Abstract
A burn is a sudden injury which immediate or long-term consequences may be life-threatening for the patient. A mass disaster event may involve large numbers of severely burned patients. Patients of this type typically have a limited area of healthy, unburned skin from which an autologous split thickness skin graft could be collected. In a clinical situation of this type, it is necessary to use a particular skin substitute. Non-viable allogeneic human skin graft materials might be considered as the most suitable skin substitutes in the treatment of such patients. At present, Poland does not have a sufficient supply of human allogeneic skin graft materials to meet the needs arising from a sudden and unforeseen mass disaster. This study involved an analysis of selected mass disasters. From this an estimate was made from a verified casualty profile of the necessary minimum stock of human allogeneic skin graft materials. An insufficient amount of skin results from an inadequate number of skin donors, which in turn results from the current tissue donation system. Therefore, a proposal has been made for the organizational, legal and systemic changes required to improve the situation in Polish transplantology, with particular emphasis on skin donation. In order to achieve a strategic stock of human skin grafts, a tissue collecting transplantation team should be organized. The rights and obligations of the non-physician transplant team member should be extended. Proposals have been made for awareness campaigns (adverts, posters etc.) and educational schemes (educational video, lectures during transplant coordinator training, etc.). Finally, a proposal has been made for possible methods to deal with the logistic management of the allogeneic skin stock. The required, essential stock of human allogeneic skin in the event of a mass disaster has been estimated at 600,000 cm2.
Similar content being viewed by others
Introduction
As a result of a thermal injury, a vast area of the patient's skin may be damaged. Extensive and deep burns require specialist treatment. The optimal method of treatment for extensive full-thickness skin burns (III˚) is to perform an autologous split thickness skin graft (STSG) donated from a body part with intact skin (Busuioc et al. 2012; Glik et al. 2017; Kitala et al. 2016; Grossova et al. 2017; Prim et al. 2017). However, despite total tissue compliance, which should be considered the main advantage of STSG, such grafts have a number of disadvantages and limitations (e.g. creation of a new wound—donor site, infection risk, pain, scaring etc.) (Kitala et al. 2016). In order to overcome these limitations, the application of biological skin substitutes may be considered (Glik et al. 2017; Kitala et al. 2016), an advantage of which may be the reduction of the donor site surface area and shortening of the hospitalization time for burn patients (Kitala et al. 2016). In this aspect, an important role may be played by allogeneic human skin graft materials (Busuioc et al. 2012; Glik et al. 2017; Kitala et al. 2016; Grossova et al. 2017; Prim et al. 2017; Voigt et al. 2017).
The importance of allogeneic human skin graft therapy in the treatment of burns is the established method of treating burns (Busuioc et al. 2012; Glik et al. 2017; Kitala et al. 2016; Grossova et al. 2017; Prim et al. 2017). The confirmation of this has been recommended by many authors (Busuioc et al. 2012; Glik et al. 2017; Kitala et al. 2016; Grossova et al. 2017; Prim et al. 2017; Voigt et al. 2017), including the recommendations of the European Burns Association (EBA), which have been in force for many years. According to these recommendations, each ward, unit or hospital treating burns should have access to a skin bank (Voigt et al. 2017).
The skin bank is a specialized laboratory involved in the collection, processing, storage and distribution of allogeneic human skin graft materials (Voigt et al. 2017).
With this approach, having a sufficiently large supply of human allogeneic skin graft materials ready for clinical use may be particularly important in the event of a sudden fire mass disaster leading to a large number of victims. There have been a number of fire mass disasters, including terrorist attacks (e.g. New York City September 11, 2001), indoor fires (e.g. Colectiv Nightclub Fire, Bucharest, Romania—October 30, 2015) or transportation crashes (e.g. Alcanar, Spain—July 11, 1978) (Haller et al. 2017). In Poland, since the year 2000, there have been 7 mass disasters in charcoal mines alone. The research by Relvas LM et al. has shown a gap in the planning for major burn disasters in Europe (Relvas et al. 2018). The prospect of establishing a strategic stock of allogeneic human skin transplants is an endeavor that requires a thorough analysis, including determination of local, facility and employment requirements. Additionally, the hardware and logistical needs should be analyzed. Another important aspect that should be taken into consideration is the estimation of the necessary minimal stock of human allogeneic skin graft materials, based on an analysis of selected historical fire mass disasters.
Bearing in mind all these aspects, the goal of the study was to propose the legal and systemic changes required to improve the situation of Polish transplantology, with particular emphasis on skin donation. The second goal of the study was to propose possible methods of achieving this strategic stock of human skin graft material and the methods for the logistical management of the allogeneic skin stock.
Materials and methods
Brief literature review of mass disasters with high numbers of burn casualties
Keywords concerning mass disasters, fires, traffic accidents and burn patients were entered into the available databases (PubMed, ClinicalKey, etc.). Additionally, available literature on disaster medicine and burn treatment was analyzed, including the medical documentation of the Dr Stanisław Sakiel Centre for Burn Treatment (CLO), Poland and Municipal Hospital in Siemianowice Śląskie, Poland.
The system of burn treatment in Poland has been briefly described.
Estimation of the necessary minimum stock of human allogeneic skin graft materials
The potential was analyzed for human allogeneic skin as a source of biomaterials for regenerative medicine.
An analysis of the extent of patient burns was performed, related to casualties of selected mass disasters from recent years in Poland. The utilization of human allogeneic skin graft materials transplanted onto these patients was analyzed. Additionally, an analysis was performed of everyday routine utilization of human allogeneic skin graft materials in recent years (2018, 2019 and 2020). The area of the transplanted human skin graft materials and the number of treatments/transplants required per patient were assessed. On this basis, the probable profile of burn casualties was estimated (total body surface area (TBSA), the area of the required skin graft materials and the number of necessary transplantations). Additionally, the probability of mass disaster occurrence was estimated. The situations were assessed where the available stock of human allogeneic skin was fully utilized and whether there was a clinical need for these products.
New and innovative methods of using human allogeneic skin were analyzed. The use of Acellular Dermal Matrix ADM in various areas of regenerative medicine was analyzed.
Proposed organizational, legal and systemic changes that could help to increase the number of skin retrievals
Risk analysis was performed to determine the critical elements of the proposed process.
The current legal situation regarding transplantology in Poland was analyzed, including the applicable legal acts. The situation related to organ and tissue donation in Poland was analyzed, not only based on potential skin donation from organ donors but also on only-tissue donors (cadaveric).
Based on the data obtained from POLTRANSPLANT, an analysis was performed of the number of multi-organ donations in which no tissues were collected or only the skin was not collected.
The need and proposal were assessed for an applicable awareness campaign, education for medical specialists (TCs, intensivists etc.) and society to increase the level of skin donations.
Additionally, a number of systemic solutions were proposed, e.g. appointment of a transplant team to collect tissues, the proposal that tissue banks should be allowed to perform a tissue donation to avoid formal problems and increase the skin donations, incorporation of other applicable forms of consent (opt-in, consent on behalf), etc.
The necessity of additional training for professionals to talk to families (transplant coordinators) was proposed. In relation to this an educational video was created to describe the skin donation process.
Possible methods of achieving a strategic stock of human skin graft materials
To assess the possibility of collecting allogeneic human skin transplants, the following is required:
Evaluation of monthly income from human allogeneic skin graft materials (A)
Evaluation of monthly utilization of human allogeneic skin graft materials (B)
Calculation of A—B = C
The value of C constitutes the amount of skin graft materials remaining monthly, which is the amount that can be saved as stock. Therefore, the value of A must be increased enough to (under normal conditions) save the required amount of skin per month (e.g. 10 000 cm2, 50 000 cm2 or more…).
Possible logistical management methods for the allogeneic skin stock
A needs analysis was performed regarding the stock management process. The development of a computer program (e.g. on the basis of MS Excel) is required which can indicate (in advance) the transplant stocks where the expiry date is due to expire soon, and therefore which should be used first (basic stock of allogeneic skin graft materials, leaving it intact).
An analysis of the needs of employment and the purchase of additional equipment was performed. The development of a tissue banking organization for an increased skin donation ratio should take into account: resources: personnel, clean room, and equipment required to cover proper processing and preservation.
