Abstract
Purpose
This meta-analysis compared the efficacy and safety of oral anticoagulation (OAC) therapy alone versus OAC plus single antiplatelet therapy (SAPT) in patients with an indication for chronic OAC (mostly due to atrial fibrillation) after transcatheter aortic valve implantation (TAVI).
Methods
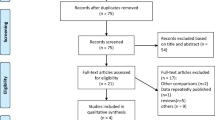
A systematic literature search was performed in the PubMed, Embase, and Cochrane Library databases to identify relevant studies. Data was extracted from the eligible studies and outcomes expressed as relative risks (RRs) with 95% confidence intervals (CIs).
Results
Five studies comprising 1344 patients with an indication for chronic OAC and undergoing TAVI were included. Of the 1344 patients, 480 patients received OAC therapy alone and 864 patients received OAC plus SAPT. There were no significant differences between OAC alone versus OAC plus SAPT in all-cause mortality (RR = 1.05, 95% CI 0.84–1.30, p = 0.69) and ischemic stroke (RR = 0.95, 95% CI 0.95–1.61, p = 0.86). However, OAC alone was associated with significantly lower risks of all bleeding events (RR = 0.62, 95% CI 0.49–0.69, p < 0.0001) and major and/ life-threatening bleeding events (RR = 0.57, 95% CI 0.42–0.76, p = 0.0002) compared to OAC plus SAPT.
Conclusion
In patients with an indication for chronic anticoagulation, post-TAVI antithrombotic therapy with OAC alone compared to OAC plus SAPT may be not significantly different in reducing all-cause mortality and ischemic stroke, but has an important benefit in a significantly lower risk of all bleeding and major and/life-threatening bleeding events.





Similar content being viewed by others
Availability of data and materials
All data generated or analyzed during this study are included in the article.
References
Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364(23):2187–98.
Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376(14):1321–31.
Witberg G, Landes U, Lador A, Yahav D, Kornowski R. Meta-analysis of transcatheter aortic valve implantation versus surgical aortic valve replacement in patients at low surgical risk. EuroIntervention. 2019;15(12):e1047–e1056.
Kolte D, Vlahakes GJ, Palacios IF, et al. Transcatheter versus surgical aortic valve replacement in low-risk patients. J Am Coll Cardiol. 2019;74(12):1532–40.
Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38(36):2739–91.
Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the Management of Patients with Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;70(2):252–89.
Zuo W, Yang M, He Y, Hao C, Chen L, Ma G. Single or dual antiplatelet therapy after transcatheter aortic valve replacement: an updated systemic review and meta-analysis. J Thorac Dis. 2019;11(3):959–68.
Ussia GP, Scarabelli M, Mulè M, et al. Dual antiplatelet therapy versus aspirin alone in patients undergoing transcatheter aortic valve implantation. Am J Cardiol. 2011;108(12):1772–6.
Stabile E, Pucciarelli A, Cota L, et al. SAT-TAVI (single antiplatelet therapy for TAVI) study: a pilot randomized study comparing double to single antiplatelet therapy for transcatheter aortic valve implantation. Int J Cardiol. 2014;174(3):624–7.
Tarantini G, Mojoli M, Urena M, Vahanian A. Atrial fibrillation in patients undergoing transcatheter aortic valve implantation: epidemiology, timing, predictors, and outcome. Eur Heart J. 2017;38:1285–93.
Tarantini G, Mojoli M, Windecker S, et al. Prevalence and impact of atrial fibrillation in patients with severe aortic stenosis undergoing Transcatheter aortic valve replacement: an analysis from the SOURCE XT prospective multicenter registry. JACC Cardiovasc Interv. 2016;9(9):937–46.
Mok M, Urena M, Nombela-Franco L, et al. Clinical and prognostic implications of existing and new-onset atrial fibrillation in patients undergoing transcatheter aortic valve implantation. J Thromb Thrombolys. 2013;35(4):450–5.
Genereux P, Cohen DJ, Mack M, et al. Incidence, predictors, and prognostic impact of late bleeding complications after transcatheter aortic valve replacement. J Am Coll Cardiol. 2014;64(24):2605–15.
Guedency P, Mehran R, Collet JP, Claessen BE, Ten Berg J, Dangas GD. Antithrombotic therapy after transcatheter aortic valve replacement. Circ Cardiovasc Interv. 2019;12(1):e7411.
Vavuranakis M, Kalogeras K, Vrachatis D, et al. Antithrombotic therapy in patients undergoing TAVI with concurrent atrial fibrillation: one center experience. J Thromb Thrombolys. 2015;40(2):193–7.
Abdul-Jawad Altisent O, Durand E, Munoz-Garcia AJ, et al. Warfarin and antiplatelet therapy versus warfarin alone for treating patients with atrial fibrillation undergoing transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2016;9(16):1706–17.
Nijenhuis VJ, Brouwer J, Delewi R, et al. Anticoagulation with or without clopidogrel after transcatheter aortic-valve implantation. N Engl J Med. 2020;382(18):1696–707.
Vrabel M. Preferred reporting items for systematic reviews and meta-analyses. Oncol Nurs Forum. 2015;42(5):552–4.
Kappetein AP, Head SJ, Généreux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur Heart J. 2012;33(19):2403–18.
