Abstract
To investigate the long-term prognostic value of the left atrial (LA) strain indices – peak atrial longitudinal strain (PALS), peak conduit strain (PCS), and peak atrial contractile strain (PACS) in acute coronary syndrome (ACS) patients in relation to all-cause mortality. This retrospective study included ACS patients treated with percutaneous coronary intervention (PCI) and examined with echocardiography. Exclusion criteria were non-sinus rhythm during echocardiography, missing images, and inadequate image quality for 2D speckle tracking analysis of the LA. The endpoint was all-cause death. Multivariable Cox regression which included relevant clinical and echocardiographic measures was utilized to assess the relationship between LA strain parameters and all-cause mortality. A total of 371 were included. Mean age was 64 years and 76% were male. Median time to echocardiography was 2 days following PCI. During a median follow-up of 5.7 years, 83 (22.4%) patients died. Following multivariable analysis, PALS (HR 1.04, 1.01–1.06, p = 0.002, per 1% decrease) and PCS (HR 1.05, 1.01–1.09, p = 0.006, per 1% decrease) remained significantly associated with all-cause mortality. PALS and PCS showed a linear relationship with the outcome whereas PACS was associated with the outcome in a non-linear fashion such that the risk of death increased when PACS < 18.22%. All LA strain parameters remained associated with worse survival rate when restricting analysis to patients with left atrial volume index < 34 ml/m2. Reduced LA function as assessed by PALS, PCS, and PACS were associated with an increased risk of long-term mortality in patients with ACS.
Graphical abstract

Similar content being viewed by others
Introduction
Patients who have suffered from acute coronary syndrome (ACS) are at an increased risk of all-cause mortality, especially over a longer term [1, 2]. Timely identification of patients with an elevated risk of all-cause mortality can provide healthcare professionals with the opportunity to offer early and intensified treatment, potentially improving outcomes, and have socioeconomic benefit [3].
Ongoing efforts to improve the treatment of ACS have yielded positive results over recent decades [4]. This is in large due to improvement in both early invasive management as well as in secondary preventive strategies [5]. Still, in an aging global population with accumulating cardiovascular risk factors, the strain on our healthcare system is expected to rise [6, 7]. It is known that impaired left atrial (LA) function following ACS is associated with major adverse cardiovascular events (MACE) [8]. Risk stratifying ACS patients based upon LA function will assist in identifying patients at high risk of mortality [9]. The non-invasive method of two-dimensional speckle tracking echocardiography (2D STE) provides a detailed assessment of LA function [10].
Previous studies have extensively demonstrated that reduced LA reservoir function assessed by peak atrial longitudinal strain (PALS) is linked to clinical outcomes including all-cause mortality in patients with ST-segment elevation myocardial infarction (STEMI) [11,12,13] and with acute myocardial infarction (MI) [14]. However, the value of a more comprehensive evaluation of LA function by other strain indices including peak atrial contractile strain (PACS) and peak conduit strain (PCS) in relation to all-cause mortality following ACS remains unknown.
We hypothesized that PALS, PCS, and PACS could be used as prognostic markers for all-cause mortality in patients with ACS. The graphical abstract summarizes aims, methods and main findings of the present study.
Methods
Study population
During the time period from January 2003 to November 2008, 579 non-consecutive ACS patients were admitted to the Dept. of Cardiology at Gentofte Hospital to have a percutaneous coronary intervention (PCI) performed. These patients were originally part of a larger observational cohort study and described in detail elsewhere [15]. The echocardiographic examinations were performed at Gentofte Hospital a median of 2 days (1–3 days) following the PCI procedure. Screening process for the current study began with 579 ACS patients. Patients were excluded from this study if they had a non-sinus rhythm during echocardiography, missing images, or inadequate image quality for 2D STE analysis. Non-sinus rhythm, which included active atrial fibrillation, was considered an exclusion criterion as PACS would be unobtainable in these patients. Additionally, PALS and PCS would be incomparable between patients with sinus rhythm and those with active atrial fibrillation [16, 17]. A total of 371 non-consecutive ACS patients were included in the final study sample. A flow diagram of the process is illustrated in Fig. 1.
Grouping
Diabetes mellitus was defined as use of anti-diabetic medicine (oral or injection). Hypertension was defined as use of antihypertensive medication. Hypercholesterolemia was defined as use of cholesterol-lowering medication. Diagnosis of heart failure (HF) was obtained through review of electronic health records at admission.
