Abstract
Purpose
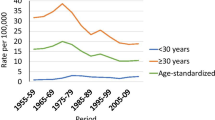
In an attempt to understand why cervical cancer (CC) survival is decreasing with diagnosis period among older women in France, this study aimed to estimate the effects of main prognostic factors on net survival in CC according to age.
Methods
French cancer registries databases were used to retrospectively analyze women diagnosed with CC in 2011–2012. Net survival was estimated with the Pohar-Perme method and prognostic factors (socio-demographic, clinical variables, stage at diagnosis, therapeutic management) were analyzed with Lambert and Royston’s flexible parametric model.
Results
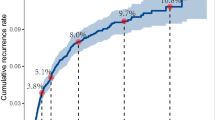
One thousand one hundred fifty three women with CC were identified. 30.4% were < 45, 41.4% 45–64, and 28.3% ≥ 65 years. Older women were diagnosed at a more advanced stage than younger women: 54.8% regional (FIGO IB2-IVA), 33.0% distant (IVB) in women ≥ 65 years vs 33.7% and 8.0%, respectively in women < 45 years. Half of women with regional stage of CC received recommended treatment; this rate decreased with increasing age (< 45: 66.1%, 45–64: 62.7%, ≥ 65: 29.2%). Older age was significantly associated with increased risk of death: hazard ratio 1.89 for age ≥ 65, as were regional stage (2.81), distant stage (15.99), and not receiving recommended treatment (2.26).
Conclusion
Older women with CC diagnosed at advanced stage who do not receive standard of care are at markedly increased risk of death. Special attention to the management of older women is warranted in France, not only to diagnose cancer at an earlier stage (via gynecological follow-up in these menopaused women who remain at risk of CC), but also to ensure they receive standard of care, taking into account their overall state of health.

Similar content being viewed by others
Data availability
The data can be made available upon reasonable request.
Abbreviations
- ADC:
-
Adenocarcinoma
- ASNS:
-
Age-standardized net survival
- CC:
-
Cervical cancer
- CCRB:
-
Concurrent chemoradiotherapy plus intracavitary brachytherapy
- CI:
-
Confidence interval
- EDI:
-
European Deprivation Index
- FIGO:
-
International Federation of Obstetrics and Gynecology
- HR:
-
Hazard ratio
- IARC:
-
International Agency for Research on Cancer
- INSEE:
-
Institut National de la Statistique et des Etudes Economiques
- IQR:
-
Interquartile range
- NS:
-
Net survival
- Q:
-
Quintile
- TNM:
-
Tumor Node Metastasis
- SCC:
-
Squamous cell carcinoma
- SEER :
-
Surveillance, Epidemiology, and End Results Program
- WHO:
-
World health organization
References
Defossez G, Le Guyader-Peyrou S, Uhry Z, Grosclaude P, Colonna M, Dantony E, et al (2019) National estimates of cancer incidence and mortality in metropolitan France between 1990 and 2018 [Internet]. Saint-Maurice: Santé publique France https://www.santepubliquefrance.fr/maladies-et-traumatismes/cancers/cancer-du-sein/documents/rapport-synthese/estimations-nationales-de-l-incidence-et-de-la-mortalite-par-cancer-en-france-metropolitaine-entre-1990-et-2018-volume-1-tumeurs-solides-etud. Accessed 10 May 2020
Bray F, Loos AH, McCarron P, Weiderpass E, Arbyn M, Møller H et al (2005) Trends in cervical squamous cell carcinoma incidence in 13 European countries: changing risk and the effects of screening. Cancer Epidemiol Biomarkers Prev 14:677–686. https://doi.org/10.1158/1055-9965.EPI-04-0569
Hamers F, Woronoff A-S, The French Network of Cancer Registries FRANCIM (2019) Cervical cancer in France: incidence and mortality trends until 2018. Bull Epidémiol Hebd 22–23:410–416
Cowppli-Bony A, Uhry Z, Remontet L, Voirin N, Guizard A-V, Trétarre B et al (2017) Survival of solid cancer patients in France, 1989–2013: a population-based study. Eur J Cancer Prev 26:461–468. https://doi.org/10.1097/CEJ.0000000000000372