Results
Literature review of mass disasters with high numbers of burn casualties
Entering the “mass”, “disaster”, “casualty” and “burns” key words into the PubMed database generated 313 results. Of these, 95 were selected as meeting the search criteria. One original work describing a given mass event was selected for the analysis. A total of 20 papers were selected to present a brief review of the most frequent mass burn casualty incident scenario.
It should be also mentioned that a new consensus for mass burn treatment has been established recently (Hughes et al. 2021; Leclerc et al. 2021). A Technical Working Group on burns (TWGB) at World Health Organization (WHO) has been established. A result of the work by TWGB was 22 recommendations to provide a framework for national and international specialized burn teams and health facilities to support the delivery of safe care and improved outcomes for burn patients in mass casualty incidents (Hughes et al. 2021). The available literature also raised the topic of the current COVID-19 pandemic situation. The reality of a mass burn casualty incident needs to be rethought in the face of the current SARS-CoV-2 virus pandemic. The main conclusions concerned the conversion of burns centers and their infrastructure in the event of a pandemic requiring isolation, specific Triage schemes and Optimal Care of burn patients in the case of a pandemic (including Triage and Optimal Care of mass burn processes), securing material delivery (e.g. stocking/warehousing of specific drugs), international exchange and ensuring cross-border communication (Kamolz et al. 2020).
The available literature included cutaneous radiation injuries (Parrish and Seda 2019; DiCarlo et al. 2020), armed conflicts (Haverkamp et al. 2019), parties/concerts/discos (Chen et al. 2019; Lin et al. 2019; Tseng et al. 2019; Yang et al. 2019), communication accidents (Ewbank et al. 2018), terrorist attacks (Konwinski et al. 2016; Ozoilo et al. 2010; Sheridan et al. 2017, Hunt et al. 2020), mass chemical casualties (Zhang et al. 2015), petroleum and LPG explosions (Kumar 2013; Carlsonet al. 2015), earthquakes (Kearns and Holmes 2014), indoor fires (Koning et al. 2015), forest fires (Seifman et al. 2011), and mine explosions (Allister and Hamilton et al. 1983).
Historically, the large-scale human exposures to radiation could be represented by the U.S. bombings of Hiroshima and Nagasaki. Briefly, the devastation resulting from the dropping of the atomic bombs on Japan in August of 1945 gave the immediate death after the explosion to the majority of all casualties. In addition approx. 50% of the deaths following the explosion were due to thermal burns and approx. 65% of the casualties had combined radiation injuries (i.e., radiation exposure combined with another trauma such as burns or other wounds) (DiCarlo et al. 2020). The total number of deaths followed by the exposure to the bomb by the end of 1945 reached approx. 140,000 in Hiroshima and approx. 70,000 in Nagasaki (Iijima 1982).
Analyzes of modern historical armed conflicts have shown that burns are one of the most common injuries after landmine explosions or gunshot wounds. It should be additionally emphasized that pediatric patients are among the most frequent victims of burns. Children were more likely to be injured in many parts of the body and had higher in-hospital mortality than adults (Haverkamp et al. 2019).
An example of a mass fire during mass events can be the situation that occurred on June 27, 2015 in the Formosa Fun Coast water park in Bali in New Taipei, Taiwan. Employees of an outdoor "party with colored powder" threw a cloud of cornstarch at the participants, which caught fire. The fire lasted 40 s and burned 508 people, killing 15 people and leaving 199 in a critical condition. The mean age of the casualties was 22.5 ± 5 years while the mean TBSA was 48.9% ± 20%. During the hospitalization two mortalities (2/37, 5.4%) were reported: one was related to cardiac insult, and another was caused by sepsis (Chen et al. 2019).
Another type of mass burn disaster is the transport crash. On August 28, 1988 in Ramstein (hist. West Germany), an aircraft collision occurred during the airshow. The crash killed 70 and seriously injured more than 1000 out of the 300,000 people present. The TBSA of the casualties ranged between 20 and 70% (Haller et al. 2017).
The historic terrorist attacks on New York City of September 11, 2001 are worth of description. The two hijacked planes were flown directly into the Twin Towers of the World Trade Center. Although many were injured or killed, few survivors had severe burns. The victims were sent primarily to two burn centers, although more were readily accessible. Nineteen were seen at the New York Presbyterian Hospital, where the mean age of the victims was 44 years and the average burn rate was 52.7% (Haller et al. 2017).
Another relevant terrorist attack that should be mentioned was that in Kuta, Bali, Indonesia—October 12, 2002. A suicide bomber detonated a bomb in a backpack at a nightclub. The people there ran outside, where a car bomb exploded. A total of 202 people were killed and 209 were injured. Eleven patients were transferred to the Concord Repatriation General Hospital. Burns ranged from 15 to 85% TBSA, mostly full-thickness burns. All patients showed both first and the second-degree burns. Complications related to Acinetobacter baumannii and Pseudomonas aeruginosa infections occurred. There were also many eye injuries (Haller et al. 2017).
The representative example of chemical burn incident occurred on 31 August 2013 in Shanghai. During restoration work in a closed cold room, there was a leakage of anhydrous ammonia. As a result, 41 people (out of 58) suffered severe burns. Ten casualties died because of severe inhalation injury at the scene, and another five casualties died during the transportation process to the nearest hospital. The six most serious patients with inhalation injuries were admitted to the burn intensive care unit. One of that patients died because of respiratory failure and ongoing pulmonary infection (Zhang et al. 2015).
Another example of fire mass disaster are petroleum pipeline fires and explosions. The frequency and impact of that incidents especially in sub-Saharan Africa could be classified as common and cause significant morbidity and mortality. It should be emphasized that the most common cause of the original leak was intentional, either from theft or vandalism, or by militia activity (Carlson et al. 2015).
Significant earthquakes typically include burns as one of the more common injuries. The Haiti earthquake on January 10, 2010 resulted in a number of burned patients with approx. 40% TBSA. Due to the lack of adequate medical infrastructure on site, the patients were transferred to other hospitals, especially in the USA (Kearns et al. 2014).
An example of mass casualty indoor fire could be the incident that occurred on June 27, 2011 in a nursing home in Utrecht, Netherlands. The number of casualties that needed hospitalization was 49 among them 9 patients needed intubation. No deaths occurred (Koning et al. 2015).
An example of mass burn disasters resulting from wildfires could be the “Black Saturday” disaster that occurred on February 7, 2009 in the state of Victoria, Australia. The event claimed 173 lives and the compensation cost more than AUD 4 billion. (Seifman et al.2011).
The literature paid attention to the important role of allogeneic human skin collected from a deceased donor during the therapy for extensive and deeply burned victims of a mass catastrophe (Brown and Fryer 1954; Horner et al. 2013).
Review of mass disasters with high numbers of burn casualties in Poland
On November 24, 1994, during the Polish pop band concert (“Golden Life”) that took place in the Gdańsk Shipyard the fire occurred. The first symptoms of fire were recognized as an additional lighting effects. The fire spread rapidly and the curtains and the wooden roof were already burning. Panic broke out and people started to run to the emergency exits trampling on each other (two victims died in the scuffle). Additionally, two of the five emergency exits were closed. Totaling, 7 people died and over 300 were injured out of the 2000 participants. The action of escorting the event participants from the building lasted about 20 min. The temperature inside the hall reached 1000 Celsius degrees. 80 people were taken to the Hospital of the Medical Academy of Gdańsk, where 5 people died as a result of burns. Then, the 24 the most severely burned patients were immediately transported by helicopters to the burn ward in Municipal Hospital in Siemianowice Śląskie. Among these patients, the mean burn area was 39.76% TBSA (SD 17.89). The mean age of the hospitalized patients was 24.32 years (SD 9.97). All hospitalized patients had burned respiratory tract, except for 3 patients. The most severely burned patients were two bodyguards aged 45 and 27 years, burned in 67% and 65% of TBSA consecutively, including respiratory tract burns. Both of them died as a result of the injuries.
The research by Borys and Majkowicz (2004a; b) revealed a significant impact of this traumatic experience on the mental health of the victims and their behavior (Borys and Majkowicz 2004a; b).
The described event was an impulse for the Burn Treatment Center (CLO) to be established in 1996 as a specialist hospital that deals with the treatment of burn patients.
