Abstract
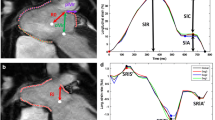
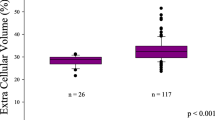
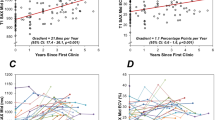
There is a known correlation between myocardial steatosis and heart function, but it is unclear how left ventricular diastolic function worsens over time in the myocardial steatosis setting. We sought to investigate whether intramyocardial fat deposition affects diastolic function over time. This was a retrospective analysis of patients who had undergone 1–3 echocardiography assessments between April 2011 and April 2017. Patients were divided into two groups: those with the presence of myocardial fat deposition in the left ventricular myocardium (assessed by having tissue within any 10-mm2 region with computed tomography values between − 190 and − 30 Hounsfield units; + MF), and those with absence of deposition not meeting the threshold (− MF). The rates of change of the standard early diastolic mitral annulus velocity (e′) and the transmitral early peak velocity (E)/e′ ratio at the second and third echocardiograph assessments were calculated relative to baseline. In total, 125 patients were eligible (+ MF, n = 39; − MF, n = 86) for inclusion. Compared with the − MF group, e′ was significantly lower and E/e′ was significantly higher in the + MF group at each scan timepoint, even when adjusted for body mass index and sex. A significant average decrease in e′ and increase in E/e′ was also observed in the + MF group across all scans compared with the − MF group. Myocardial steatosis was associated with an acceleration of decreased left ventricular diastolic function over time.


Similar content being viewed by others
Data availability
Data are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Hruby A, Hu FB (2015) The epidemiology of obesity: a big picture. Pharmacoeconomics 33(7):673–689. https://doi.org/10.1007/s40273-014-0243-x
Lakatta EG, Levy D (2003) Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part II: the aging heart in health: links to heart disease. Circulation 107(2):346–354. https://doi.org/10.1161/01.cir.0000048893.62841.f7
Lakatta EG (2003) Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part III: cellular and molecular clues to heart and arterial aging. Circulation 107(3):490–497. https://doi.org/10.1161/01.cir.0000048894.99865.02
Wei JY (1992) Age and the cardiovascular system. N Engl J Med 327(24):1735–1739. https://doi.org/10.1056/NEJM199212103272408
van der Meer RW, Rijzewijk LJ, Diamant M, Hammer S, Schär M, Bax JJ, Smit JW, Romijn JA, de Roos A, Lamb HJ (2008) The ageing male heart: myocardial triglyceride content as independent predictor of diastolic function. Eur Heart J 29(12):1516–1522. https://doi.org/10.1093/eurheartj/ehn207
Gaborit B, Kober F, Jacquier A, Moro PJ, Cuisset T, Boullu S, Dadoun F, Alessi MC, Morange P, Clément K, Bernard M, Dutour A (2012) Assessment of epicardial fat volume and myocardial triglyceride content in severely obese subjects: relationship to metabolic profile, cardiac function and visceral fat. Int J Obes (Lond) 36(3):422–430. https://doi.org/10.1038/ijo.2011.117
Rijzewijk LJ, van der Meer RW, Smit JW, Diamant M, Bax JJ, Hammer S, Romijn JA, de Roos A, Lamb HJ (2008) Myocardial steatosis is an independent predictor of diastolic dysfunction in type 2 diabetes mellitus. J Am Coll Cardiol 52(22):1793–1799. https://doi.org/10.1016/j.jacc.2008.07.062
Nyman K, Granér M, Pentikäinen MO, Lundbom J, Hakkarainen A, Sirén R, Nieminen MS, Taskinen MR, Lundbom N, Lauerma K (2013) Cardiac steatosis and left ventricular function in men with metabolic syndrome. J Cardiovasc Magn Reason 15(1):103. https://doi.org/10.1186/1532-429X-15-103
Nakae I, Mitsunami K, Yoshino T, Omura T, Tsutamoto T, Matsumoto T, Morikawa S, Inubushi T, Horie M (2010) Clinical features of myocardial triglyceride in different types of cardiomyopathy assessed by proton magnetic resonance spectroscopy: comparison with myocardial creatine. J Card Fail 16(10):812–822. https://doi.org/10.1016/j.cardfail.2010.05.006
Sharma S, Adrogue JV, Golfman L, Uray I, Lemm J, Youker K, Noon GP, Frazier OH, Taegtmeyer H (2004) Intramyocardial lipid accumulation in the failing human heart resembles the lipotoxic rat heart. FASEB J 18(14):1692–1700. https://doi.org/10.1096/fj.04-2263com