Vercelli M, Lillini R, Capocaccia R, Micheli A, Coebergh JW, Quinn M et al (2006) Cancer survival in the elderly: effects of socio-economic factors and health care system features (ELDCARE project). Eur J Cancer 42:234–242. https://doi.org/10.1016/j.ejca.2005.07.032
Fedewa SA, Cokkinides V, Virgo KS, Bandi P, Saslow D, Ward EM (2012) Association of insurance status and age with cervical cancer stage at diagnosis: National Cancer Database, 2000–2007. Am J Public Health 102:1782–1790. https://doi.org/10.2105/AJPH.2011.300532
Bjurberg M, Holmberg E, Borgfeldt C, Flöter-Rådestad A, Dahm-Kähler P, Hjerpe E et al (2019) Primary treatment patterns and survival of cervical cancer in Sweden: a population-based Swedish Gynecologic Cancer Group Study. Gynecol Oncol 155:229–236. https://doi.org/10.1016/j.ygyno.2019.08.022
Quinn BA, Deng X, Colton A, Bandyopadhyay D, Carter JS, Fields EC (2019) Increasing age predicts poor cervical cancer prognosis with subsequent effect on treatment and overall survival. Brachytherapy 18:29–37. https://doi.org/10.1016/j.brachy.2018.08.016
Shimamoto K, Saito T, Kitade S, Tomita Y, Nagayama R, Yamaguchi S et al (2018) A study of treatments and outcomes in elderly women with cervical cancer. Eur J Obstet Gynecol Reprod Biol 228:174–179. https://doi.org/10.1016/j.ejogrb.2018.06.032
Lorin L, Bertaut A, Hudry D, Beltjens F, Roignot P, Bone-Lepinoy M-C et al (2015) About invasive cervical cancer: a French population based study between 1998 and 2010. Eur J Obstet Gynecol Reprod Biol 191:1–6. https://doi.org/10.1016/j.ejogrb.2015.04.007
Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, Whelan S (2008) International classification of diseases for oncology, 3rd edn. World Health Organization, Geneva
Bray F, Colombet M, Mery L, Piñeros M, Znaor A, Zanetti R et al (eds) (2017) Cancer Incidence in Five Continents, Vol. XI. Lyon: International Agency for Research on Cancer. https://ci5.iarc.fr. Accessed 18 May 2020
Sobin LH, Gospodarowicz MK, Wittekind C (2009) TNM classification of malignant tumours, 7th edn. Geneva, Wiley-Blackwell
Pecorelli S, Zigliani L, Odicino F (2009) Revised FIGO staging for carcinoma of the cervix. Int J Gynecol Obstet 105:107–108. https://doi.org/10.1016/j.ijgo.2009.02.009
Marth C, Landoni F, Mahner S, McCormack M, Gonzalez-Martin A, Colombo N et al (2017) Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 28:72–83. https://doi.org/10.1093/annonc/mdx220
Pornet C, Delpierre C, Dejardin O, Grosclaude P, Launay L, Guittet L et al (2012) Construction of an adaptable European transnational ecological deprivation index: the French version. J Epidemiol Community Health 66:982–989. https://doi.org/10.1136/jech-2011-200311
Arbyn M, Anttila A, Jordan J, Ronco G, Schenck U, Segnan N et al (2010) European guidelines for quality assurance in cervical cancer screening. Second Edition—summary document. Ann Oncol 21:448–458. https://doi.org/10.1093/annonc/mdp471
Perme MP, Stare J, Estève J (2012) On estimation in relative survival. Biometrics 68:113–120. https://doi.org/10.1111/j.1541-0420.2011.01640.x
Corazziari I, Quinn M, Capocaccia R (2004) Standard cancer patient population for age standardising survival ratios. Eur J Cancer 40:2307–2316. https://doi.org/10.1016/j.ejca.2004.07.002
Grafféo N, Castell F, Belot A, Giorgi R (2016) A log-rank-type test to compare net survival distributions: a test to compare net survival distributions. Biometrics 72:760–769. https://doi.org/10.1111/biom.12477
Lambert PC, Royston P (2009) Further development of flexible parametric models for survival analysis. Stata J 9:265–290. https://doi.org/10.1177/1536867X0900900206
Fantin R, Santamaría-Ulloa C, Barboza-Solís C (2020) Social inequalities in cancer survival: a population-based study using the Costa Rican Cancer Registry. Cancer Epidemiol 65(101695):1–8. https://doi.org/10.1016/j.canep.2020.101695
Ibfelt EH, Kjær SK, Høgdall C, Steding-Jessen M, Kjær TK, Osler M et al (2013) Socioeconomic position and survival after cervical cancer: influence of cancer stage, comorbidity and smoking among Danish women diagnosed between 2005 and 2010. Br J Cancer 109:2489–2495. https://doi.org/10.1038/bjc.2013.558