The further analysis of the historical mass burn disasters revealed that 7 fire accidents occurred in Polish carbon mines in the 2000–2014 period. The average number of casualties was 11.16 (SD 6.21). The maximum number of casualties hospitalized in CLO was 18 and minimum was 2. It should be emphasized that the CLO tissue bank was established in 2008 and achieved efficiency in 2010. For that reason, the 2014 disaster in KWK Wujek-Śląsk was the most suitable for analysis.
The analysis of the KWK Wujek-Śląsk explosion showed that the number of hospitalized patients was 18, and the average TBSA was 56.22% (SD 14.90). The maximum TBSA was 90% and the minimum was 21%.
Additionally, it should be remarked that during this mass burn disaster a deficit occurred of allogeneic human skin graft and allogeneic human amniotic membrane graft materials.
Review of allogeneic skin graft materials utilization at CLO
The utilized allogeneic skin graft material at CLO was analyzed, including 495 clinical cases of everyday routine use of allogeneic human skin graft materials. The period of time covered the years 2018, 2019 and 2020. The number of hospitalized patients was 1244 in 2018, 1297 in 2019 and 1033 in 2020, totaling 3574 patients. Of these, 13.85% received a human allogeneic skin graft.
The number of thermal burns treated with human allogeneic skin was 483, chemical burns was 4, chronic ulcers was 4 and frostbite was 2. Additionally, 2 cases involved toxic epidermal necrolysis (TEN) treated with human allogeneic skin graft materials. The mean TBSA of the patients was 19.15% (SD 15.30), maximum TBSA was 80% and minimum TBSA was 1%.The average area of the transplanted skin graft materials was 1651.09 cm2 (SD 1749.84), with a maximum of 12,783 cm2 and minimum of 21 cm2.
Estimation of the necessary minimum stock of human allogeneic skin graft materials
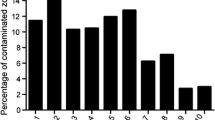
The number of skin donations collected in each year for the period 2009–2020, along with the area of the prepared and grafted grafts, is presented in Fig. 1.The same figure also shows that since the beginning of allogeneic skin retrieval activities at CLO in 2009 until the end of 2020 a total of 456 allogeneic skin retrievals were performed. It should be also mentioned that in 2015 a contract was signed with a forensic facility to cover the period until the end of 2018. It can be seen that during the 2015–2018 period the number of prepared and grafted allogeneic skin graft materials was higher at some point, as can be seen in Fig. 1.
In accordance with the cases in the literature and the analysis of historical fire mass accidents in Poland, an estimation has been proposed of the minimum stock of human allogeneic skin transplant materials, with the following assumed:
30 hospitalized patients
patients with 60% TBSA
patients will require approx. 10,000 cm2 of allogeneic skin graft materials
patients will require skin grafts twice.
In relation to the above assumptions, it was assumed that the minimum, inviolable stock of human allogeneic skin graft materials should be 600,000 cm2.
System of burn treatment in Poland
The system of burn treatment in Poland assumes that every surgical ward is able to treat burns except for extreme burns (J22), severe burns (J23) and moderate burns (J24). Such cases may be treated only in specialized units or wards. In Poland there are five specialized units or wards that treat burns. These are the Dr. Stanislaw Sakiel Centre for Burn Treatment in Siemianowice Śląskie CLO (monospecialist unit), Ludwik Rydygier Specialist Hospital in Krakow (ward), Eastern Center for Burn Treatment and Reconstructive Surgery in Łęczna (monospecialist unit), West Pomeranian Center of Severe Burns Treatment and Plastic Surgery in Gryfice (monospecialist unit) Multidisciplinary City Hospital, and Józef Strus with Care and Treatment Institute SPZOZ in Poznań (ward).However, the only tissue establishment (skin bank) is located in CLO.
The ICD9 code of the procedure for allogeneic skin transplantation is 86.662. Such a procedure can be performed for the following JGP groups:
J22–Extreme burns with surgery > 15 days
J23–evere burns with surgery > 10 days
J24–Average burns/frostbites with surgery > 5 days
J32Major skin treatments (http://jgp.uhc.com.pl/doc/28.5/icd9/86.662.html).
Review of the legal situation in Poland
Donors of allogeneic skin are qualified in accordance with Polish transplant act implementing Directive 2004/23/EU, Commission Directive 2006/17/EC and Commission Directive 2006/86/EC.
That means that all transplantation issues in Poland are regulated by the Act of July 1, 2005 on the collection, storage and transplanting of cells, tissues and organs (“Transplantation Act”) with subsequent changes (Journal of Laws of 2009, No. 141, item 1149).
The act regulates in detail the rules of retrieval, storing and cell transplantation, including hematopoietic cell bone marrow, peripheral blood and umbilical cord blood.
The provisions of the act also apply to derived tissues and organs from living donors or cadavers.
It was established to achieve the required levels of quality and safe standards for the donation, collection, testing, processing, preservation, storage and distribution of human tissues and cells. This directive applies to tissues and cells that include hematopoietic products, cord blood and bone marrow stem cells, reproductive cells fetal, adult and embryonic tissues and stem cells. This regulation involves tissues and cells for use in industrial manufacture, including medical devices, exclusively when it comes to donation, procurement and testing.
However, it does not apply to processing, preservation, storage and distribution. Further manufacturing steps are included in Directive 2001/83/EC of the European Parliament and of the Council of November 6, 2001 on Community code relating to medicinal products for human use. It was noted that states should establish a system for the accreditation of tissue establishments and a notification system for incidents and adverse reactions related to: downloading, testing, processing, preservation, storage and distribution of tissues and cells. States belonging to the European Union should also organize an inspection and take control measures by officials representing the competent authority to ensure that that tissue and cell establishments comply with the provisions of the directive.
The directive indicates that personnel directly involved in the tissue donation, tissue retrieving, testing, processing, preserving, storage and distribution of human tissues and cells must be properly qualified and guaranteed periodic appropriate training. It was indicated that an appropriate system should be established to allow monitoring of human tissues and cells. It should also allow for verification in relation to quality and safety standards. The monitoring system should be implemented by developing operational procedures for identification of the donor and recipient. These procedures ensure full identification any materials used in tissue establishments and cells. The scope, method and time of storage require defined documentation and implementation of an appropriate system for the labeling of transplants. The identity of the recipient(s) and the donor or the donor's family should not be disclosed. The issues mentioned must comply with the legislation in force in a Member State. In exceptional situations, in the case of donating reproductive cells, it is acceptable to cancel the donor's anonymity. For more effective enforcement in accordance with the directive, there are penalties to be used by individual states of the community. Member States should share their scientific data relating to the safety of tissues and cells, in particular to assist the Commission with its adaptation of the provisions of the directive for scientific and technical progress, in light of the rapid development of biotechnological knowledge, and proceedings in the field of human tissues and cells.
The “Transplantation Act” consists of 59 articles, grouped together in 12 chapters. A brief description of the Act is presented in Table 1.
Briefly the “Transplantation Act” determines that the method of expressing consent to the retrieval of tissues and organs after death in Poland happens by not expressing an objection during life (opt-out system). An interview with the family is required in the manner of the donor’s rejection and risk behavior verification. It is not possible to demand payment or financial benefit for the collected tissues and organs. However, the reimbursement of costs incurred during the retrieval is not a payment. For the purpose of procurement, collection, processing, sterilization, etc., of tissues a tissue bank is set up. The tissue bank sets up a donation team headed by a medical doctor. Members of the donation team who are not medical doctors should have a medical, biotechnological or biological education, and should be trained.
In addition, many issues relevant to transplantation are included in the implementing acts to which it refers in its content law. In the particular manner of tissue retrieval (with specific estimation of skin retrieval) the Regulation of the Minister of Health of October 26, 2018 on the detailed conditions for the procurement, storage and transplantation of cells, tissues and organs deserves special attention. This legal act regulates and determines what professional qualifications should be possessed by a person performing activities related to the collection and transplantation of cells, tissues and organs. In brief, to proceed on tissue retrieval from a deceased donor one should be a medical doctor, dentist or trained member of a donation team (that is not a medical doctor or dentist). In that case the retrieval must be supervised by the doctor (head of donation team). Tissue banks and donation teams are subjected to National Centre for Cell and Tissue Banking in Warsaw, Poland.