Cannavale G, Francone M, Galea N, Vullo F, Molisso A, Carbone I, Catalano C (2018) Fatty images of the heart: spectrum of normal and pathological findings by computed tomography and cardiac magnetic resonance imaging. Biomed Res Int 2018:5610347. https://doi.org/10.1155/2018/5610347
Kimura F, Matsuo Y, Nakajima T, Nishikawa T, Kawamura S, Sannohe S, Hagiwara N, Sakai F (2010) Myocardial fat at cardiac imaging: how can we differentiate pathologic from physiologic fatty infiltration? Radiographics 30(6):1587–1602. https://doi.org/10.1148/rg.306105519
Kimura N, Mochizuki J, Honma M, Fukuda T, Ueno Y, Akatsuki N, Michio T, Yoshiki H, Hitoyuki T (2013) Shinkin-nai shibō chinchaku ga kokoro kinō ni oyobosu eikyō [The influence of myocardial fat on cardiac function]. Chōonpakensa Gijutsu 38:375–380 ([in Japanese])
Snel M, Jonker JT, Schoones J, Lamb H, de Roos A, Pijl H, Smit JW, Meinders AE, Jazet IM (2012) Ectopic fat and insulin resistance: pathophysiology and effect of diet and lifestyle interventions. Int J Endocrinol 2012:983814. https://doi.org/10.1155/2012/983814
de Wit-Verheggen VHW, Altintas S, Spee RJM, Mihl C, van Kuijk SMJ, Wildberger JE, Schrauwen-Hinderling VB, Kietselaer BLJH, van de Weijer T (2020) Pericardial fat and its influence on cardiac diastolic function. Cardiovasc Diabetol 19(1):129. https://doi.org/10.1186/s12933-020-01097-2
Wei J, Nelson MD, Szczepaniak EW, Smith L, Mehta PK, Thomson LE, Berman DS, Li D, Bairey Merz CN, Szczepaniak LS (2016) Myocardial steatosis as a possible mechanistic link between diastolic dysfunction and coronary microvascular dysfunction in women. Am J Physiol Heart Circ Physiol 310(1):H14–H19. https://doi.org/10.1152/ajpheart.00612.2015
Widya RL, de Mutsert R, den Heijer M, le Cessie S, Rosendaal FR, Jukema JW, Smit JWA, de Roos A, Lamb HJ, for the NEO Study Group (2016) Association between hepatic triglyceride content and left ventricular diastolic function in a population-based cohort: The Netherlands Epidemiology of Obesity Study. Radiology 279(2):443–450. https://doi.org/10.1148/radiol.2015150035
Nyman K, Granér M, Pentikäinen MO, Lundbom J, Hakkarainen A, Sirén R, Nieminen MS, Taskinen MR, Lundbom N, Lauerma K (2013) Cardiac steatosis and left ventricular function in men with metabolic syndrome. J Cardiovasc Magn Reson 15(1):103. https://doi.org/10.1186/1532-429X-15-103
Granér M, Nyman K, Siren R, Pentikäinen MO, Lundbom J, Hakkarainen A, Lauerma K, Lundbom N, Nieminen MS, Taskinen MR (2015) Ectopic fat depots and left ventricular function in nondiabetic men with nonalcoholic fatty liver disease. Circ Cardiovasc Imaging 8(1):e001979. https://doi.org/10.1161/CIRCIMAGING.114.001979
Halliburton SS, Abbara S, Chen MY, Gentry R, Mahesh M, Raff GL, Shaw LJ, Hausleiter J (2011) SCCT guidelines on radiation dose and dose-optimization strategies in cardiovascular CT. J Cardiovasc Comput Tomogr 5(4):198–224. https://doi.org/10.1016/j.jcct.2011.06.001
Kvist H, Sjöström L, Tylén U (1986) Adipose tissue volume determinations in women by computed tomography: technical considerations. Int J Obes 10(1):53–67
Ma R, Ties D, van Assen M, Pelgrim GJ, Sidorenkov G, van Ooijen PMA, van der Harst P, van Dijk R, Vliegenthart R (2020) Towards reference values of pericoronary adipose tissue attenuation: impact of coronary artery and tube voltage in coronary computed tomography angiography. Eur Radiol 30(12):6838–6846. https://doi.org/10.1007/s00330-020-07069-0
Arques S, Roux E, Luccioni R (2007) Current clinical applications of spectral tissue Doppler echocardiography (E/E’ ratio) as a noninvasive surrogate for left ventricular diastolic pressures in the diagnosis of heart failure with preserved left ventricular systolic function. Cardiovasc Ultrasound 5:16. https://doi.org/10.1186/1476-7120-5-16
Van Buuren S, Groothius-Oudshoorn K (2021) Mice: multivariate imputation by chained equations. R package version 3.13.0. Available at: https://cran.r-project.org/web/packages/mice/mice.pdf
Liu CY, Bluemke DA, Gerstenblith G, Zimmerman SL, Li J, Zhu H, Lai S, Lai H (2014) Myocardial steatosis and its association with obesity and regional ventricular dysfunction: evaluated by magnetic resonance tagging and 1H spectroscopy in healthy African Americans. Int J Cardiol 172(2):381–387. https://doi.org/10.1016/j.ijcard.2014.01.074