Endpoints
Date of PCI designated the beginning of follow-up. Follow-up data on all-cause mortality was retrieved from the Danish National Causes of Death Registry. Endpoint extraction was made in May 2013. Follow-up was complete (100%).
Echocardiographic examination
Patients underwent transthoracic echocardiography by experienced clinicians and sonographers using GE Vivid ultrasound machines (GE Healthcare, Little Chalfont, UK). The examinations were transferred to and stored on a remote GE Healthcare image archive. All echocardiographic examinations were subsequently analyzed offline including 2D STE using commercially available EchoPac version 202.71 (GE Healthcare, Horten, Norway). The investigator tasked with analysis of the echocardiographic images was blinded to clinical baseline data and endpoints.
Conventional 2D echocardiography
In the parasternal long axis view at the level of the mitral valve leaflet tips, the left ventricle (LV) dimensions were measured at end-diastole [18]. LV mass index (LVMI) was calculated by dividing the anatomical mass with body surface area (BSA) [18]. LV ejection fraction (LVEF) was measured using the Simpson’s biplane method [18]. LA volume (LAV) was obtained at end-systole in the apical 4- and 2-chamber view by the Simpson’s biplane method [18]. LAV index (LAVI) was acquired by indexing LAV to BSA. Mitral valve inflow at the tip of the mitral valve leaflets was recorded using pulsed-wave Doppler imaging in the apical 4-chamber view to measure the peak velocity blood flow in early diastole (E-wave), peak velocity blood flow in late diastole (A-wave), deceleration time of the early filling (DT), and the E/A ratio. By applying pulsed-wave tissue Doppler imaging with the sample areas placed at the septal and lateral walls of the mitral annulus, early mitral annular diastolic velocity (e’) was measured and the E/e’ ratio was determined [19, 20]. LV diastolic dysfunction was classified based on the E/e’ ratio with values > 14, 9–14 and < 9 considered abnormal, indeterminate, and normal respectively [19]. Right ventricular dysfunction was assessed according to tricuspid annular plane systolic excursion, where < 1.7 cm indicated abnormality [18].
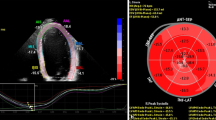
Speckle tracking echocardiography
2D STE analysis was performed of the LA in the 4- and 2-chamber views with a manual point and click function that defined a region of interest (ROI) with the option of being adjusted manually by the investigator if the automatic ROI was considered inaccurate. Both the 4- and 2-chamber LA views were divided into 6 segments for a total analysis of 12 segments. If more than two segments were deemed untraceable after manual adjustment, the investigator excluded it from analysis. The following LA strain measures were derived: PALS, PCS, and PACS. The mean frame rate was 71 ± 25. The methodology is illustrated in Fig. 2.
Statistical analysis
Statistics were carried out using (STATA/SE 17.0). The Wilcoxon rank-sum test was used for comparing continuous non-Gaussian distributed variables, which are presented as interquartile ranges. Pearson’s Chi2 test was used for comparing categorical variables, which are expressed as frequencies (percentages). Student’s t-test was used for comparing continuous Gaussian distributed variables, which are displayed as mean values ± standard deviation. All strain values are presented as absolute values. The prognostic value of PALS, PCS, and PACS were assessed by uni- and multivariable Cox proportional hazards regression models. The multivariable model consisted of either PALS, PCS, or PACS and were adjusted for common confounders and clinically significant factors, i.e., age, sex, LVEF, hypertension, diabetes mellitus, heart failure, multivessel disease, global longitudinal strain (GLS), and LAVI. A sensitivity analysis was performed in which the multivariable analyses were restricted to patients with LAVI < 34 mL/m2. Reported lower limits of normality in a healthy cohort for PALS, PCS, and PACS were used to calculate sensitivity, specificity, positive predictive value, and negative predictive value for LA strain indices [21]. Poisson regression was used for estimating incidence rates and restricted cubic spline curves were constructed to illustrate the relationship between LA strain indices and the incidence rate of all-cause mortality. The number of optimal knots were determined by the lowest Akaike information criterion. Kaplan–Meier curves were constructed to estimate survival probability by groups of low or high PALS, PCS, and PACS, defined by median values. A p-value < 0.05 was considered statistically significant in two-tailed tests.