Another important legal act is the Regulation of the Minister of Health of 16 December 2020 amending the regulation on the detailed method of determining the costs of activities related to the collection, storage, processing, sterilization and distribution of cells, tissues and organs. In brief, the costs related to the skin retrieval have been set at 31 PLN/100 cm2 of donated skin (6.6878 €/100 cm2; 1 € = 4.6353 PLN, exchange rate according to the National Bank of Poland on March 28, 2021). The costs related to the cosmetics of the donor after skin retrieval have been set at 44 PLN (9.4923 €). The costs related to the donor consultation/qualification before the retrieval have been set at 140 PLN (30.2030 €).
Educational schemes and awareness campaigns
The proposal for a society awareness campaign was established initially. A number of plastic works on the subject related to transplantation were made. Figure 2 shows one of the most serious reasons for a family's refusal—fear of disfiguring the body. The figure in an amusing way attempts to convey the information that after tissue retrieval there will be no disfigurement or defecation of the body. Figure 3 shows the modification of the symbol regarding the disposal of waste. In the figure, the waste element has been replaced with the image of an organ (e.g. heart) that has been thrown into the garbage. The presented situation is clearly defined as negative and accompanied by a comment that makes people aware of the possibility of tissue and organ transplantation.
A proposal for a promotional poster as part of an awareness campaign. The picture is modeled on a school assignment and depicts two identicalimages of a small, smiling vampire. The purpose is to raise awareness in a fun way that the removal of tissues and organs does not leave any visible signs of disfigurement. Our own creation, based on a free vector downloaded from the website: www.freepik.com
A proposed promotional poster as part of an awareness campaign. The picture is modeled on the actions promoting waste segregation and recycling, the “zero waste” attitude. Our own creation, based on a free vector downloaded from the website: www.freepik.com
Another poster proposal is presented in Fig. 4. The figure shows a modified infinity symbol with an integrated heart symbol. The whole is accompanied by a commentary informing about the need and the possibility of giving someone a chance for a new life.
The necessity to cooperate with journalists, celebrities and influencers was indicated. Cooperation with the above may have a positive impact on the improvement of the positive reception of transplantology by society.
Additionally, the awareness raising campaign has been prepared and conducted for the students of emergency medical services at the WSB Academy in Dąbrowa Górnicza, Poland. The campaign took place as part of two four-hour meetings with an expert. The success of these classes inspired the university authorities to introduce a new subject for Medical Rescue studies, entitled Transplant Procedures.
An additional education scheme was initially proposed for medical specialists (TCs, intensivists etc.) concerning skin donation. An educational video was created depicting the skin donation process. The video, shown during TC training, is intended to convince the specialists that skin retrieval does not cause the disfiguration of the body and does not influence the presence of the body during the funeral. That should help the professionals talking to families (transplant coordinators), to convince them to consent for skin donation.
There was a proposal for a poster (Fig. 5) that could be located in ICUs, hospital corridors, the offices of doctors or TCs etc. The poster depicts a graph showing the difference between available organs for transplant and clinical need. A significant difference between the access to these organs and the demand for them was indicated. At the same time, a clear message was made that it is up to healthcare professionals to improve this disadvantage (Fig. 5).
Additionally, a presentation has been created concerning the treatment of severely burned patients, to be presented during scientific conferences, transplant training sessions and workshops, educational projects, etc., starting from September 2021. This should raise the awareness among TCs of the role of allogeneic skin graft materials in the treatment of burn wounds.
Systemic changes—prospects to increase the skin donation ratio
The analysis of the data obtained from POLTRANSPLANT and National Centre for Cell and Tissue Banking in Warsaw revealed that in 2018 a total of 496 multiorgan donations (MODs) were procured. In 2019 a total of 504 MODs were procured. And in 2020 a total number of 529 MODs were procured.
In 2020 a total of 54 skin donations were procured in Poland (22 donations during MODs and 32 donations during tissue procurements). In order to show some disproportion, in 2020 a total of 744 corneal donations were performed (337 during MODs and 407 with tissue-only donors).
Systemic solutions like the appointment of a central procurement team to collect tissues is proposed. Such a team would be under the auspices of the National Center for Tissue and Cell Banking in Warsaw (KCBTK). The central procurement team would then be divided into regional teams. Initially, it is planned to establish 6 such teams. Ultimately, it could be planned to appoint 16 teams, so that in each of the 16 Polish voivodeships there would be an active procurement team collecting tissues. Tissue retrievals will be performed during multi-organ donations (MOD) or during applicable only-tissue donations organized by specific hospitals throughout Poland. Additionally the tissue procurement will take place in forensic medicine facilities, mortuaries, funeral homes and other legally authorized entities. It should be emphasized that the procurement teams will retrieve various tissues. Thus, the collected material will be sent to distant tissue banks by means of specialized medical transport immediately after the procurement, along with the accompanying medical documentation. An exemplary workflow is shown in Fig. 6.
The scheme of collaboration between multiple regional tissue procurement teams and various tissue banks. a An example of a situation in which the procurement team performed the tissue retrieval in northwestern Poland and then transferred the appropriate tissues to specialized, distant tissue banks, for example skin. b An example of a situation in which the procurement team performed the tissue retrieval at the forensic medicine department (ZMS) and then transferred the collected tissues to specialized, distant tissue bank
There is no medical profession of tissue banker. Another systemic solution could be to establish such a profession. A tissue banker should be allowed to perform a tissue donation from a deceased donor (as a member of a team) without any additional supervision. A specifically experienced and trained tissue banker should be allowed to lead a donor team and be allowed to consult/qualify the deceased donor for tissue retrieval. Such solutions would ease and help to avoid some particular formal problems that occur at present. These solutions would lead to an increase in skin donations, etc. Currently, a physician has to be the head of a tissue procurement team, whereas 1 in 20 anonymously asked physicians stated that they had the time or will to participate in the tissue donating process. By basing the tissue donation system on only physicians impairs the whole process.
Good cooperation with transplantation centers (hospitals) and forensic facilities should be maintained.
It could be proposed that every MOD should end with multi tissue retrieval. What is more, each deceased patient could be a potential tissue donor.
Increasing the costs and investments in transplantation may lead to an increase in the number of donations.
Possible methods of achieving a strategic stock of human skin graft materials
The implementation of the above potential solutions and proposals could result in an increase in the number of actual retrievals:
Increase in society’s awareness;
Increase in awareness and education of medical professionals (TCs, intensivists etc.);
Set up the medical profession of Tissue Banker;
Tissue Banker/donation team member allowed to consult deceased donor and retrieve tissues;
Tissue retrieval should be processed for all multiorgan donations and in forensic facilities (where applicable).
Tissue retrieval should be processed for all tissue retrieval in all cases of hospital death (where applicable).
As presented in Sect. 4.2, the analysis of the number of skin donations made by the CLO donation team in the years 2009–2020 showed that during this time a total of 456 retrievals (including forensic facilities and multiorgan donations) were processed with a total area of 1,946,177.5 cm2 collected, an average of 183,389.00 cm2 per year. At that time, the total area of transplanted skin graft materials was 1,829,758.5 cm2 (yearly average of 152,479.88 cm2). The difference between the average annual income and the average annual expenditure of skin graft materials was 30 909 cm2 (Fig. 1).
The presented data may suggest that a significant increase in the number of skin donations is necessary in order to create a strategic skin graft stock.
However, there are certain factors that can further adversely affect the process, reducing the number of donors and procurements. One such factor may be the time limit that is required from the death of a potential donor to the time of tissue donation. The time depends on the necessary activities related to the proper qualification of the donor for tissue retrieval. Thus, the time required to coordinate the procurement, i.e. to perform appropriate diagnostic tests, possible donor transport and an interview with the family/relatives of the deceased, can be considered a key element. However, it should be taken into account in this context that the listed activities (e.g. interview with the family) are obligatory elements of the coordination of any donation. And they always took place in a limited time regime. In a situation where the specific time frame for a given type of tissue is too short, the only possible solution would be to propose an extension of the time limit for performing tissue donation. However, it should be very clearly emphasized that this solution would be possible only on the condition of performing a validation on the basis of which it was unquestionably proven that the collected tissue material has the appropriate and required biological and mechanical properties.
