Abstract
The esophageal Doppler monitor (EDM) is a clinically useful device for minimally invasive assessment of cardiac output, preload, afterload, and contractility. An empirical model, based upon the logistic function, has been developed. Use of this model illustrates how the EDM could estimate the net effect of aortic and non-aortic contributions to inertia, resistance, and elastance within real time. This is based on an assumed mechanical impedance conceptually resembling that of a series arrangement of a spring, mass, and dashpot. In addition, when used with an invasive radial arterial catheter, the EDM may also estimate aortic pulse wave velocity, as well as aortic characteristic impedance, and characteristic volume. Approximations of left ventricular stroke work and stroke power can also be made. Furthermore, the effects of inertia, resistance, and elastance, on mean blood pressure during systole, can be quantified. These additional parameters could offer insight for clinicians, as well as researchers, and may be beneficial in further examining and utilizing clinical hemodynamics with the EDM. These additional measurements also underscore the need to integrate the EDM with existing and future monitoring equipment.






Similar content being viewed by others
References
American Society of Anesthesiologists Task Force on Guidelines for Pulmonary Artery Catheterization. Practice Guidelines for Pulmonary Artery Catheterization. Anesthesiology. 2003;99(4):988–1014.
Atlas G. Can the esophageal Doppler monitor be used to clinically evaluate peak left ventricular dp/dt? Cardiovasc Eng Intl J. 2002;2(1):1–6
Atlas G, Mort T. Placement of the esophageal Doppler ultrasound monitor probe in awake patients. Chest. 2001;119:319.
Beltrami E. Mathematics for dynamic modeling. San Diego, CA: Academic Press; 1987.
Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999;99:2434–39.
Boulnois JLG, Pechoux T. Non-invasive cardiac output monitoring by aortic blood flow measurement with the Dynemo 3000. J Clin Monit Comput. 2000; 16:127–40.
Bove AA, Kreulen TH, Spann JF. Computer analysis of left ventricular dynamic geometry in man. Am J Cardiol. 1978;41(7):1239–48
Bramwell JC, Hill AV. The velocity of the pulse wave in man. Proc R Soc Lond B Contain Paper Biol Charact. 1922;93(652):298–306.
Bulpitt CJ, Rajkumar C, Cameron JD. Vascular compliance as a measure of biological age. J Am Geriatr Soc. 1999;47(6):657–63.
Carney WI, Rheinlander HF, Cleveland RJ. Control of acute aortic dissection. Surgery. 1975;78:114–20.
Chen CH, Nevo E, Fetics B, Pak PH, Yin FCP, Maughan WL, Kass DA. Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure. Circulation. 1997;95:1827–36.
Dark PM, Singer M. The validity of trans-esophageal Doppler ultrasonography as a measure of cardiac output in critically ill adults. Intensive Care Med 2004;30:2060–66.
Davies JI, Band MM, Pringel S, Ogston S, Struthers AD. Peripheral blood pressure measurement is as good as applantion tonometry at predicting ascending aortic blood pressure. J Hypertens. 2003;21:571–6.
De Hert SG, Robert D, Cromheecke S, et al. Evaluation of left ventricular function in anesthesized patients using femoral artery dP/dt(max). J Cardiothoracic Vasc Anesth. 2006;20(3):325–30.
deSimone G, Roman MJ, Koren MJ, Mensah GA, Ganau A, Devereux RB. Stroke volume/pulse pressure ratio and cardiovascular risk in arterial hypertension. Hypertension. 1999;33(3):800–5.
DiCorte CJ, Latham P, Greilich PE, Cooley MV, Grayburn PA, Jessen ME. Esophageal Doppler monitor determinations of cardiac output and preload during cardiac operations. Annl Thorac Surg. 2000;69(6):1782–6.
Dodd TEL. Nasal insertion of the oesophageal Doppler probe. Anaesthesia. 2002;57(4):412.
Domino KB, Bowdle TA, Posner KL, Spitellie PH, Lee LA, Cheney FW. Injuries and liability related to central vascular catheters: a closed claims analysis. Anesthesiology. 2004;100(6):1411–8.