Bielska-Lasota M, Rossi S, Krzyżak M, Haelens A, Domenic A, De Angelis R et al (2020) Reasons for low cervical cancer survival in new accession European Union countries: a EUROCARE-5 study. Arch Gynecol Obstet 301:591–602. https://doi.org/10.1007/s00404-019-05412-5
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al. (eds.) (2020) SEER Cancer Statistics Review, 1975–2017, National Cancer Institute [Internet]. Accessed 19 May 2020 https://seer.cancer.gov/csr/1975_2017/index.html
Feldman S, Cook E, Davis M, Gershman ST, Hanchate A, Haas JS et al (2018) Cervical cancer incidence among elderly women in Massachusetts compared with younger women. J Low Genit Tract Dis 22:314–317. https://doi.org/10.1097/LGT.0000000000000435
Brookfield KF, Cheung MC, Lucci J, Fleming LE, Koniaris LG (2009) Disparities in survival among women with invasive cervical cancer: a problem of access to care. Cancer 115:166–178. https://doi.org/10.1002/cncr.24007
Albert A, Lee A, Allbright R, Vijayakumar S (2019) Impact of age on receipt of curative treatment for cervical cancer: an analysis of patterns of care and survival in a large, national cohort. J Geriatr Oncol 10:465–474. https://doi.org/10.1016/j.jgo.2018.10.005
Brun JL, Stoven-Camou D, Trouette R, Lopez M, Chene G, Hocké C (2003) Survival and prognosis of women with invasive cervical cancer according to age. Gynecol Oncol 1:395–401. https://doi.org/10.1016/s0090-8258(03)00501-8
Schad MD, Moore J, Camacho F, Anderson RT, Cantrell LA, Showalter TN (2019) Predictors of quality of care and survival in a three-state cohort of locally advanced cervical cancer patients and development of a predictive model to identify women at risk of incomplete treatment. Medicine. https://doi.org/10.1097/MD.0000000000016874
Wang W, Hou X, Yan J, Shen J, Lian X, Sun S et al (2017) Outcome and toxicity of radical radiotherapy or concurrent Chemoradiotherapy for elderly cervical cancer women. BMC Cancer 17:510. https://doi.org/10.1186/s12885-017-3503-2
Sarfati D, Koczwara B, Jackson C (2016) The impact of comorbidity on cancer and its treatment. CA Cancer J Clin 66:337–350. https://doi.org/10.3322/caac.21342
Emmett M, Gildea C, Nordin A, Hirschowitz L, Poole J (2018) Cervical cancer does the morphological subtype affect survival rates? J Obstet Gynaecol 38:548–555. https://doi.org/10.1080/01443615.2017.1379062
Benard VB, Watson M, Saraiya M, Harewood R, Townsend JS, Stroup AM et al (2017) Cervical cancer survival in the United States by race and stage (2001–2009): findings from the CONCORD-2 study. Cancer 123:5119–5137. https://doi.org/10.1002/cncr.30906
Ioka A, Tsukuma H, Ajiki W, Oshima A (2005) Influence of age on cervical cancer survival in Japan. Jpn J Clin Oncol 35:464–469. https://doi.org/10.1093/jjco/hyi125
Haelens A, Roche L, Bastos J, Woronoff A-S, Zorzi M, Francart J (2017) Trends in net survival from cervical cancer in six European Latin countries: results from the SUDCAN population-based study. Eur J Cancer Prev 26:S92–S99. https://doi.org/10.1097/CEJ.0000000000000292
Jackson R, Wang L, Jembere N, Murphy J, Kupets R (2019) Why Do Women Get Cervical Cancer in an Organized Screening Program in Canada? J Low Genit Tract Dis 23:1–6. https://doi.org/10.1097/LGT.0000000000000450
Coker AL, Du XL, Fang S, Eggleston KS (2006) Socioeconomic status and cervical cancer survival among older women: findings from the SEER–Medicare linked data cohorts. Gynecol Oncol 102:278–284. https://doi.org/10.1016/j.ygyno.2005.12.016
Tron L, Belot A, Fauvernier M, Remontet L, Bossard N, Launay L et al (2019) Socioeconomic environment and disparities in cancer survival for 19 solid tumor sites: an analysis of the French Network of Cancer Registries (FRANCIM) data. Int J Cancer 144:1262–1274. https://doi.org/10.1002/ijc.31951
