Abstract
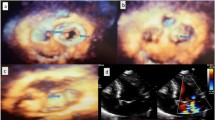
Mitral valve area (MVA) measurement by three-dimensional transesophageal echocardiography (3D-TEE) has a crucial role in the evaluation of mitral stenosis (MS) severity. Three-dimensional direct (3D-direct) planimetry has been proposed as a new technique to measure mitral valve area. This study aimed to compare the 3D-direct mitral valve planimetry to conventional three-dimensional multiplanar reconstruction (3D-MPR) in severe MS using 3D-TEE. In this cross-sectional, prospective study; 149 patients with severe MS who were referred for transesophageal echocardiography in Shahid Madani Hospital (Tabriz Iran), just before percutaneous transmitral commissurotomy (PTMC), recruited consecutively. All patients underwent 2D transthoracic echocardiography (2D-TTE) and 3D-TEE in a single session before PTMC. During 2D-TTE planimetry, pressure half time (PHT), and proximal isovelocity surface area (PISA) were applied to measure the MVA. Transmitral mean pressure gradient (MPG) was measured. During 3D-TEE, MVA planimetry was carried out with both 3D-direct and 3D-MPR methods. 3D-direct was applied from both atrial and ventricular views. The consistency of MVA measurements with 3D-direct, 3D-MPR, and 2D-TTE methods was statistically investigated. Our sample consisted of 109 (73.2%) women and 40 (26.8%) men. The mean age was 51.75 ± 9.81 years. The agreement between 3D-direct and 3D-MPR planimetry was significant and moderate (0.99 ± 0.29 cm2 vs. 1.12 ± 0.26 cm2, intraclass correlation = 0.716, p value = 0.001).The accuracy of the 3D-direct method reduced significantly compared to the MPR method at MVA > 1.5 cm2. The maximum difference between two methods was observed in cases with MVAs larger than 1.5 cm2. MVA measured with the 3D-MPR method was significantly correlated with a 2D-TTE method, with a moderate agreement (intraclass correlation = 0.644, p value = 0.001). Also, 2D-TTE and 3D-direct TEE techniques yielded significantly consistent measurements of the MVA (1.06 ± 0.026 cm2 vs. 0.99 ± 0.29 cm2, intraclass correlation = 0.787, p value = 0.001); however, with a slight overestimation of the MVA by the former with a net difference of 0.06 ± 0.013 cm2. Mitral valve pressure gradient (MPG) had no significant correlation with planimetry results. A significant inverse correlation was seen between the MVA and pulmonary arterial systolic pressure. 3D-direct planimetry has an acceptable agreement with 3D-MPR planimetry at MVA less than 1.5 cm2, but their correlation decreases significantly at MVA above 1.5 cm2. 3D-direct planimetry underestimates MVA compared to 3D-MPR, especially at MVA above 1.5 cm2. It seems that the saddle shape of mitral valve, interferes with 3D-direct measurement of commissures at moderate MS. The 2D-TTE planimetry has generally acceptable accuracy, but its correlation to the 3D-TEE methods is significantly reduced in cases with moderate to severe MS (i.e. MVA > 1.0 cm2).