DuBourg O, Jondeau G, Beauchet A, Hardy A, Bourdarias JP. Doppler-derived aortic maximal acceleration: a reliable index of left ventricular systolic function. Chest. 1993;103(4):1064–7.
English JD, Moppett IK. Evaluation of trans-oesophageal Doppler probe in awake patients. Anaesthesia. 2005;60:712–26.
Feldman LS, Anidjar M, Metrakos P, Stanbridge D, Fried GM, Carli F. Optimization of cardiac preload during laparoscopic donor nephrectomy: a preliminary study of central venous pressure versus esophageal Doppler monitoring. Surg Endosc. 2004;18(3):412–6.
Gan TJ, Soppitt A, Maroof M et al. Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology. 2002;97(4):820–26.
Gardin JM, Davidson DM, Rohan MK, Butman S, Knoll M, Garcia R, Dubria S, Gardin SK, Henry WL. Relationship between age, body size, gender, and blood pressure and Doppler flow measurements in the aorta and pulmonary artery. Am Heart J. 1987;113:101–9.
Groenink M, de Roos A, Mulder BJM, Spaan JAE, van der Wall EE. Changes in aortic distensibility and pulse wave velocity assessed with magnetic resonance imaging following beta-blocker therapy in the Marfan syndrome. Am J Cardiol. 1998;82(2):203–8.
Hinghofer-Szalkay H. Method of high-precision microsample blood and plasma densitometry. J Appl Physiol. 1986;60(3):1082–8.
Hopkins KD, Lehmann ED, Gosling RG (1994) Aortic compliance measurements: a non-invasive indicator of atherosclerosis? Lancet. 1994;343(8911):1447.
Hsieh KS, Chang CK, Chang KC, Chen HI. Effect of loading conditions on peak aortic flow velocity and its maximal acceleration. Proc Natl Sci Council Repub China B Life Sci. 1991;15(3):165–70.
Kreyszig E. Advanced engineering mathematics. 8th ed. New York, NY: John Wiley & Sons; 1999.
Kumar A, Anel R, Bunnell E, et al. Preload-independent mechanisms contribute to increased stroke volume following large volume saline infusion in normal volunteers: a prospective interventional study. Critic Care. 2004; 8(3):R128–36.
Lafanechere A, Albaladejo P, Raux M, et al. Cardiac output measurements during infrarenal aortic surgery: echo-esophageal Doppler versus thermodilution catheter. J Cardiothor Vasc Anesth. 2006;20(1):26–30.
Latham RD, Westerhof N, Sipkema P, et al. Regional wave travel and reflections along the human aorta: a study with six simultaneous micromanometric pressures. Circulation. 1985;72:1257–69.
Lehmann ED. Clinical value of aortic pulse-wave velocity measurement. Lancet. 1999;354(9178):528–9.
Levy N. Extending the oesophageal Doppler into the perioperative period. Anaesthesia 2001;56(11):1123–24.
Liu Z, Ting CT, Zhu S, Yin FCP. Aortic compliance in human hypertension. Hypertension. 1989;14:129–36.
Madan AK, UyBarreta VV, Aliabadi-Wahle S, Jesperson R, Hartz RS, Flint LM, Steinberg SM. Esophageal Doppler ultrasound monitor versus pulmonary artery catheter in the hemodynamic management of critically ill surgical patients. J Trauma Injury Infect Critic Care. 1999;46(4):607–11.
Matsubara H, Araki J, Takaki M, Nakagawa ST, Suga H. Logistic characterization of left ventricular isovolumic pressure-time curve. Jpn J Physiol. 1995;45:535–52.
McEniery CM, Wallace YS, Maki-Petaja K, et al. Increased stroke volume and aortic stiffness contribute to isolated systolic hypertension in young adults. Hypertension 2005;46(1):221–6.
Milnor WR. Hemodynamics. 2nd ed. Baltimore, MD: Williams & Wilkens; 1989.
Mitchell GF, Lacourciere Y, Ouellet JP, et al. Determinants of elevated pulse pressure in middle-aged and older subjects with uncomplicated systolic hypertension. The role of proximal aortic diameter and the aortic pressure-flow relationship. Circulation 2003;108:1592–8.