Results
The final study population consisted of 371 ACS patients following exclusions. Time from onset of ACS to post-PCI echocardiography was median 2 (IQR 1–3) days. The mean age was 64 ± 12 years, and the population predominantly consisted of males (76%). During a median follow-up time of 5.7 (IQR 4.7–6.9) years, 83 (22.4%) patients died. Median time to death in non-survivors was 252 (IQR 44–668) days. Table 1 displays baseline characteristics stratified according to outcome.
Those who died were older (73.2 vs 60.8 years, p < 0.001), had higher heart rate (79.3 ± 17.2 vs 72.4 ± 13.6, p < 0.001), suffered less frequently from hypertension (45.8 vs 66.7%, p < 0.001), fewer were active smokers (55.6 vs 71.2%, p = 0.039), and had a lower body mass index (25.1 ± 4.6 vs 26.7 ± 4.1, p = 0.003). Looking at the echocardiographic measures shown in Table 2, non-survivors had significantly lower LVEF (35.5 vs 42.6% p < 0.001), PALS (30.5 vs 42.9%, p < 0.001), PACS (16.5 vs 20.6%, p < 0.001), PCS (14.9 vs 22.6%, p < 0.001), and GLS (10.7 vs 13.4%, p < 0.001). Table 3 lists all Cox regression models performed.
PALS, PCS, and PACS (PALS: HR 1.06, 1.04–1.08, p < 0.001, per 1% decrease; PCS: HR 1.12, 1.08–1.15, p < 0.001, per 1% decrease; PACS: HR 1.05, 1.02–1.08, p < 0.001, per 1% decrease) were all significantly associated with all-cause mortality in univariable regressions. In multivariable adjustment, only PCS and PALS (PCS: HR 1.05, 1.01–1.09, p = 0.006, per 1% decrease; PALS: HR 1.04, 1.01–1.06, p = 0.002, per 1% decrease) remained significantly associated with all-cause mortality. The continuous relationships between LA strain measures and all-cause mortality are illustrated in Fig. 3a–c.
Risk of dying by continuous changes in left atrial strain indices. Restricted cubic spline curves displaying the unadjusted incidence rate of all-cause death per 100 patient-years as a function of the three LA strain measures, thus illustrating the risk of dying with decreasing values for A PALS. B PCS. C PACS
PALS and PCS showed a linear relationship with all-cause mortality. PACS showed a non-linear relationship such that the incidence rate of death did not increase before PACS decreased below approximately 18.22% corresponding to the median value. The survival probabilities according to medians of PALS, PCS, and PACS are illustrated in Kaplan Meier curves in Fig. 4a–c. All three LA strain indices were significantly associated with all-cause death when the analysis was restricted to individuals with normal LAVI in the multivariable model, (PALS: HR 1.04, 1.02–1.07, p = 0.001, per 1% decrease; PCS: HR 1.05, 1.01–1.09, p = 0.023, per 1% decrease; PACS: HR 1.04, 1.01–1.08, p = 0.019, per 1% decrease). Finally, when restricting the analysis to patients with LAVI < 34 mL/m2, with LA strain indices below its median PALS and PACS remained significantly associated with all-cause death (PALS < 37.89%: HR 2.12, 1.18–3.79, p = 0.011, per 1% decrease; PCS < 18.75%: HR 1.40, 0.77–2.53, p = 0.265, per 1% decrease; PACS < 18.22%: HR 1.89, 1.08–3.31, p = 0.026).
Kaplan–Meier estimators stratified according to abnormal LA strain values. Kaplan–Meier curves displaying probability of staying alive throughout the follow-up period. The x-axis displays the time from exposure (ACS). The y-axis represents the cumulative probability of survival. The study population is stratified into two groups based on whether they are above or below the median of the LA strain measurements (A PALS. B PCS. C PACS). The star symbol denotes the HR
The sensitivity, specificity, positive predictive value, and negative predictive value according to reported lower limits of normality for PALS (< 23%), PCS (< 8.8%), and PACS (< 6.4%) are listed in Table 4.
