Abstract
Purpose
Adults with atherosclerotic cardiovascular disease (ASCVD) are recommended high-intensity statins, with those at very high risk for recurrent events recommended adding ezetimibe and/or a proprotein convertase subtilisin/kexin type 9 inhibitor if their low-density lipoprotein cholesterol (LDL-C) is ≥70 mg/dL. We estimated the number of recurrent ASCVD events potentially averted if all adults in the United States (US) ≥45 years of age with ASCVD achieved an LDL-C <70 mg/dL.
Methods
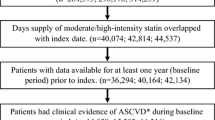
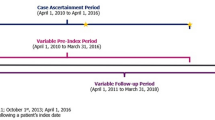
The number of US adults with ASCVD and LDL-C ≥70 mg/dL was estimated from the National Health and Nutrition Examination Survey 2009–2016 (n = 596). The 10-year cumulative incidence of recurrent ASCVD events was estimated from the REasons for Geographic And Racial Differences in Stroke study (n = 5390), weighted to the US population by age, race, and sex. The ASCVD risk reduction by achieving an LDL-C <70 mg/dL was estimated from meta-analyses of lipid-lowering treatment trials.
Results
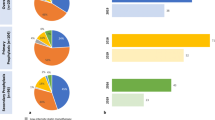
Overall, 14.7 (95% CI, 13.7–15.8) million US adults had ASCVD, of whom 11.6 (95% CI, 10.6–12.5) million had LDL-C ≥70 mg/dL. The 10-year cumulative incidence of ASCVD events was 24.3% (95% CI, 23.2–25.6%). We projected that 2.823 (95% CI, 2.543–3.091) million ASCVD events would occur over 10 years among US adults with ASCVD and LDL-C ≥70 mg/dL. Overall, 0.634 (95% CI, 0.542–0.737) million ASCVD events could potentially be averted if all US adults with ASCVD achieved and maintained LDL-C <70 mg/dL.
Conclusion
A substantial number of recurrent ASCVD events could be averted over 10 years if all US adults with ASCVD achieved, and maintained, an LDL-C <70 mg/dL.


Similar content being viewed by others
References
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. Circulation. 2014;129:S1–45. https://www.ahajournals.org/doi/10.1161/01.cir.0000437738.63853.7a.
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38:2459–72. https://doi.org/10.1093/eurheartj/ehx144.
Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet. 2010;376:1670–81. https://doi.org/10.1016/S0140-6736(10)61350-5.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387–97. http://www.nejm.org/doi/10.1056/NEJMoa1410489.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379:2097–107. http://www.nejm.org/doi/10.1056/NEJMoa1801174.
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713–22. http://www.nejm.org/doi/10.1056/NEJMoa1615664.
Ference BA, Cannon CP, Landmesser U, Lüscher TF, Catapano AL, Ray KK. Reduction of low density lipoprotein-cholesterol and cardiovascular events with proprotein convertase subtilisin-kexin type 9 (PCSK9) inhibitors and statins: an analysis of FOURIER, SPIRE, and the Cholesterol Treatment Trialists Collaboration. Eur Heart J. 2018;39:2540–5. https://academic.oup.com/eurheartj/article-abstract/39/27/2540/4082634.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:E1082–143. https://doi.org/10.1161/CIR.0000000000000625.
Eckel RH, Jakicic JM, Ard JD, De Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;p. 76–99. http://circ.ahajournals.org/lookup/suppl/doi:10.1161/01.cir.0000437740.48606.d1/-/DC1.
Rosenblit PD. Extreme atherosclerotic cardiovascular disease (ASCVD) risk recognition. Curr Diab Rep. 2019;19:1–20. http://link.springer.com/10.1007/s11892-019-1178-6.
Muntner P, Levitan EB, Brown TM, Sharma P, Zhao H, Bittner V, et al. Trends in the prevalence, awareness, treatment and control of high low density lipoprotein-cholesterol among United States adults from 1999–2000 through 2009–2010. Am J Cardiol.; 2013;112:664–70. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3769104/.
Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174 000 participants in 27 randomised trials. Lancet. 2015;385:1397–405. https://linkinghub.elsevier.com/retrieve/pii/S0140673614613684.
Colantonio LD, Monda KL, Rosenson RS, Brown TM, Mues KE, Howard G, et al. Characteristics and cardiovascular disease event rates among African Americans and Whites who meet the Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk (FOURIER) trial inclusion criteria. Cardiovasc Drugs Ther. 2019;33:189–99. https://doi.org/10.1007/s10557-019-06864-2.