Mowat DH, Haites NE, Rawles JM. Aortic blood velocity measurement in healthy adults using a simple ultrasound technique. Cardiovasc Res. 1983;17(2):75–80.
Nichols W, O’Rourke MF. McDonald’s blood flow in arteries. 5th ed. London, UK: Hodder Arnold; 2005.
Noordergraaf A. Circulatory system dynamics. New York, NY: Academic Press; 1978.
Pauca AL, O’Rourke MF, Kon ND. Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension. 2001;38:932–7.
Poeze M, Ramsay G, Greve JW, Singer M. Prediction of postoperative cardiac surgical morbidity and organ failure within 4 hours of intensive care unit admission using esophageal Doppler ultrasonography. Critic Care Med. 1999;27(7):1288–94.
Polanczyk CA, Rohde LE, Goldman L, Cook EF, Thomas EJ, Marcantonio ER, Mangione CM, Lee TH. Right heart catheterization and cardiac complications in patients undergoing noncardiac surgery. JAMA. 2001;286(3):309–14.
Prokop EK, Palmer RF, Wheat MW. Hydrodynamic forces in dissecting aneurysms. Circ Res. 1970;27:121–7.
Roeck M, Jakob SM, Boehlen T, et al. Change in stroke volume in response to fluid challenge: assessment using esophageal Doppler. Intensive Care Med. 2003;29:1729–35.
Rogers WJ, Hu YL, Coast D, Vido DA, Kramer CM, Pyretiz RE, Reichek N. Age-associated changes in regional aortic pulse wave velocity. J Am Coll Cardiol. 2001;38:1123–9.
Rothenberg DM, Tuman KJ. Pulmonary artery catheter: what does the literature actually tell us? Intl Anesthesiol Clin. 2000;38(4):171–87.
Sandham JD, Hull RD, et al. A randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients. NEJM. 2003;348(1):5–14.
Schertel ER. Assessment of left-ventricular function. Thorac Cardiovasc Surg. 1998;46(Suppl 2):248–54.
Segers P, Qasem A, De Backer T, Carlier S, Verdonck P, Avolio A. Peripheral “Oscillatory” compliance is associated with aortic + augmentation index. Hypertension. 2001;37:1434–9.
Seoudi HM, Perkal MF, Hanrahan A, Angood PB. The esophageal Doppler monitor in mechanically ventilated surgical patients: does it work? J Trauma Injury Infect Critic Care. 2003;55(4):720–6.
Singer M, Bennett ED. Noninvasive optimization of left ventricular filling using esophageal Doppler. Critic Care Med. 1991;19(9):1132–7.
Singer M, Allen MJ, Webb AR, Bennett ED. Effects of alteration in left ventricular filling, contractility, and systemic vascular resistance on the ascending aortic blood velocity waveform of normal subjects. Crit Care Med 1991;19:1138–45.
Soma J, Aakhus S, Dahl K, Widerøe TE, Skjærpe T. Total arterial compliance in ambulatory hypertension during selective β1 adrenergic receptor blockade and angiotensin-converting enzyme inhibition. J Cardiovasc Pharmacol. 1999;33(2):273–9.
Stergiopulos N, Westerhof BE, Westerhof N. Total arterial inertance as the fourth element of the windkessel model. Am J Physiol. 1999;276(Heart Circ Physiol 45):H81–8.
Sugawara M, Senda S, Katayama H, Masugata H, Nishiya T, Matsuo H. Noninvasive estimation of left ventricular Max(dP/dt) from aortic flow acceleration and pulse wave velocity. Echocardiography. 1994;11:377–84.
The National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. NEJM. 2006;354(21):2213–23.
Valtier B, Cholley BP, Belot JP, et al. Noninvasive monitoring of cardiac output in critically ill patients using transesophageal Doppler. Am J Respir Crit Care Med. 1998;158:77–83.
Vignon P. Hemodynamic assessment of critically ill patients using echocardiography Doppler. Curr Opin Critic Care. 2005;11(3):227–34.