Discussion
In the present study, we examined the prognostic value of the LA strain indices PALS, PCS, and PACS in regards to long-term survival rate in ACS patients who had echocardiography performed median 2 days after PCI. We made several significant findings: (1) Continuously decreasing PALS and PCS were associated with increased risk of death following multivariable adjustments. (2) PACS was associated with the outcome in a non-linear fashion in patients with normal sized LA such that the risk of death only increased when PACS < 18.22%. (3) All parameters remained significantly associated with all-cause mortality when restricting analysis to patients with normal LAVI.
Previous studies have evaluated the prognostic value of PALS in relation to all-cause death in ACS cohorts. This study was the first to investigate the prognostic value of the additional strain measurements PACS and PCS in an ACS population. A study consisting of 320 STEMI patients treated with PCI achieved results similar to ours. It found PALS as an independent predictor of a composite endpoint consisting of all-cause death, reinfarction and hospitalization due to HF, where 48 (15%) patients reached the combined endpoint [12]. This contrasts with Ersbøll et al. [14], who conducted a study in an MI cohort of 843 patients with a composite endpoint including all-cause death and HF hospitalization in which 47 (5.6%) and 29 (3.4%) patients reached these outcomes, respectively. Echocardiography was performed within 48 h of admission to tertiary hospital where 79.6% of admitted patients underwent PCI. The authors found PALS to be a univariable predictor of outcome, but it was insignificant when adjusting for GLS, age, and LAV, thus concluding that PALS did not provide additional prognostic information over conventional measures. The discrepancy in findings between Ersbøll et al. and the present study may be explained by the difference in endpoints (all-cause mortality vs all-cause mortality and HF hospitalizations) or differences in baseline clinical characteristics. The present cohort, compared to Ersbøll et al. was older, had lower LVEF, and had a higher frequency of hypertension and STEMI indicating that Ersbøll et al. investigated a healthier cohort compared to ours. Such differences could explain the discrepancy in the results. Furthermore, a recent study of patients with HF with the same composite outcome as Ersbøll et al. reported results similar to ours. They found PALS to be a strong prognostic marker in 405 stable HF patients with LVEF < 40%, independent of both GLS and LAV [22]. The three different studies all evaluated the association between PALS and outcome. In summary, they found PALS to be an univariable predictor of outcome and in the majority of studies, it was still significant when accounting for GLS and LAV. Unfortunately, the number of studies investigating the prognostic ability of PCS and PACS is limited and no study has previously investigated the prognostic value of PCS and PACS regarding mortality outcomes among patients with ischemic heart disease. However, a study by Li et al. [9] of 229 ACS patients examined by echocardiography median of 1 day before PCI, demonstrated PALS to have the strongest correlation with global registry of acute coronary events (GRACE) score out of all investigated echocardiographic variables (which included a vast number of structural and functional echocardiographic measurements), closely followed by PCS and PACS. Finally, Svartstein et al. [23] examined 392 STEMI patients following PCI and observed decreasing PALS, PCS, and PACS to be associated with incident atrial fibrillation. However, only PALS remained significant after multivariable analysis. Although these studies are not directly comparable to the present study due to the different investigated endpoints, their observation of similar patterns aligns with our own findings.
In this study, we found a significant association between continuously decreasing PALS and PCS, and an increased risk of death. In contrast, we found that PACS was not significantly associated with an increased risk of death until levels were below 18.22%. This discrepancy may be attributed to the distinct pathophysiological development paths of PALS, PCS, and PACS. PALS and PCS tend to develop in a unidirectional manner, while PACS can exhibit a bidirectional pathophysiological progression [24]. In general, the interdependent LA measurements PALS, PCS, and PACS represent reservoir phase, conduit phase, and contractile phase of the LA respectively [25]. Reservoir phase for the pulmonary venous return is primarily influenced by longitudinal displacement of the LV during contraction and LA myocardial compliance. Conduit phase reflects LV relaxation translated as the passive flow of blood from LA to LV. Contractile phase relies on LV filling pressures and synchronous electromechanical activity. Increased LV filling pressure is common after myocardial infarction and leads to reduced passive filling of the LV from the LA. This is reflected by a reduction in PCS. The LA will compensate by increasing its contractile pressure thereby maintaining PACS. The increase in LA contractile pressure causes reflux to the pulmonary veins leading to increased LA preload which can result in LA remodeling and subsequent decrease in PACS [26]. Persistently increased LV filling pressure can cause LA remodeling and subsequent impaired LA contractile function, which will be observed as a decrease in PACS.