Sampson M, Ling C, Sun Q, Harb R, Ashmaig M, Warnick R, et al. A new equation for calculation of low-density lipoprotein cholesterol in patients with normolipidemia and/or hypertriglyceridemia. JAMA Cardiol. 2020;5:E1–9. https://jamanetwork.com/journals/jamacardiology/fullarticle/2761953.
Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The Reasons for Geographic and Racial Differences in Stroke study: objectives and design. Neuroepidemiology. 2005;25:135–43. https://doi.org/10.1159/000086678.
Safford MM, Brown TM, Muntner PM, Durant RW, Glasser S, Halanych JH, et al. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308:1768–74. https://doi.org/10.1001/jama.2012.14306.
Hansen RA, Khodneva Y, Glasser SP, Qian J, Redmond N, Safford MM. Antidepressant medication use and its association with cardiovascular disease and all-cause mortality in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. Ann Pharmacother. 2016;50:253–61. http://www.ncbi.nlm.nih.gov/pubmed/26783360.
Curtin L, Mohadjer L, Dohrmann S, Kruszon-Moran D, Mirel L, Carroll M, et al. National Health and Nutrition Examination Survey: sample design, 2007-2010. National Center for Health Statistics. 2013. https://www.cdc.gov/nchs/data/series/sr_02/sr02_160.pdf. Accessed 30 Dec 2020.
Mirel LB, Mohadjer LK, Dohrmann SM, Clark J, Burt VL, Johnson CL, et al. National Health and Nutrition Examination Survey: estimation procedures, 2007-2010. National Center for Health Statistics. 2013. https://www.cdc.gov/nchs/data/series/sr_02/sr02_159.pdf. Accessed 30 Dec 2020.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
DiCiccio TJ, Efron B. Bootstrap confidence intervals. Stat Sci. 1996;11:189–212.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88. https://doi.org/10.1093/eurheartj/ehz455.
Jellinger PS. American Association of Clinical Endocrinologists/American College of Endocrinology management of dyslipidemia and prevention of cardiovascular disease clinical practice guidelines. Diabetes Spectr. 2018;31:234–45. https://doi.org/10.2337/ds18-0009.
Brown TM, Deng L, Becker DJ, Bittner V, Levitan EB, Rosenson RS, et al. Trends in mortality and recurrent coronary heart disease events after an acute myocardial infarction among Medicare beneficiaries, 2001-2009. Am Heart J Mosby Inc. 2015;170:249–255.e2. https://doi.org/10.1016/j.ahj.2015.04.027.
Pandya A, Gaziano TA, Weinstein MC, Cutler D. More Americans living longer with cardiovascular disease will increase costs while lowering quality of life. Health Aff. 2013;32:1706–14. https://doi.org/10.1377/hlthaff.2013.0449.
American Heart Association. Check. Change. Control. Cholesterol Progam. 2018. https://www.heart.org/en/health-topics/cholesterol/cholesterol-tools-and-resources/check-change-control-cholesterol-program. Accessed 7 Dec 2020.
Sabatine MS, Wiviott SD, Im K, Murphy SA, Giugliano RP. Efficacy and safety of further lowering of low-density lipoprotein cholesterol in patients starting with very low levels: a meta-analysis. JAMA Cardiol. 2018;3:823–8. https://doi.org/10.1001/jamacardio.2018.2258.
Colantonio LD, Rosenson RS, Deng L, Monda KL, Dai Y, Farkouh ME, et al. Adherence to statin therapy among US adults between 2007 and 2014. J Am Heart Assoc. 2019;8:1–20. https://doi.org/10.1161/JAHA.118.010376.
Thompson PD, Panza G, Zaleski A, Taylor B. Statin-associated side effects. J Am Coll Cardiol. 2016;67:2395–410. https://doi.org/10.1016/j.jacc.2016.02.071.
Mefford MT, Tajeu GS, Tanner RM, Colantonio LD, Monda KL, Dent R, et al. Willingness to be reinitiated on a statin (from the REasons for Geographic and Racial Differences in Stroke study). Am J Cardiol. 2018;122:768–74. https://doi.org/10.1016/j.amjcard.2018.05.016.
Cannon CP, Khan I, Klimchak AC, Reynolds MR, Sanchez RJ, Sasiela WJ. Simulation of lipid-lowering therapy intensification in a population with atherosclerotic cardiovascular disease. JAMA Cardiol. 2017;2:959–66. https://doi.org/10.1001/jamacardio.2017.2289.
Bohula EA, Morrow DA, Giugliano RP, Blazing MA, He P, Park JG, et al. Atherothrombotic risk stratification and ezetimibe for secondary prevention. J Am Coll Cardiol. 2017;69:911–21. https://doi.org/10.1016/j.jacc.2016.11.070.
Dixon DL, Trankle C, Buckley L, Parod E, Carbone S, Van Tassell BW, et al. A review of PCSK9 inhibition and its effects beyond LDL receptors. J Clin Lipidol. 2016;10:1073–80. https://doi.org/10.1016/j.jacl.2016.07.004.