Tissue establishment employee profile
An employee profile has been proposed for tissue establishments. A tissue bank employee (assistant) is a person who:
has higher education—medical (including physicians, nurses, paramedics), biological or biotechnological; has thorough knowledge of medical sciences, especially in the field of anatomy and histology as well as cell biology and received appropriate training in the principles of conduct in clean rooms, practical and legal rules for the eligibility of donors or other equivalent training required by law to allow proper movement within clean rooms and a theoretical basis for performing such activities as, for example, preparation of tissue transplants, in vitro culture of human cells, or the collection of specific tissues from human cadavers. These activities are performed in terms of the principles of the quality assurance system. The employee should know and understand the principles of occupational health and safety, in particular working with biological material—potentially infectious. Should have knowledge in the field of quality assurance; be able to perform a risk analysis for specific processes and propose conclusions resulting from this analysis. The employee must complete and scrupulously maintain medical and work-related documentation in the clean room. The employee should be able to plan and possibly carry out specific works related to the qualification of rooms and devices and the required validation activities. In addition, the employee should have the necessary knowledge of the legal basis of work in a tissue bank. An employee of a tissue bank should have the necessary knowledge in the field of pharmaceutical law regarding Good Manufacturing Practice (GMP). In this situation, a tissue bank employee should be ready to make an additional effort to improve his or her professional qualifications.
shows constant readiness to improve their qualifications; especially to take part in appropriate training, postgraduate studies, specializations and research work. In addition, an employee of a tissue bank should be constantly prepared to seek new methods of processing cell and tissue material and to improve these methods. The tissue bank assistant should be ready to present scientific and practical achievements during national and international scientific conferences. The tissue bank assistant should be ready to publish the obtained results of scientific work in domestic and foreign trade journals, with particular emphasis on journals with a good impact factor (IF) in order to constantly update knowledge in field of tissue donation and preparation.
Possible methods of logistic management of the allogeneic skin stock
The development of a computer program to indicate (in advance) the expiry date of transplants, and therefore which should be used first (basic stock of allogeneic skin graft materials, leaving it intact).
Despite the CLO transplant team being available 24 h/7 days a week, the analysis of the needs of employment show that there would be a need for donation teams working a 3-shift system. This means that at least two additional employees must be employed as members of the procurement team. Under this assumption, the tissue bank would have three employees ready for multi-organ donations. In this case, it would also be possible to replace individual team members if he or she were not ready to start. In addition, if two or three MODs or other types of donation (e.g. forensic etc.) were to take place at the same time, the team would be able to handle them. The assumption is that these two new employees would also take an active part in the production of transplants. According to this assumption, the number of skin retrievals would be 1–3 per day. If the number of skin retrievals reached a higher number, it would be necessary to hire additional staff. At this point, it should be additionally noted that the CLO tissue bank currently employs an appropriate number of trained employees who can also participate in the MOD and perform skin preparation. The assumption includes the preparation of at least four skin donations a day. Of course, there should be no doubt that this is an immediate and temporary solution. The CLO procurement team, even with an increased number of employees, will not be able to take part in the retrievals which takes place in Poland in a distant regions from the CLO. In this approach, all necessary steps should be taken to establish a central procurement team that would be divided into several smaller, regional teams. In this way, regional procurement teams will be able to perform tissue retrievals in distant locations in Poland. Therefore, material collected in remote places in the country will go to the appropriate tissue establishments.
An analysis of the CLO equipment showed that there was enough of the required devices (dermatomes) and clean rooms. The need was proposed to purchase additional equipment like small surgical tools (scissors, tweezers, peans, blankets etc.) and trolleys/bags for tools and low temperature freezers. If the number of skin procurements increases, then building a new facility will be considered.
The majority of tissue establishments in Poland are public organizational structures or operating on a non-profit basis. Most of them are public or university hospital-based tissue banks, often associated with the surgical department they supply. The tissue they handle is often only distributed in that hospital and sometimes to other hospitals in the region. The costs of these activities are difficult to distinguish from the budget of the hospital in which a given tissue establishment is located. This often leads to limited cost-awareness of the real costs of a tissue bank and inadequate price-setting processes for skin graft material preparation and distribution. The cost generating factors for a tissue bank, such as additional national requirements on safety and quality including donor screening, testing or processing, additional legal frameworks for medical devices on replacement tissues, regulatory quality requirements on premises and equipment or complicated administrative procedures, are often thresholds, expensive and impossible to overcome, especially for small-scale public poor-funded tissue establishments with limited resources. The prices of donor procurement and testing are often fixed at the national level and do not necessarily reflect the real costs. In terms of operational costs there are four general cost-objects, including donation, testing and screening, processing and distribution. Post-mortem skin donations generate expenses for logistics, salary costs for procurement personnel, virology testing etc. Specifically for a post mortem skin donation it is important to procure a sufficient area of skin to cover those costs by the distribution of allografts after processing. The CLO Tissue Bank indicated that they strive for 6000 cm2 per donor to make the donation feasible. The skin tissue sector is also subject to continuous technological innovation and the consequences of changing economics and organizational setups. All these cost-generating factors prevent tissue establishments not only from growing their activities and expanding their tissue supply to a larger area, but even from achieving the required financial break-even point. Therefore, in order to promote skin transplantation and assist tissue banks at the operational level, a contribution is required through grants or financial injections by public actors or government, such asthe National Program for Transplantation Medicine Development 2021–2030.
Additionally, signing agreements with other tissue establishments may be considered, where transplant teams from other units could collect skin for the CLO tissue bank. This can be advantageous, especially for MODs organized in locations distant from the CLO. In addition, the CLO transplant team could then harvest tissues other than skin and donate them to a specific other tissue establishment.
In addition, closer cooperation with a second skin bank in Poland (KCBTK in Warsaw) should be established. In this situation, the transfer or replacement of transplants would become significantly more efficient.
Communication management strategy
The communication management strategy was created to ensure optimal information flow, e.g. regarding the risks associated with the creation and provision of the planned amount of allogeneic skin. The stakeholders include:
Director of the facility—Mariusz Nowak, MD, PhD;
Doctors responsible for the clinical implementation of products in CLO—skin recipient;
External hospital—skin recipient on the basis of an agreement;
External hospital—skin retrieval during MOD;
Ministry of Health;
Poltransplant;
National Center for Tissue and Cell Banking;
CLO transplant team;
Forensic medicine transplant team;
Supplier of bags for packing transplants;
ICHiTJ—transplant sterilization according to contract;
Hospital pharmacy—products for preparation;
Microbiological laboratory responsible for testing the quality of the product;
Analytical laboratory responsible for donor research;
Cleaning maintenance team;
Person from the technical department dedicated to assist in the validation/qualification of equipment, rooms and installations;
External companies to qualify equipment;
A company responsible for the qualification of the rooms in the preparation rooms.
Identified stakeholders will be subject to a risk assessment, assessed in terms of probability and impact (Table 2). Risk identification will take place both during the planning and implementation of the project.
Risks with the value ≥ 10 (red in the matrix—Table 2) are critical and will be reduced or removed. For individual risks, reactions have been defined, and reflected in the plans (Table 3).
The risks recognized in the field of permits, contracts and financing were analyzed, see Table 4. Despite their low probability, the possible consequences would be catastrophic.
A similar situation was observed with the risks identified in the production process listed in Table 5. Despite the low probability of the risks, their possible consequences would be catastrophic.
Identified risks in documentation and quality, presented in Table 6 also would be unlikely to happen, although the consequences would be catastrophic.
The risks identified in the area of qualification and validation, presented in Table 7, would bring the same effect.
The planned counteracting of the above-mentioned unfavorable phenomena should be based on risk reduction. The meaning of specific, possible actions to be taken to manage the risk (e.g. avoidance, reduction etc.) has been presented in Table 3. Activities aimed at reducing the identified risks may include supervision over concluded contracts, adequate compliance with procedures, compliance with the requirements resulting from the quality assurance system, appropriate supervision over clean rooms, laboratory equipment and documentation.