LA strain is potentially a better indicator of LA function and prognosis following ACS than LAVI (the only recommended parameter to evaluate). The study findings indicate that LA strain parameters may provide valuable additional prognostic information in identifying individuals at a higher risk of early death following ACS, even when restricted to normal LAVI. Patients with PALS and PCS below the study median had a more than threefold higher risk of dying than patients above the median. Furthermore, in patients without LA remodeling assessed by LAVI, all LA strain parameters provided long-term prognostic value. Studies have found LA strain to yield predictive value for development of complications associated with increased mortality such as MACE, atrial fibrillation and HF in ACS cohorts [11, 23, 27]. The previously mentioned study by Li et al. [9]. found PALS to be superior to LAVI by comparing their correlation with GRACE risk scores in predicting short term MACE [18, 28, 29]. Furthermore, accurate determination of LAVI has shown to be difficult in under-/overweight patients, and deterioration of LA function can occur before an increase in LAVI [30,31,32]. Inclusion of LA strain analysis in the echocardiographic examination post-PCI is time efficient and simple and may be helpful in detection of high-risk patients. This has the potential to assist in identifying individuals who require intensified follow-up, monitoring, and potential risk intervention, as well as those at a lower risk who may need less frequent monitoring. However, it is crucial to note that these findings should be considered hypothesis-generating, and definitive conclusions would necessitate larger prospective studies or randomized controlled trials.
Limitations
This study has important limitations that must be acknowledged. Firstly, the analysis of LA speckle tracking was performed using non-dedicated software that was originally developed for the LV. This, along with the reliance on vendor-dependent software, may limit the generalizability of our results to other study samples that were analyzed using different echocardiographic software and hardware [33]. However, Mirea et al. [34] compared the use of LV and dedicated LA tracking tools for measuring LA strain, and found no statistical difference in strain value. Additionally, as LA dedicated automatic software was unavailable at the time of analysis, we were unable to perform intra- and inter-observer analysis between LA strain measured by the method used in the present study and LA dedicated automatic software, Secondly, in this study, we adhered to the currently recommended method of measuring LAVI using 2D images [35]. However, the possibility of underestimating true LA volumes by using 2D STE over 3D cannot be dismissed. Thirdly, due to the retrospective nature of the study, several potentially residual confounders related to additional pharmacological treatment, relevant chronic conditions such as paroxysmal/persistent atrial fibrillation, mitral regurgitation, history of important events—e.g., stroke—and certain biochemical markers including estimated glomerular filtration rate, creatine phosphokinase, brain natriuretic peptide, troponin, and reperfusion status were unavailable. Moreover, the potential impact of undiagnosed pre-existing conditions in patients prior to their initial hospitalization for ACS cannot be ruled out, which may have influenced our results. Lastly, since the study sample primarily comprised individuals of Scandinavian descent, caution should be exercised when extrapolating the findings to other ethnicities.
Conclusion
In patients with ACS, reduced LA function by lower PALS, PCS, and PACS were in univariable analysis associated with an increased risk of long-term mortality. Impaired PALS and PCS remained associated with mortality following multivariable adjustments. Lastly, PALS, PCS, and PACS provided prognostic value in patients with normal-sized LA.
Data availability
The data underlying this article cannot be shared publicly due to Danish and European data laws. The data will be shared on reasonable request to the corresponding author.
