular allografts were used during the first, second and third periods, respectively. Usually, a short segment of iliac artery and/or vein was required. Therefore, the requests for the venous allografts and short iliac arteries have grown seriously in the last period compared to the respective first and second periods.
The use of cryopreserved arteries for the treatment of vascular trauma showed decreasing evolution, with 3.3%, 1.9% and 0 0.3% of arterial allografts used during first, second and third period, respectively.
Replacement of arterial allografts for degeneration was an indication for the use of arterial allografts in 1.5%, 0.9% and 1.2% during the first, second and third periods, respectively. Although there was an important increase in implanted allografts in the last period, the proportion of failures remained remarkably low, approximately equivalent to that in the previous two periods.
In conclusion, the activity of donation and transplantation of vascular allografts, as carried out by our TE, has shown a progressive increase over time. Despite the large number of distributed allografts, the number of processing and postimplantation complications is relatively low. Nevertheless, due to the high need for the treatment of patients with specific problems, the improvement and enlargement of cooperation with donation centers could increase the availability of vascular tissues for clinical application. In the other hand, the procurement procedures as well as the processing, decontamination and cryopreservation, and handling of the test samples should be further improved in order to increase the safety and quality of the allografts and reduce the rate of discard.
The issue of premature degeneration of allografts (veins/arteries) in some patients should be the subject of future studies.
References
Amri A et al (2022) Contemporary outcomes of aortic arch hypoplasia and coarctation repair in a tertiary pediatric cardiac surgery centre. Cardiol Young 32(7):1098–1103. https://doi.org/10.1017/S1047951121003747
Antonopoulos C, Papakonstantinou N, Hardy D, Lyden S (2019) Editor’s choice of cryopreserved allografts for arterial reconstruction after aorto-iliac infection: a systematic review and meta-analysis. Eur J Vasc Endovasc Surgery 58(1):120–128. https://doi.org/10.1016/j.ejvs.2019.03.003
Axthelm S, Porter J, Strickland S, Baur G (1979) Antigenicity of venous allografts. Ann Surgery 189(3):290–293
Ben Ahmed S, Louvancourt A, Daniel G et al (2018) Cryopreserved arterial allografts for in situ reconstruction of abdominal aortic native or secondary graft infection. J Vasc Surgery 67(2):468–477. https://doi.org/10.1016/j.jvs.2017.06.088
Buzzi M, Mirelli M, Vaselli C et al (2005) Vascular tissue banking: state of the art. Transpl Proc 37:2428–2429
Carrel A (1908) Results of the transplantation of blood vessels, organs and limbs. JAMA 51:1662
Dimitrievska S, NiklasonL E (2018) Historical perspective and future direction of blood vessel developments. Cold Spring Harb Perspect Med 8:a025742
Dodd PD (2010) Wat tissue bankers should know about the use of allograft blood vessels. Cell Tissue Bank 11(1):3–11. https://doi.org/10.1007/s10561-009-9149-9
Furlough CL, Jain AK, Ho KJ, Rodriguez HE (2019) Peripheral artery reconstructions using cryopreserved arterial allografts in infected fields. J Vasc Surgery 70(2):562–568. https://doi.org/10.1016/j.jvs.2018.10.111
Goffin YA, Grandmugin D, Wozniak G et al (1998) Banking and distribution of large cryopreserved arterial homografts in brussels: assessment of 4 years of activity by the European Homograft Bank (EHB) with reference to implantation results in reconstruction of infected infrarenal arterial prostheses and mycotic aneurys. Vasc Surgery 32(1):19–32
Goffin YA, Van Hoeck B, Jashari R, Soots G, Kalmar P (2000) Banking of cryopreserved heart valves in Europe: assessment of a 10-year operation in the European Homograft Bank (EHB). J Heart Valve Dis 9(2):207–214
Guevara-Noriega KA, Villamizar A, Juan G, Castro-Rios JG, Pomar JL (2021) Outcomes of vascular allograft transplants in the autonomous community of Catalonia, Spain. Cir Cir 89(6):797–805. https://doi.org/10.24875/CIRU.20001069
Harlander-Locke P, Harmon MP, Lawrence LK, Oderich PF et al (2014) The use of cryopreserved aortoiliac allograft for aortic reconstruction in the United States. J Vasc Surgery 59:669–674
Harrison LH (1976) Historical aspects in the development of venous autografts. Ann Surgery 183(2):101–106
Jashari R, Van Hoeck B, Tabaku M et al (2004) Banking of the human heart valves and the arteries at the European homograft bank (EHB) -overview of a 14-year activity in this International Association in Brussels. Cell Tissue Bank 5(4):239–251. https://doi.org/10.1007/s10561-004-1441-0
Jashari R, Goffin Y, Van Hoeck B et al (2010) Belgian and European exprerience with the European Homograft Bank (EHB) cryopreserved allograft valves. -Assessment of a 20 year activity. Acta Chir Belg 110:280–290