Karalis DG, Mallya UG, Ghannam AF, Elassal J, Gupta R, Boklage SH. Prescribing patterns of proprotein convertase subtilisin-kexin type 9 inhibitors in eligible patients with clinical atherosclerotic cardiovascular disease or heterozygous familial hypercholesterolemia. Am J Cardiol. 2018;121:1155–61. https://doi.org/10.1016/j.amjcard.2018.02.002.
Nadruz W, Claggett B, Henglin M, Shah AM, Skali H, Rosamond WD, et al. Widening racial differences in risks for coronary heart disease. Circulation. 2018;137:1195–7. https://doi.org/10.1161/CIRCULATIONAHA.117.030564.
Peters SAE, Colantonio LD, Dai Y, Zhao H, Bittner VA, Farkouh ME, et al. Trends in recurrent coronary heart disease following myocardial infarction among US women and men between 2008 and 2017. Circulation. 2020;143:650–60. https://doi.org/10.1161/CIRCULATIONAHA.120.047065.
Patel KK, Taksler GB, Hu B, Rothberg MB. Prevalence of elevated cardiovascular risks in young adults: a cross-sectional analysis of National Health and Nutrition Examination Surveys. Ann Intern Med. 2017;166:876–82. https://doi.org/10.7326/M16-2052.
Acknowledgements
The design and conduct of the study, interpretation of the results, and preparation of the manuscript were supported through a research grant from Amgen, Inc. (Thousand Oaks, CA). The academic authors conducted all analyses and maintained the rights to publish this article. The REGARDS study is supported by a cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke and the National Institute on Aging, National Institutes of Health, Department of Health and Human Service. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis, or interpretation of the data. Additional support was provided by grants R01 HL080477 and K24 HL111154 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions and further information about the study can be found at http://www.regardsstudy.org.
Availability of Data Materials
The datasets generated and/or analyzed during the current study will be made available from the corresponding author upon reasonable request.
Declarations
Ethics Approval and Consent to Participate
The institutional review board at the University of Alabama at Birmingham approved the study and waived the requirement to obtain informed consent.
Consent for Publication
Not applicable.
Competing Interests
ECM receives research support from Amgen, Inc. VAB receives research support from Amgen, Inc.; serves on the executive steering committee of the ODYSSEY OUTCOMES trial (Sanofi); as National Coordinator for STRENGTH (Astra Zeneca), DalGene (Dalcor), and CLEAR (Esperion); and as local site investigator for ORION IV (Novartis). She served as a consultant to Sanofi in 2018 and is currently consulting for Pfizer. TMB receives research support from Amgen, Inc. and served as the local site investigator for STRENGTH (Astra Zeneca). EAJ receives research support from Amgen, Inc. and NIH; consulting fees from the American College of Cardiology and McKesson; expert witness for DeBlase Brown Everly, LLP; royalties from UpToDate, Inc.; and editor for the American Heart Association. MEF receives research support from Amgen, Inc., Novo Nordisk, and Novartis. EBL receives research support from Amgen, Inc. and consulting fees from Novartis. RSR receives research support from Amgen, Inc., Astra Zeneca, Novartis, and Regeneron; consulting fees from Amgen, Inc., Amryt, C5, CVS Caremark, Novartis, Regeneron, and 89 Bio; honoraria from Amgen, Inc., Kowa, and Regeneron; and royalties from Wolters Kluwer (UpToDate, Inc.) and has stock in MediMergent, LLC. MMS receives research support from Amgen, Inc. MW serves as a consultant for Amgen, Inc., Freeline, and Kyowa Kirin. JE, KKO, and SRR are employees of and have stock in Amgen, Inc. PM receives research support and consulting fees from Amgen, Inc. LDC receives research support from Amgen, Inc. No other disclosures were reported.
Funding
This work was funded by Amgen Inc., Thousand Oaks, CA.
Author information
Authors and Affiliations
Contributions
ECM, VAB, TMB, EAJ, MEF, EBL, RSR, MMS, JE, KKO, SRR, PM, and LDC contributed to the study concept, study design, interpretation of results, and manuscript content. LC and LH conducted the data analysis. The first draft of the manuscript was written by ECM. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 99.4 kb)
Rights and permissions
About this article
Cite this article
McKinley, E.C., Bittner, V.A., Brown, T.M. et al. The Projected Impact of Population-Wide Achievement of LDL Cholesterol <70 mg/dL on the Number of Recurrent Events Among US Adults with ASCVD. Cardiovasc Drugs Ther 37, 107–116 (2023). https://doi.org/10.1007/s10557-021-07268-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-021-07268-x