References
Ellis CJ et al (2019) All-cause mortality following an acute coronary syndrome: 12-year follow-up of the comprehensive 2002 New Zealand acute coronary syndrome audit. Heart Lung Circ 28(2):245–256. https://doi.org/10.1016/j.hlc.2017.10.015
Konttila KK et al (2021) Poor long-term outcome in acute coronary syndrome in a real-life setting: ten-year outcome of the TACOS study. Cardiol J 28(2):302–311. https://doi.org/10.5603/CJ.a2019.0037
Tarride J-E et al (2009) A review of the cost of cardiovascular disease. Can J Cardiol 25(6):e195-202. https://doi.org/10.1016/s0828-282x(09)70098-4
Szummer K et al (2017) Improved outcomes in patients with ST-elevation myocardial infarction during the last 20 years are related to implementation of evidence-based treatments: experiences from the SWEDEHEART registry 1995–2014. Eur Heart J 38(41):3056–3065. https://doi.org/10.1093/eurheartj/ehx515
Vora AN et al (2016) Differences in short- and long-term outcomes among older patients with ST-elevation versus non-ST-elevation myocardial infarction with angiographically proven coronary artery disease. Circ Cardiovasc Qual Outcomes 9(5):513–522. https://doi.org/10.1161/CIRCOUTCOMES.115.002312
Puymirat E et al (2017) Acute myocardial infarction: changes in patient characteristics, management, and 6-month outcomes over a period of 20 years in the FAST-MI program (French registry of acute ST-elevation or non-ST-elevation myocardial infarction) 1995 to 2015. Circulation 136(20):1908–1919. https://doi.org/10.1161/CIRCULATIONAHA.117.030798
Ogurtsova K et al (2017) IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract 128:40–50. https://doi.org/10.1016/j.diabres.2017.03.024
Lønborg JT et al (2013) Left atrial volume and function in patients following ST elevation myocardial infarction and the association with clinical outcome: a cardiovascular magnetic resonance study. Eur Heart J Cardiovasc Imaging 14(2):118–127. https://doi.org/10.1093/ehjci/jes118
Li Y-T et al (2022) Left atrial strain predicts risk and prognosis in patients with acute coronary syndrome: a retrospective study with external validation. Heliyon 8(11):e11276. https://doi.org/10.1016/j.heliyon.2022.e11276
Saraiva RM et al (2010) Left atrial strain measured by two-dimensional speckle tracking represents a new tool to evaluate left atrial function. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr 23(2):172–180. https://doi.org/10.1016/j.echo.2009.11.003
Chu A-A, Wu T-T, Zhang L, Zhang Z (2021) The prognostic value of left atrial and left ventricular strain in patients after ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. Cardiol J 28(5), Art. no. 5. https://doi.org/10.5603/CJ.a2020.0010
Antoni ML et al (2011) Left atrial strain is related to adverse events in patients after acute myocardial infarction treated with primary percutaneous coronary intervention. Heart Br Card Soc 97(16):1332–1337. https://doi.org/10.1136/hrt.2011.227678
Iwahashi N et al. (2022) Prognostic significance of the combination of left atrial reservoir strain and global longitudinal strain immediately after onset of ST-elevation acute myocardial infarction. Circ J advpub:CJ-21-0907. https://doi.org/10.1253/circj.CJ-21-0907
Ersbøll M et al (2013) The prognostic value of left atrial peak reservoir strain in acute myocardial infarction is dependent on left ventricular longitudinal function and left atrial size. Circ Cardiovasc Imaging 6(1):26–33. https://doi.org/10.1161/CIRCIMAGING.112.978296
Iversen AZ et al (2011) Impact of abciximab in diabetic patients with acute coronary syndrome who undergo percutaneous coronary intervention: results from a high-volume, single-center registry. J Invasive Cardiol 23(1):21–26
Cameli M, Mandoli GE, Loiacono F, Sparla S, Iardino E, Mondillo S (2016) Left atrial strain: a useful index in atrial fibrillation. Int J Cardiol 220:208–213. https://doi.org/10.1016/j.ijcard.2016.06.197
DellEra G, Rondano E, Franchi E, Marino PN et al (2010) Atrial asynchrony and function before and after electrical cardioversion for persistent atrial fibrillation. Eur J Echocardiogr 11(7):577–583. https://doi.org/10.1093/ejechocard/jeq010
Lang RM et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr 28(1):1-39.e14. https://doi.org/10.1016/j.echo.2014.10.003
Nagueh SF et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr 29(4):277–314. https://doi.org/10.1016/j.echo.2016.01.011
Park J-H, Marwick TH (2011) Use and limitations of E/e’ to assess left ventricular filling pressure by echocardiography. J Cardiovasc Ultrasound 19(4):169–173. https://doi.org/10.4250/jcu.2011.19.4.169