Vincent JL, Dhainaut JF, Perret C, Suter P (1998) Is the pulmonary artery catheter misused? A European view. Critic Care Med. 1998;26(7):1283–7.
Wallmeyer K, Wann LS, Sagar KB, Kalbfleisch J, Klopfenstein HS. The influence of preload and heart rate on Doppler echocardiographic indexes of left ventricular performance: comparison with invasive indexes in an experimental preparation. Circulation. 1986;74:181–6.
Warzawski RC, Deye AN, et al. Early use of the pulmonary artery catheter and outcomes in patients with shock and acute respiratory distress syndrome: a randomized controlled trail. JAMA. 2003;290(20):2713–20.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A
Determining Cardiac Output Using EDM Parameters (Boulnois and Pechoux 2000)
Stroke distance, in the distal aorta, SDaorta, is determined from the integral of distal aortic blood flow velocity over flow time:
Note that the average velocity, of distal aortic blood flow \(\bar{V}\), is:
Therefore, SDaorta is equivalent to the product of average velocity and flow time:
Stroke volume in the distal aorta is:
where A is the distal aortic cross-sectional area. Thus:
That portion of cardiac output, which flows through the distal aorta, is then:
In this application, flow time, FT, has units of seconds/beat and heart rate, HR, has units of beats/second. Therefore the product: FT × HR is dimensionless.
Total cardiac output is then:
where 1.4 is a dimensionless constant which is based upon a linear regression analysis from clinical data (Boulnois and Pechoux 2000).
If distal aortic cross-sectional area is unknown, minute distance within the aorta, MDaorta, can be defined as:
Therefore, MDaorta = SDaorta · HR. Thus, MDaorta correlates with total cardiac output.
Appendix B
Determining Stroke Distance, in the Distal Aorta, by Integrating Aortic Blood Flow Velocity Over Time
Using the logistic-based systolic model:
Separating the above so that sd(t) = I 1 − I 2—constant of integration:
The constant of integration is then chosen so that sd(0) = 0:
Thus:
Figure A1 is plot of sd(t) which reveals the familiar sigmoid curve that is characteristic of the logistic function.
Evaluating \({sd}(t)\vert^{\rm FT}_{0}\) yields SDaorta = sd(FT) since sd(0) = 0:
Appendix C
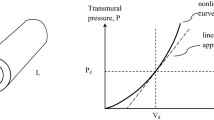
Derivation of the Bramwell–Hill Equation (Bramwell and Hill 1922)
Tension, T, within the wall of a compliant cylinder can be described as:
where σ is stress and h is wall thickness. It is assumed that h is small compared to radius, r. Furthermore, both internal and external radii are approximately equal and are represented as the constant r. ΔP represents the difference between external and internal wall pressures.
Therefore, wall stress is (Noordergraaf 1978):
Strain, ɛ, is defined as:
Young’s modulus, E, is:
The change in radius, due to the change in pressure, can then be represented as:
Compliance is defined as the change in volume divided by the change in pressure:
where r f is the final radius and r i is the initial radius and L e is the length of the compliant cylinder. Recognizing that (r 2f −r 2i ) is the difference of two squares, (C.6) can then be expressed as:
Noting that \(r_{\rm f}+ r_{\rm i}\approx 2 r\) and r f−r i = Δr, then (C.7) can be expressed as:
Substituting (C.5) into (C.8) yields:
Compliance can then be expressed as:
Young’s modulus can then be represented as:
The Moens–Korteweg equation (Milnor 1989) relates pulse wave velocity, in a compliant cylinder, to its geometric and physical properties:
Substituting (C.11) into (C.12) and simplifying yields the Bramwell–Hill equation ([Milnor 1989; Liu et al. 1989):
Rights and permissions
About this article
Cite this article
Atlas, G.M. Development and Application of a Logistic-Based Systolic Model for Hemodynamic Measurements Using the Esophageal Doppler Monitor. Cardiovasc Eng 8, 159–173 (2008). https://doi.org/10.1007/s10558-008-9057-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10558-008-9057-9