Discussion/conclusion
The main goal of the study was to prepare applicable prospective solutions for the creation of a strategic stock of human allogeneic skin graft materials in terms of a mass casualty event (e.g. mass burn casualty disaster). The definition of amass casualty event could be understood as an emergency with a greater number of victims than can be accommodated by the rescue services and their supplies. A mass burn casualty disaster could be defined as proposed by the American Burn Association (ABA) as “any catastrophic event in which the number of burn victims exceeds the capacity of the local burn center to provide optimal burn care.”The term ‘capacity’ includes the availability of burn beds, burn surgeons, burn nurses, other support staff, operating rooms, equipment, supplies, and related resources (Haller et al. 2017), which could include a suitable amount of material for human allogeneic skin graft materials.
Historically the phrase mass burn casualty disaster included radiation injuries, terrorist attacks, indoor fires, club/disco fires, transport accidents, chemical burns, explosions (including industrial) etc. (Allister and Hamilton 1983; Seifman et al. 2011; Kumar 2013; Kearns et al. 2014; Carlson et al. 2015; Koning et al. 2015; Zhang et al. 2015; Konwinski et al. 2016; Ozoilo et al. 2010; Haller et al. 2017; Sheridan et al. 2017; Ewbank et al. 2019; Hunt, 2017; Chen et al. 2019; Haverkamp et al. 2019; Lin et al. 2019; Tseng et al. 2019; Parrish and Seda 2019; Yang et al. 2019; DiCarlo et al. 2020). From recent history in Poland, mass burn casualty disasters included mainly accidents in the carbon mines located in the Śląskie Voivodship (Southern Poland).
Many authors have emphasized that the allogeneic human skin graft materials collected from a deceased donor play significant role in the therapy of heavily (extensive and deeply) burned casualties of a mass catastrophe (Brown and Fryer 1954; Horner et al. 2013). Additionally, it could be remarked that human allogeneic skin graft materials may be the source of the collagenous biomaterials that are produced and evaluated in terms of tissue engineering. Such products include acellular dermal matrix ADM, which could serve as the scaffold for in vitro cultured specific cells (e.g. autologous keratinocites, fibroblasts or allogeneic mesenchymal stem cells MSC). In that manner one could obtain a viable skin substitute as an alternative to autologous skin graft materials. This would be especially advantageous in the treatment of severely burned patients (Łabuś et al. 2015, 2018, 2020; Kitala et al. 2020). To emphasize the important role of human allogeneic skin transplants in the treatment of burn patients, reference can be made to the guidelines of the European Burn Association (EBA). One of the EBA recommendations is that any burn treatment unit or ward should have an access to a skin bank (Moiemen 2017). In accordance to that approach, skin banks may be considered one of the key institutions in the treatment of severely burned patients. In that manner it may be accepted that the main requirement for a skin bank is to provide the required amount of allogeneic human skin graft materials for normal, everyday clinical routine work as well in the case of a mass disaster.
The analysis of the historical mass burn disasters that occurred in Polish carbon mines revealed a serious deficit in materials for allogeneic human skin grafts and amnion grafts. To avoid such undesirable and dangerous situations in the future, the creation of a stock of allogeneic human skin graft materials should be considered.
Further analysis of the Polish mine disasters revealed that the average number of victims was 11, with an average burn area of approx. 56% TBSA. It may be remarked that an average TBSA of more than 50% is characteristic for mass burn disasters, as reported by many authors (Allister and Hamilton 1983; Seifman et al. 2011; Kumar 2013; Kearns et al. 2014; Carlson et al. 2015; Koning et al. 2015; Zhang et al. 2015; Konwinski et al. 2016; Ozoilo et al. 2010; Haller et al. 2017; Sheridan et al. 2017; Ewbank et al. 2019; Hunt 2017; Chen et al. 2019; Haverkamp et al. 2019; Lin et al. 2019; Tseng et al. 2019; Parrish & Seda 2019; Yang et al. 2019; DiCarlo et al. 2020). According to that data the approximate burn area for the model profile of a burn casualty was estimated at 60% TBSA. The number of casualties was estimated at 30 hospitalized patients, additionally it was assumed that such patients would require approx. 10,000 cm2 of allogeneic skin graft materials and would require skin grafts twice. In relation to the above assumptions, it was assumed that the minimum, inviolable stock of human allogeneic skin graft materials should be 600,000 cm2.
According to the data concerning the number of skin retrievals during multiorgan donations procured in Poland it seems clear that in the present situation there is no possibility to create the assumed stock. The goal would not be possible even if the forensic medicine skin retrievals were taken into consideration. There should be no doubt that the primary and essential solution to this disadvantageous situation is to significantly increase the number of skin retrievals (taken place during MODs and during forensic retrievals). An analysis of the average annual allogeneic skin graft materials income and utilization revealed that the average annual leftover of allogeneic skin graft materials is 30,909 cm2 (Fig. 1). In this manner the achieving of the assumed stock of 600,000 cm2 would take about 20 years. It could be concluded that a significant increase in the number of skin retrievals is required, and it could also be hypothesized that to increase the number of skin retrievals would require strong political and legal support.
In this particular manner the significant gap between the number of skin procurements and corneal button/whole eye procurements is worthy of remark. The thesis could be proposed that in both cases, the public perception of skin and eye tissue collection may be considered controversial. However, the number of eye tissue samples is significantly higher. According to POLTRANSPLANT the number of corneal retrievals was 744 while the number of skin donations was 54 in 2020. A probable explanation of this phenomenon can be found in the higher awareness and knowledge of eye tissue harvesting techniques among Polish transplant coordinators. From this it can be concluded that, despite the different assumptions of the applicable law, families often decide which tissues and organs will be procured.
The analysis of Polish legal regulations revealed that the valid form of consent for donation after death is the opt–out system. Theoretically the opt–out system in Poland assumes that the only binding form of consent is the decision of the deceased donor expressed during his or her lifetime. Any conversation with the deceased's family would only serve to confirm that will. In practice during the interview with the family, the members often decide which organs or tissues may be retrieved (data not shown). However, it should be clearly emphasized that the percentage of family refusals has not exceeded 10% for several years (Czerwiński et al. 2020). However, this situation should be termed a “soft opt–out system”, even though the Polish legal guidelines do not provide for such situation, and it might be considered a movement towards a good solution (empathy and understanding towards family mourning and regret is a primary attitude of TCs). On the other hand, families often reject skin donation, despite agreeing to corneal donation. Data from POLTRANSPLANT and KCBTK confirms this situation. The fact that the number of corneal retrievals was 744 while the number of skin donations was 54 in 2020may relate to the thesis that skin retrievals have an extremely negative connotation, concerning partly the fear of the body disfigurement. One possible solution to this negative outcome is the proposal for more intensive training and education schemes for TCs, and a long-term awareness campaign for society.
Some proposals have been presented in relation to this. One is that posters could be used to increase awareness of members of society and medical professionals (Figs. 1, 2, 3, 4). In accordance with the individual capabilities of the author, educational lectures for physicians, paramedics and cosmetologists have taken place.
In accordance with the form of consent, some authors would agree that opt-out or presumed consent would increase the rate of the donations in those countries that changed their regulations from opt-in to opt-out (Saab et al. 2019). It should be noted that Poland’s donation ratio increased after implementing that form of consent (Saab et al. 2019); however, there are many countries in the world with a valid opt-in system and with much better outcomes, e.g. the USA. From this it might be concluded that the type of consent is not the most important element of success, which finds compliance in the work of Ezaz and Lai (2019). The authors conclude that although opt-out consent may bring better outcomes, it is not some kind of “gold standard” to solve all potential problems (Ezaz and Lai 2019). In this specific manner it could be added that our research showed that Polish society is characterized by a positive attitude towards the idea of donation and transplantation (approx. 90%), even though the level of specialized knowledge is low (data not shown). That finding may lead to the conclusion that educational awareness campaigns are required.
Another important issue concerning Polish law is the issue of rights to retrieve the tissues from a deceased human donor. At present only a physician or a dentist is allowed to lead a retrieval team. Although a member of that team (not a physician) is allowed to collect the tissues, all the actions must be supervised by the head of the team. As well as the needing the qualification of the donor, the shortage of physicians who would be willing to participate in tissue donation may be a serious impediment. One proposed solution is to include an extension to the rights of a team member (right to retrieve without supervision, right to qualify the donor, right to lead the team). Being the head of the team could require 2–5 years of experience in tissue donations or a PhD in the field of tissue banking. Additionally, the establishment of a new medical profession: “tissue and cell banking technologist” would probably be necessary. Such a profession would also require an official commission to award the specific rights and obligations (as in other medical professions).