Nielsen AB et al (2022) Normal values and reference ranges for left atrial strain by speckle-tracking echocardiography: the Copenhagen City Heart Study. Eur Heart J—Cardiovasc Imaging 23(1):42–51. https://doi.org/10.1093/ehjci/jeab201
Carluccio E et al (2018) Left atrial reservoir function and outcome in heart failure with reduced ejection fraction. Circ Cardiovasc Imaging 11(11):e007696. https://doi.org/10.1161/CIRCIMAGING.118.007696
Svartstein A-SW et al (2022) Predictive value of left atrial strain in relation to atrial fibrillation following acute myocardial infarction. Int J Cardiol 364:52–59. https://doi.org/10.1016/j.ijcard.2022.05.026
Blume GG et al (2011) Left atrial function: physiology, assessment, and clinical implications. Eur J Echocardiogr 12(6):421–430. https://doi.org/10.1093/ejechocard/jeq175
Barbier P, Solomon SB, Schiller NB, Glantz SA (1999) Left atrial relaxation and left ventricular systolic function determine left atrial reservoir function. Circulation 100(4):427–436. https://doi.org/10.1161/01.CIR.100.4.427
Baltabaeva A et al (2009) How to detect early left atrial remodelling and dysfunction in mild-to-moderate hypertension. J Hypertens 27(10):2086–2093. https://doi.org/10.1097/HJH.0b013e32832f4f3d
Gan GCH, Ferkh A, Boyd A, Thomas L (2018) Left atrial function: evaluation by strain analysis. Cardiovasc Diagn Ther 8(1):29–46. https://doi.org/10.21037/cdt.2017.06.08
Collet J-P et al (2021) 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 42(14):1289–1367. https://doi.org/10.1093/eurheartj/ehaa575
Ibanez B et al (2018) 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 39(2):119–177. https://doi.org/10.1093/eurheartj/ehx393
Modin D, Pedersen S, Fritz-hansen T, Gislason G, Biering-sørensen T (2020) Left atrial function determined by echocardiography predicts incident heart failure in patients with STEMI treated by primary percutaneous coronary intervention. J Card Fail 26(1):35–42. https://doi.org/10.1016/j.cardfail.2019.08.014
Kojima T et al (2012) Left atrial global and regional function in patients with paroxysmal atrial fibrillation has already been impaired before enlargement of left atrium: velocity vector imaging echocardiography study. Eur Heart J—Cardiovasc Imaging 13(3):227–234. https://doi.org/10.1093/ejechocard/jer281
Singh M, Sethi A, Mishra AK, Subrayappa NK, Stapleton DD, Pellikka PA (2020) Echocardiographic imaging challenges in obesity: guideline recommendations and limitations of adjusting to body size. J Am Heart Assoc 9(2):e014609. https://doi.org/10.1161/JAHA.119.014609
Wang Y et al (2019) Left atrial strain reproducibility using vendor-dependent and vendor-independent software. Cardiovasc Ultrasound 17(1):9. https://doi.org/10.1186/s12947-019-0158-y
Mirea O, Duchenne J, Voigt J-U (2022) Comparison between nondedicated and novel dedicated tracking tool for right ventricular and left atrial strain. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr 35(4):419–425. https://doi.org/10.1016/j.echo.2021.11.011
Badano LP et al (2018) Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 19(6):591–600. https://doi.org/10.1093/ehjci/jey042
Funding
Open access funding provided by Copenhagen University.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by Philip Rüsell Pedersson and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
T.B.S. reports: Steering Committee member of the Amgen financed ‘GALACTIC-HF’ trial. Chief investigator and steering committee chair of the Sanofi Pasteur financed ‘NUDGE-FLU’ trial. Chief investigator and steering committee chair of the Sanofi Pasteur financed ‘DANFLU-1’ trial. Chief investigator and steering committee chair of the Sanofi Pasteur financed ‘DANFLU-2’ trial. Steering Committee member of ‘LUX-Dx TRENDS Evaluates Diagnostics Sensors in Heart Failure Patients Receiving Boston Scientific’s Investigational ICM System’ trial. Advisory Board: Sanofi Pasteur, Amgen, and GSK. Speaker Honorarium: Novartis, Sanofi Pasteur, and GSK. Research grants: GE Healthcare and Sanofi Pasteur. K.G.S reports: Advisory Board: Sanofi Pasteur. P.G.J reports: Speaker Honorarium from Astra Zeneca. The remaining authors have nothing to disclose.
Ethical approval
Written informed consent was obtained from all patients. The retrospective study was performed in accordance with the 2nd declaration of Helsinki and approved by the regional ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pedersson, P.R., Skaarup, K.G., Lassen, M.C.H. et al. Left atrial strain is associated with long-term mortality in acute coronary syndrome patients. Int J Cardiovasc Imaging 40, 841–851 (2024). https://doi.org/10.1007/s10554-024-03053-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-024-03053-7