Similar content being viewed by others
References
Ranjan R, Pressman GS (2018) A etiology and epidemiology of mitral stenosis. E-J Cardiol Pract 16:14
Reményi B, Wilson N, Steer A, Ferreira B, Kado J, Kumar K et al (2012) World heart federation criteria for echocardiographic diagnosis of rheumatic heart disease–an evidence-based guideline. Nat Rev Cardiol 9(5):297–309
Manjunath CN, Srinivas P, Ravindranath KS, Dhanalakshmi C (2014) Incidence and patterns of valvular heart disease in a tertiary care high-volume cardiac center: a single center experience. Indian Heart J 66(3):320–326
Nishimura RA, Carabello BA, Faxon DP, Freed MD, Lytle BW, O’Gara PT et al (2008) ACC/AHA 2008 guideline update on valvular heart disease: focused update on infective endocarditis: a report of the American College of Cardiology/American Heart Association task force on practice guidelines: endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 118(8):887–896
Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP et al (2009) Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr 22(1):1–23
Baumgartner H, Hung J, Bermejo J (2009) Echocardiographic assessment of valve stenosis: European Association of Echocardiography (EAE)/American Society of Echocardiography (ASE) recommendations for clinical practice. Eur J Echocardiogr 10:1–25
Dreyfus J, Brochet E, Lepage L, Attias D, Cueff C, Detaint D et al (2011) Real-time 3D transoesophageal measurement of the mitral valve area in patients with mitral stenosis. Eur J Echocardiogr 12(10):750–755
Messika-Zeitoun D, Brochet E, Holmin C, Rosenbaum D, Cormier B, Serfaty J-M et al (2007) Three-dimensional evaluation of the mitral valve area and commissural opening before and after percutaneous mitral commissurotomy in patients with mitral stenosis. Eur Heart J 28(1):72–79
Schlosshan D, Aggarwal G, Mathur G, Allan R, Cranney G (2011) Real-time 3D transesophageal echocardiography for the evaluation of rheumatic mitral stenosis. JACC Cardiovasc Imaging 4(6):580–588
Anwar AM, Attia WM, Nosir YF, Soliman OI, Mosad MA, Othman M et al (2010) Validation of a new score for the assessment of mitral stenosis using real-time three-dimensional echocardiography. J Am Soc Echocardiogr 23(1):13–22
Poster Session - Poster session 1 (2019). Eur Heart J Cardiovasc Imaging 20(1):i138–i254. https://doi.org/10.1093/ehjci/jey258p317
Zhong X, Chen W, Shi Z, Huan Z, Ma L, Liu W et al (2020) Three-dimensional transesophageal echocardiography measurement of mitral valve area in patients with rheumatic mitral stenosis: multiplanar reconstruction or 3D direct planimetry. Int J Cardiovasc Imaging 37:99–107
Sadeghian H, Rezvanfard M, Jalali A (2019) Measurement of mitral valve area in patients with mitral stenosis by 3D echocardiography: a comparison between direct planimetry on 3D zoom and 3D quantification. Echocardiography 36(8):1509–1514
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Fleisher LA et al (2017) 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 70(2):252–289
Eibel S, Turton E, Mukherjee C, Bevilacqua C, Ender J (2017) Feasibility of measurements of valve dimensions in en-face-3D transesophageal echocardiography. Int J Cardiovasc Imaging 33(10):1503
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin Iii JP, Gentile F et al (2021) 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Am Coll Cardiol 77(4):e25–e197
Schlosshan D, Aggarwal G, Mathur G, Allan R, Cranney G (2011) Real-time 3D transesophageal echocardiography for the evaluation of rheumatic mitral stenosis. JACC: Cardiovasc Imaging 4(6):580–588
Min S-Y, Song J-M, Kim Y-J, Park H-K, Seo M-O, Lee M-S et al (2013) Discrepancy between mitral valve areas measured by two-dimensional planimetry and three-dimensional transoesophageal echocardiography in patients with mitral stenosis. Heart 99(4):253–258
Najih H, Arous S, Laarje A, Baghdadi D, Benouna MG, Azzouzi L et al (2016) Discordance between mitral valve area (MVA) and pressure gradient in patients with mitral valve stenosis: mean transmitral valve gradient is a severity index or a tolerance index of severity of mitralss valve stenosis. Pan Afr Med J 25:75
Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H et al (2012) Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 33(19):2451–2496
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA et al (2014) 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation 129(23):2440–2492
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The Authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Toufan Tabrizi, M., Faraji Azad, H., Khezerlouy-Aghdam, N. et al. Measurement of mitral valve area by direct three dimensional planimetry compared to multiplanar reconstruction in patients with rheumatic mitral stenosis. Int J Cardiovasc Imaging 38, 1341–1349 (2022). https://doi.org/10.1007/s10554-022-02523-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-022-02523-0