Additionally, in accordance with a donor qualification prepared by a non-physician retrieval team member, it should be strongly emphasized that all medical documentation and data concerning the donor should be collected and prepared according to the highest standards. In this way the responsible TE person or the TE physician could make the final qualification of the donor without any doubt.
The establishment of a sufficient number of retrieval teams that would be able to take part in every multiorgan donation to retrieve the skin and other tissues should be considered. Such teams would consist of several members (e.g. two). Each team would be available 24 h/7 days per week, according to a timetable. In this situation the special role of TCs should be emphasized. A TC should have adequate knowledge of the nature of tissue procurement, with particular emphasis on the skin. In such a situation, the TC would be able to provide the deceased's family with all the necessary information, including dispelling any doubts related to, for example, disfigurement of the corpse due to tissue collection. Another important issue would be the preservation of a blood sample for the tissue bank. As mentioned before, some additional educational schemes could be proposed, and in that particular aspect the “Spanish model” should be taken into consideration (Matesanz et al. 2017).
Additionally, tissue retrieval protocols could be extended for every deceased patient in each hospital. In that potential manner every deceased person would be treated as a deceased potential donor. After proper qualification a tissue retrieval could take place. In such case the specific monitoring of deceased donors should be provided. Such patients should be monitored and recorded in some electronic central database by the hospital TC.
There is no doubt that all the proposed solutions require strong financial, legal and political support. In that manner the financial cost issue is very often taken into consideration. Despite the costs included in the regulation of the minister of health as the main disadvantage, the situation of concern (mainly for physicians) is that only after actual retrieval can payment be achieved. There is a proposal for the inclusion of some kind of readiness fee.
However, it could be concluded that to achieve the strategic stock of human allogeneic skin graft materials a significant increase in the skin retrievals ratio is vital. This could include the procurement of skin from every multiorgan donor and procurement from every eligible deceased patient (including forensic medicine facilities). To achieve that, the TCs and other persons included in the transplant procurement system should be optimally trained and educated to perform a suitable interview with the family to resolve all the doubts concerning, for example, disfigurement of the body after skin retrieval.
Such a significant increase in the number of skin retrievals would require an increase in the number of retrieval teams. That would necessitate an increase in the employment of professionals ready to take part in donation trips, often distant and time-consuming. In that manner there should be no doubt that most of the retrieval teams would consist of members who are not medical doctors. In order to improve their work, they should be granted an additional professional qualification (e.g. the right to independently qualify a donor and perform retrieval).
The significant increase in donated skin graft materials would require an increase in skin bank employment and device supply (e.g. low temperature freezers, laminar air flow chambers etc.). The possible necessity of building a new facility (skin bank) should also be taken into consideration.
The proposed solutions to increase skin retrieval from deceased donors and eventually to the creation of a strategic stock of human allogeneic skin graft materials would require the strong support at the legal, financial and political levels.
It could be concluded that:
Every medically acceptable multiorgan donor and deceased patient should become a tissue donor (including skin);
Tissue retrieval teams should be appointed;
Rights and duties of a team member (not a doctor) could be extended;
Necessary facility and equipment requirements should be provided;
Educational programs and awareness campaigns should be continued;
Political support would be required as some changes in legislation may be needed;
Financial support would be required to cover the costs resulting from the above assumptions.
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Allister C, Hamilton GM (1983) Cardowan coal mine explosion: experience of a mass burns incident. Br Med J (clin Res Ed) 287(6389):403–405. https://doi.org/10.1136/bmj.287.6389.403
Borys B, Majkowicz M (2004a) Psychological changes in the victims of the Gdańsk Shipyard hall fire in the period of 1995–1999. Psychiatria Polska 38(4):661–671
Borys B, Majkowicz M (2004b) Coping with stress in those who experienced a traumatic situation. Psychiatria Polska. 38(4):651–659
Busuioc CJ, Popescu FC, Mogoşanu GD, Pârvănescu H, Streba L, Mogoantă L (2012) allograft. Rom J MorpholEmbryol 4:1061–1067
Brown JB, Fryer MP (1954) Postmortem homografts to reduce mortality in extensive burns: early biological closure and saving of patients for permanent healing; use in mass casualties and in national disaster. J Am Med Assoc 156(12):1163–1166. https://doi.org/10.1001/jama.1954.02950120037011
Carlson LC, Rogers TT, Kamara TB, Rybarczyk MM, Leow JJ, Kirsch TD, Kushner AL (2015) Petroleum pipeline explosions in sub-Saharan Africa: a comprehensive systematic review of the academic and lay literature. Burns 41(3):497–501. https://doi.org/10.1016/j.burns.2014.08.013
Chen HC, Wu KP, Yen CI, Hsiao YC, Yang SY, Yang JY, Chang SY, Chuang SS (2019) Management of major burns in 37 casualties of a colored powder explosion: experience of the Linkou Burn Center in Taiwan. Ann Plast Surg 82(5):512–519. https://doi.org/10.1097/SAP.0000000000001928
Czerwiński J, Malanowski P, Grzywacz A, Łęczycka A (ed.) (2020) Poltransplant Biuletyn Informacyjny 1
DiCarlo AL, Bandremer AC, Hollingsworth BA, Kasim S, Laniyonu A, Todd NF, Wang SJ, Wertheimer ER, Rios CI (2020) Cutaneous radiation injuries: models, assessment and treatments. Radiat Res 194(3):315–344. https://doi.org/10.1667/RADE-20-00120.1
Ewbank C, Gupta S, Stewart BT, Kushner AL, Charles A (2019) A systematic review of oil tanker truck disasters: identifying prevention targets. Burns 45(4):905–913. https://doi.org/10.1016/j.burns.2018.12.010
Ezaz G, Lai M (2019) How the “Opt-In” OPTION optimizes organ donation rates. Dig Dis Sci 64(5):1067–1069. https://doi.org/10.1007/s10620-019-05483-z
Glik J, Kawecki M, Kitala D, Klama-Baryła A, Łabuś W, Grabowski M, Durdzińska A, Nowak M, Misiuga M, Kasperczyk A (2009) A new option for definitive burn wound closure—pair matching type of retrospective case-control study of hand burns in the hospitalised patients group in the Dr Stanislaw Sakiel Centre for burn treatment between 2009 and 2015. Int Wound J 14(5):849–855
Grossova I, Zajicek R, Kubok R, Smula MC (2017) The treatment of palmar contact burns in children: a five-year review. Ann Burns Fire Disasters. 30(1):5-8
Haller HL, Wurzer P, Peterlik C, Gabriel C, Cancio LC (2017) Burn Management in Disasters and Humanitarian Crises. In Herndon DN. Total Burn Care, 5th Edn. Elsevier
Haverkamp FJC, van Gennip L, Muhrbeck M, Veen H, Wladis A, Tan ECTH (2019) Global surgery for paediatric casualties in armed conflict. World J Emerg Surg 9(14):55. https://doi.org/10.1186/s13017-019-0275-9
Horner CW, Crighton E, Dwiewulski P (2013) Challenges in the provision of skin in the UK: the use of human deceased donor skin in burn care relating to mass incidents in the UK. Cell Tissue Bank 14(4):579–588. https://doi.org/10.1007/s10561-013-9374-0
Hughes A, Almeland SK, Leclerc T, Ogura T, Hayashi M, Mills JA, Norton I, Potokar T (2021) Recommendations for burns care in mass casualty incidents: WHO emergency medical teams technical working group on burns (WHO TWGB) 2017–2020. Burns 47(2):349–370. https://doi.org/10.1016/j.burns.2020.07.001