Jashari R, Faucon F, Hoeck B et al (2011) Determination of residual antibiotics in cryopreserved heart valve allografts. Transfus Med Hemother 38(6):379–386. https://doi.org/10.1159/000334706
Jashari R, Van Hoeck B, Ngakam R, Goffin Y et al (2013) Banking of cryopreserved arterial allografts in Europe: 20 years of operation in the European Homograft Bank (EHB) in Brussels. Cell Tissue Bank 14(4):589–599. https://doi.org/10.1007/s10561-012-9359-4
Jashari R, Vanzeebroeck S, Petit P et al (2021) The BD BACTEC FX blood culture system with the gentlemacs dissociator is suitable for sterility testing of heart valve and vascular allografts-A validation study. Cell Tissue Bank 22(3):453–466. https://doi.org/10.1007/s10561-020-09893-6
Kieffer E, Gomes D, Chiche L et al (2004) Allograft replacement for infrarenal aortic graft infection: early results in 179 npatients. J Vasc Surgery 39:1009–1017
Leseche G, Castier G, Petit M-D et al (2001) Long-term result of cryopreserved arterial allograft reconstruction in infected prosthetic grafts and mycotic aneurysms of the abdominal aorta. J Vasc Surgery 34:616–622
Lewis MJ et al (2020) Long-term results of aortic arch reconstruction with branch pulmonary artery homograft patches. J Card Surgery 35(4):868–874. https://doi.org/10.1111/jocs.14494
Mestres C-A, Mulet J, Pomar J-L (1995) Large-caliber cryopreserved arterial allografts in vascular reconstructive operations: early experience. Ann Thorac Surgery 60:S105–S107
Nevelsteen A, Goffin Y, Lacroix H, Vandeginste N, Suy R (1995) Recurrent aortic infection: treatment by arterial homograft replacement. Cardiovasc Surgery 3(4):441–444. https://doi.org/10.1016/0967-2109(95)94166-t
Nevelsteen A, Feryn T, Lacroix H, Suy R, Goffin Y (1998) Experience with cryopreserved arterial allografts in the treatment of prosthetic graft infections. Cardiovasc Surgery 6(4):378–383. https://doi.org/10.1016/s0967-2109(98)00014-3
Ochsner JL, Lawson JD, Eskind SJ, Mills NL, DeCamp PT (1984) Homologous veins as an arterial substitute: long-term results. J Vasc Surgery 1:306–313
Soquet J, Chambon JP, Goffin Y, Jashari R (2015) Acute rejection of a cryopreserved arterial homograft. Cell Tissue Bank 16(3):331–333. https://doi.org/10.1007/s10561-014-9489-y
Spacek M, Mericka P, Janousek L et al (2019) Current vascular allograft procurement, cryopreservation and transplantation techniques in the Czech Republic. Adv Clin Exp Med 28(4):529–534. https://doi.org/10.17219/acem/90037
Tice A, Victor R, Zerbino AR, Wayne OI et al (1976) Coronary artery bypass with freeze-preserved saphenous vein allografts. J Thorac Cardiovasc Surgery 71(3):378–382
van Beynum IM et al (2021) Reconstruction of the aortic arch in neonates and infants: the Importance of Patch Material. World J Pediatr Congenit Heart Surgery 12(4):487–491. https://doi.org/10.1177/21501351211003502
Verhelst R, Lacroix V, Vraux H et al (2000) Use of cryopreserved arterial homografts for management of infected prosthetic grafts: a multicentric study. Ann Vasc Surgery 14(6):602–607. https://doi.org/10.1007/s100169910109
Vogt PR, von Segesser LK, Goffin Y, Pasic M, Turina MI (1995) Cryopreserved arterial homografts for in situ reconstruction of mycotic aneurysms and prosthetic graft infection. Eur J Cardiothorac Surgery 9(9):502–506. https://doi.org/10.1016/s1010-7940(95)80050-6
Vogt PR, von Segesser LK, Goffin Y, et al (1996) Eradication of aortic infections with the use of cryopreserved arterial homografts. Ann Thorac Surg 62(3):640–645. https://doi.org/10.1016/s0003-4975(96)0045-4
Walker PJ, Mitchell RS, McFadden PM et al (1993) Early experience with cryopreserved saphenous vein allografts as a conduit complex limb-salvage. J VAsc Surgery 18:561–569
Acknowledgements
We acknowledge Ms. BVH for all of her dedication to our TE over 3 decades and her contribution to the data collection for this particular study and several other studies published in the past.
Funding
There was no funding required for this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R. Jashari was Medical Director until June 30th 2021 and S. Mastrobuoni is the current Medical Director of EHB.
Ethical approval
Since April 2019, EHB has been taken over by the UCL Saint Luc (UCL St. Luc is a nonprofit University Hospital). This TE holds ethical approval for its tissue banking activity (donation, transplantation, research) from the Ethics Committee of the UCL St. Luc. All donors reported in this study gave their consent for organ/tissue donation for clinical application and/or research in compliance with the EU/Belgian tissue banking regulation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jashari, R., Bouzet, V., Alcaraz Blanco, MJ. et al. Vascular allografts for clinical application in Europe: assessment of 30 years of experience with vascular tissue banking in Brussels. Cell Tissue Bank 24, 613–625 (2023). https://doi.org/10.1007/s10561-022-10063-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-022-10063-z