Figini F, Latib A, Maisano F, et al. Managing patients with an indication for anticoagulant therapy after transcatheter aortic valve implantation. Am J Cardiol. 2013;111(2):237–42.
Geis N, Kiriakou C, Chorianopoulos E, Pleger S, Katus H, Bekeredjian R. Feasibility and safety of vitamin K antagonist monotherapy in atrial fibrillation patients undergoing transcatheter aortic valve implantation. EuroIntervention. 2017;12(17):2058–66.
D’Ascenzo F, Benedetto U, Bianco M, et al. Which is the best antiaggregant or anticoagulant therapy after TAVI? A propensity-matched analysis from the ITER registry. The management of DAPT after TAVI. EuroIntervention. 2017;13(12):e1392–400.
Mojoli M, Gersh BJ, Barioli A, et al. Impact of atrial fibrillation on outcomes of patients treated by transcatheter aortic valve implantation: a systematic review and meta-analysis. Am Heart J. 2017;192:64–75.
Rossi JE, Noll A, Bergmark B, et al. Variability in antithrombotic therapy regimens Peri-TAVR: a single academic center experience. Cardiol Ther. 2015;4(2):197–201.
Vranckx P, Windecker S, Welsh RC, Valgimigli M, Mehran R, Dangas G. Thrombo-embolic prevention after transcatheter aortic valve implantation. Eur Heart J. 2017;38(45):3341–50.
Fairbairn TA, Mather AN, Bijsterveld P, et al. Diffusion-weighted MRI determined cerebral embolic infarction following transcatheter aortic valve implantation: assessment of predictive risk factors and the relationship to subsequent health status. Heart. 2011;98(1):18–23.
Kosmidou I, Liu Y, Alu MC, et al. Antithrombotic therapy and cardiovascular outcomes after transcatheter aortic valve replacement in patients with atrial fibrillation. JACC Cardiovasc Interv. 2019;12(16):1580–9.
Schmidt T, Leon MB, Mehran R, et al. Debris heterogeneity across different valve types captured by a cerebral protection system during transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2018;11(13):1262–73.
Kahlert P, Al-Rashid F, Döttger P, et al. Cerebral embolization during transcatheter aortic valve implantation. Circulation. 2012;126(10):1245–55.
Van Mieghem NM, El Faquir N, Rahhab Z, et al. Incidence and predictors of debris embolizing to the brain during transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2015;8(5):718–24.
Nombela-Franco L, Webb JG, de Jaegere PP, et al. Timing, predictive factors, and prognostic value of cerebrovascular events in a large cohort of patients undergoing transcatheter aortic valve implantation. Circulation. 2012;126(25):3041–53.
Seeger J, Gonska B, Otto M, Rottbauer W, Wöhrle J. Cerebral embolic protection during transfemoral aortic valve replacement significantly reduces death and stroke compared with unprotected procedures. JACC Cardiovasc Interv. 2017;10(22):2297–303.
Nietlispach F, Wijesinghe N, Gurvitch R, et al. An embolic deflection device for aortic valve interventions. JACC Cardiovasc Interv. 2010;3(11):1133–8.
Généreux P, Head SJ, Van Mieghem NM, et al. Clinical outcomes after transcatheter aortic valve replacement using valve academic research consortium definitions. J Am Coll Cardiol. 2012;59(25):2317–26.
Piccolo R, Pilgrim T, Franzone A, et al. Frequency, timing, and impact of access-site and non–access-site bleeding on mortality among patients undergoing transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2017;10(14):1436–46.
Toggweiler S, Gurvitch R, Leipsic J, et al. Percutaneous aortic valve replacement: vascular outcomes with a fully percutaneous procedure. J Am Coll Cardiol. 2012;59(2):113–8.
Stortecky S, Wenaweser P, Diehm N, et al. Percutaneous management of vascular complications in patients undergoing transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2012;5(5):515–24.
Lamberts M, Gislason GH, GYH L, et al. Antiplatelet therapy for stable coronary artery disease in atrial fibrillation patients taking an oral anticoagulant. Circulation. 2014;129(15):1577–85.
Valgimigli M, Hector B, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the task force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018;39(3):213–60.
Acknowledgements
First, we would like to express our gratitude to Professor Fabrizio D’Ascenzo for providing us with valuable data when we performed this research. Additionally, we also thanks EditSprings (https://www.editsprings.com/) for the expert linguistic services provided.
Code availability
We performed statistical analysis in the present study with Review Manager version 5.3 (Cochrane Collaboration; Copenhagen, Denmark).
Author information
Authors and Affiliations
Contributions
ZNJ, HGZ, and HL were responsible for the study conception and design. YZ, SM, and MLC contributed to data extraction, assessment of study quality, analysis and interpretation of data, and draft manuscript. The comprehensive literature search was completed by JN. RFJ and LL revised the manuscript critically.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics Approval
The present study is a systematic review and meta-analysis, therefore ethics approval is not required.
Consent to participate
Not applicable.
Consent for publication
All authors read and approved the final manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Zhu, Y., Meng, S., Chen, M. et al. Comparing anticoagulation therapy alone versus anticoagulation plus single antiplatelet drug therapy after transcatheter aortic valve implantation in patients with an indication for anticoagulation: a systematic review and meta-analysis. Cardiovasc Drugs Ther 35, 995–1002 (2021). https://doi.org/10.1007/s10557-020-07081-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-020-07081-y