Hunt P (2020) Lessons identified from the 2017 Manchester and London terrorism incidents. Part two: the reception and definitive care (hospital) phases. BMJ Mil Health. 166(2):115–119. https://doi.org/10.1136/jramc-2018-000935
Iijima S (1982) Pathology of atomic bomb casualties. Acta Pathol Jpn 32(Suppl 2):237–270 (PMID: 7187578)
Kamolz LP, Schiefer JL, Horter J, Plock JA (2020) COVID-19 and burns: Lessons learned? Burns 46(6):1467–1468. https://doi.org/10.1016/j.burns.2020.05.015
Kearns RD, Holmes JH 4th, Skarote MB, Cairns CB, Strickland SC, Smith HG, Cairns BA (2014) Disasters; the 2010 Haitian earthquake and the evacuation of burn victims to US burn centers. Burns 40(6):1121–1132. https://doi.org/10.1016/j.burns.2013.12.015
Kitala D, Kawecki M, Klama-Baryła A, Łabuś W, Kraut M, Glik J, Ryszkiel I, Kawecki MP, Nowak M (2016) Allogeneic vs. autologous skin grafts in the therapy of patients with burn injuries: a retrospective, open-label clinical study with pair matching. Adv Clin Exp Med 25(5):923–929
Kitala D, Łabuś W, Klama-Baryła A, Kraut M, Maj M, Szapski M (2020) Application of amniotic stem cells on an acellular dermal matrix scaffold in a burn patient: a case report. Transplant Proc 52(8):2563–2569. https://doi.org/10.1016/j.transproceed.2020.01.110
Koning SW, Ellerbroek PM, Leenen LP (2015) Indoor fire in a nursing home: evaluation of the medical response to a mass casualty incident based on a standardized protocol. Eur J Trauma Emerg Surg 41(2):167–178. https://doi.org/10.1007/s00068-014-0446-z
Konwinski RR, Singh A, Soto J (2016) Imaging of lower extremity trauma from Boston Marathon bombing. Emerg Radiol 23(5):433–437. https://doi.org/10.1007/s10140-016-1414-1
Kumar P (2013) Fire disaster following LPG tanker explosion at Chala in Kannur (Kerala, India): August 27, 2012. Burns 39(7):1479–1487. https://doi.org/10.1016/j.burns.2013.04.004
Leclerc T, Potokar T, Hughes A, Norton I, Alexandru C, Haik J, Moiemen N, Almeland SK (2021) A simplified fluid resuscitation formula for burns in mass casualty scenarios: analysis of the consensus recommendation from the WHO emergency medical teams technical working group on burns. Burns. 27:S0305–4179(21)00058–9. https://doi.org/10.1016/j.burns.2021.02.022
Lin CH, Lin CH, Tai CY, Lin YY, Shih FF (2019) Challenges of burn mass casualty incidents in the prehospital setting: lessons from the formosa fun coast park color party. Prehosp Emerg Care. 23(1):44–48. https://doi.org/10.1080/10903127.2018.1479473
Łabuś W, Kitala D, Klama-Baryła A, Szapski M, Smętek W, Kraut M, Poloczek R, Glik J, Pielesz A, Biniaś D, Sarna E, Grzybowska-Pietras J, Kucharzewski M (2020) A new approach to the production of a biovital skin graft based on human acellular dermal matrix produced in-house, in vitro revitalized internally by human fibroblasts and keratinocytes on the surface. J Biomed Mater Res B Appl Biomater 108(4):1281–1294. https://doi.org/10.1002/jbm.b.34476
Łabuś W, Glik J, Klama-Baryła A, Kitala D, Kraut M, Maj M, Nowak M, Misiuga M, Marcinkowski A, Trzebicka B, Poloczek R, Kawecki M (2018) Atomic force microscopy in the production of a biovital skin graft based on human acellular dermal matrix produced in-house and in vitro cultured human fibroblasts. J Biomed Mater Res B Appl Biomater 106(2):726–733. https://doi.org/10.1002/jbm.b.33883
Łabuś W, Kawecki M, Glik J, Maj M, Kitala D, Misiuga M, Klama-Baryła A, Kraut M, Nowak M (2015) Own experience from the use of a substitute of an allogeneic acellular dermal matrix revitalized with in vitro cultured skin cells in clinical practice. Pol Przegl Chir 87(10):513–521. https://doi.org/10.1515/pjs-2015-0097
Moiemen N (2017) European practice guidelines for burn care. European Burns Association. Version 4
Matesanz R, Domínguez-Gil B, Coll E, Mahíllo B, Marazuela R (2017) How Spain reached 40 deceased organ donors per million population. Am J Transplant 17(6):1447–1454. https://doi.org/10.1111/ajt.14104
Ozoilo KN, Amupitan I, Peter SD, Ojo EO, Ismaila BO, Ode M, Adoga AA, Adoga AS (2016) Experience in the management of the mass casualty from the January 2010 Jos Crisis. Niger J Clin Pract 19(3):364–7. https://doi.org/10.4103/1119-3077.179276
Parrish JS, Seda G (2019) Disasters resulting from radiologic and nuclear events. Crit Care Clin 35(4):619–631. https://doi.org/10.1016/j.ccc.2019.06.005
Prim PM, Kim HS, Shapiro LE, Lee JS, Kaan JH, Jackson JD, YooJJ, Atala A, Lee SJ (2017) In vitro skin expansion: Wound healing assessment. Wound Repair Regen. https://doi.org/10.1111/wrr.12550.
Relvas LM, de Oliveira AP. The medical response to burn disasters in Europe: a scoping review. Am J Disaster Med. 2018 Summer 13(3):169–179. https://doi.org/10.5055/ajdm.2018.0298.
Saab S, Saggi SS, Akbar M, Choi G (2019) Presumed consent: a potential tool for countries experiencing an organ donation crisis. Dig Dis Sci 64(5):1346–1355. https://doi.org/10.1007/s10620-018-5388-6
Seifman M, Ek EW, Menezes H, Rozen WM, Whitaker IS, Cleland HJ (2011) Bushfire disaster burn casualty management: the Australian “Black Saturday” bushfire experience. Ann Plast Surg 67(5):460–463. https://doi.org/10.1097/SAP.0b013e3182111021
Sheridan RL, Friedstat J, Votta K (2017) Lessons learned from burn disasters in the post-9/11 Era. Clin Plast Surg 44(3):435–440. https://doi.org/10.1016/j.cps.2017.02.003
Tseng YC, Chen BC, Chen CT, Chou YC, Dai NT, Chen PJ, Huang TY, Shih YL, Chang WK, Hsieh TY, Lin JC (2019) Early Initiation of post-pyloric feeding in patients with major burns: experience in Taiwan Formosa water park dust explosion disaster. Tohoku J Exp Med 247(2):111–118. https://doi.org/10.1620/tjem.247.111
Voigt CD, Williamson S, Kagan RJ, Branski LK (2017) The Skin Bank. In Herndon DN, Total burn care, 5th Edn. Elsevier
Yang CJ, Tsai SH, Chien WC, Chung CH, Dai NT, Tzeng YS, Chen SJ, Wu DC, Chen CJ (2019) The crowd-out effect of a mass casualty incident: Experience from a dust explosion with multiple burn injuries. Medicine (baltimore) 98(18):e15457. https://doi.org/10.1097/MD.0000000000015457
Zhang F, Zheng XF, Ma B, Fan XM, Wang GY, Xia ZF (2015) Mass chemical casualties: treatment of 41 patients with burns by anhydrous ammonia. Burns 41(6):1360–1367. https://doi.org/10.1016/j.burns.2015.02.016
Acknowledgements
This work has been proceeded as the master thesis at the 17th edition of the International Master in Donation & Transplantation of Organs, Tissues and Cells—Barcelona University & Donation and Transplantation Institute DTI (Spain).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. All financing was covered from the statutory funds of Dr. Stanisław Sakiel Center for Burns Treatment, Siemianowice Śląskie, Poland.
Author information
Authors and Affiliations
Contributions
WŁ—study design, manuscript preparation, data collection, data analysis, corresponding author. DK—study design, manuscript preparation, data collection, data analysis. AN—study design, manuscript correction. AKB—manuscript preparation. MK–manuscript preparation, data collection. AS—manuscript preparation. WS–manuscript preparation. AK– study design, manuscript correction.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This research complies with the guidelines for human studies and it was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The Bioethics Committee at the Silesian Regional Medical Chamber in Katowice, Poland waived the need for approval due to the nature of the study as well as the written informed consent obtained from participants (or their parent/legal guardian/next of kin) to participate in the study was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 465503 kb)
Rights and permissions
About this article
Cite this article
Łabuś, W., Kitala, D., Navarro, A. et al. The urgent need to achieve an optimal strategic stock of human allogeneic skin graft materials in case of a mass disaster in Poland. Cell Tissue Bank 23, 863–885 (2022). https://doi.org/10.1007/s10561-022-10001-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-022-10001-z