Granér M, Siren R, Nyman K, Lundbom J, Hakkarainen A, Pentikäinen MO, Lauerma K, Lundbom N, Adiels M, Nieminen MS, Taskinen MR (2013) Cardiac steatosis associates with visceral obesity in nondiabetic obese men. J Clin Endocrinol Metab 98(3):1189–1197. https://doi.org/10.1210/jc.2012-3190
Lavie CJ, Milani RV, Ventura HO (2009) Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol 53(21):1925–1932. https://doi.org/10.1016/j.jacc.2008.12.068
Lakatta EG (2002) Age-associated cardiovascular changes in health: impact on cardiovascular disease in older persons. Heart Fail Rev 7(1):29–49. https://doi.org/10.1023/a:1013797722156
Cheitlin MD (2003) Cardiovascular physiology-changes with aging. Am J Geriatr Cardiol 12(1):9–13. https://doi.org/10.1111/j.1076-7460.2003.01751.x
Iozzo P (2011) Myocardial, perivascular, and epicardial fat. Diabetes Care. https://doi.org/10.2337/dc11-s250
Banerjee R, Rial B, Holloway CJ, Lewandowski AJ, Robson MD, Osuchukwu C, Schneider JE, Leeson P, Rider OJ, Neubauer S (2015) Evidence of a direct effect of myocardial steatosis on LV hypertrophy and diastolic dysfunction in adult and adolescent obesity. JACC Cardiovasc Imaging 8(12):1468–1470. https://doi.org/10.1016/j.jcmg.2014.12.019
Dokainish H, Zoghbi WA, Lakkis NM, Ambriz E, Patel R, Quinones MA, Nagueh SF (2005) Incremental predictive power of B-type natriuretic peptide and tissue Doppler echocardiography in the prognosis of patients with congestive heart failure. J Am Coll Cardiol 45(8):1223–1226. https://doi.org/10.1016/j.jacc.2005.01.025
Satpathy C, Mishra TK, Satpathy R, Satpathy HK, Barone E (2006) Diagnosis and management of diastolic dysfunction and heart failure. Am Fam Physician 73(5):841–846
Eisman AS, Shah RV, Dhakal BP, Pappagianopoulos PP, Wooster L, Bailey C, Cunningham TF, Hardin KM, Baggish AL, Ho JE, Malhotra R, Lewis GD (2018) Pulmonary capillary wedge pressure patterns during exercise predict exercise capacity and incident heart failure. Circ Heart Fail 11(5):e004750. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004750
Acknowledgements
We thank Clare Cox, PhD, and Tim Spelman, PhD, of Edanz for providing medical writing and statistical analysis support, respectively. No funding was received for this study.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the interpretation of the data and critical revision of the manuscript. All authors read and approved the final manuscript and agree to be accountable for the accuracy and integrity of the contents. Conception and design of the study and analysis of the data were performed by YH, YK, NK, and JM. Data acquisition was conducted by YK, NK, JM, SO, HM, and KH. YH contributed to the manuscript drafting.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This research study was conducted retrospectively from data obtained for clinical purposes. We consulted extensively with the IRB of Minamino Cardiovascular Hospital who determined that our study did not need ethical approval. An IRB official waiver of ethical approval was granted from the IRB of Minamino Cardiovascular Hospital.
Consent to participate
All patients provided written informed consent prior to their inclusion in the study.
Consent for publication
Not applicable. No individually identifiable patient data are included.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Some results of this study were previously presented at the 82nd Annual Scientific Meeting of the Japanese Circulation Society, March 23–25, 2018, Osaka, Japan. Data from the first scan of 26 of the 125 participants were included in a previous publication: Kimura et al.: The influence of myocardial fat on the cardiac function. Japanese Journal of Medical Ultrasound Technology 2013; 38:375–380.
Rights and permissions
About this article
Cite this article
Hata, Y., Koike, Y., Kimura, N. et al. Longitudinal effect of myocardial fat deposition on left ventricular diastolic function: a retrospective cohort study. Int J Cardiovasc Imaging 38, 955–961 (2022). https://doi.org/10.1007/s10554-021-02483-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-021-02483-x