Sharma C, Deutsch I, Horowitz DP, Hershman DL, Lewin SN, Lu Y-S et al (2012) Patterns of care and treatment outcomes for elderly women with cervical cancer. Cancer 118:3618–3626. https://doi.org/10.1002/cncr.26589
Yang J, Cai H, Xiao Z-X, Wang H, Yang P (2019) Effect of radiotherapy on the survival of cervical cancer patients: an analysis based on SEER database. Medicine 98:e16421. https://doi.org/10.1097/MD.0000000000016421
Diaz A, Baade PD, Valery PC, Whop LJ, Moore SP, Cunningham J et al (2018) Comorbidity and cervical cancer survival of Indigenous and non-Indigenous Australian women: a semi-national registry-based cohort study (2003–2012). PLoS ONE 13(5):e0196764. https://doi.org/10.1371/journal.pone.0196764
Brewer N, Borman B, Sarfati D, Jeffreys M, Fleming ST, Cheng S et al (2011) Does comorbidity explain the ethnic inequalities in cervical cancer survival in New Zealand? A retrospective cohort study. BMC Cancer 11:1–7. https://doi.org/10.1186/1471-2407-11-132
Acknowledgments
The authors thank all those who contributed to the inclusion of cancer patients in the registries, in particular pathologists, medical informatics staff in public and private healthcare institutions, medical staff of health insurance companies, chest physicians and oncologists, as well as medical practitioners. French cancer registries are supported by the Institut National du Cancer, Santé Publique France, Direction Générale de l'Offre de Soins, local institutions and League Against Cancer. The authors thank Fiona Ecarnot, PhD (EA3920, University of Franche-Comté, Besançon, France) for translation and editorial assistance. The authors also thank Morgane Mounier for her advice on the choice of statistical model.
Funding
This study was partly supported for data collection and analysis by a grant from the French National Cancer Institute (INCa), related to the DEPREV-2017 program. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: Anne-Sophie Woronoff, Elisabeth Monnet; Methodology: Anne-Sophie Woronoff, Zoéwendtalé Cyrille Compaoré, Elisabeth Monnet, Aurélie Gérazime; Data curation: Anne-Sophie Woronoff, Zoéwendtalé Cyrille Compaoré, Aurélie Gérazime; Formal analysis: Anne-Sophie Woronoff, Zoéwendtalé Cyrille Compaoré, Aurélie Gérazime; Investigation: Anne-Sophie Woronoff, Florence Molinié, Anne-Valérie Guizard, Patricia Delafosse Tienhan Sandrine Dabakuyo-Yonli, Brigitte Trétarre. Gaëlle Coureau, Karima Hamas, Sandrine Plouvier, Simona Bara, Gautier Défossez, Bénédicte Lapôtre-Ledoux, Laetitia Daubisse-Marliac, Tania d’Almeida; Project administration: Anne-Sophie Woronoff; Writing—original draft preparation: Zoéwendtalé Cyrille Compaoré, Anne-Sophie Woronoff; Writing—review and editing: Zoéwendtalé Cyrille Compaoré, Anne-Sophie Woronoff, Elisabeth Monnet, Aurélie Gérazime, Florence Molinié, Anne-Valérie Guizard, Patricia Delafosse Tienhan Sandrine Dabakuyo-Yonli, Guy Launoy, Laura Mansi, Brigitte Trétarre; Funding acquisition: Anne-Sophie Woronoff; Resources: Anne-Sophie Woronoff, Florence Molinié, Anne-Valérie Guizard, Patricia Delafosse Tienhan Sandrine Dabakuyo-Yonli, Brigitte Trétarre. Gaëlle Coureau, Karima Hamas, Sandrine Plouvier, Simona Bara, Gautier Défossez, Bénédicte Lapôtre-Ledoux, Laetitia Daubisse-Marliac, Tania d’Almeida; Supervision and validation: Anne-Sophie Woronoff, Elisabeth Monnet.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Consent for publication
Not applicable. In accordance with French legislation governing medical research, no ethics committee approval was required for this registry-based study. The Registry has approval from the French national commission for data privacy for the ongoing collection of data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Morphology codes [12]
According to the IARC’s Cancer Incidence in five continents volume XI (CI5-XI), tumors were classified as:
-
Squamous cell carcinoma: [8050–8078], [8083–8084].
-
Adenocarcinoma: [8140–8141], [8190–8211], [8230–8231], [8260–8265], 8310, 8380, [8382–8384], [8440–8490], [8570–8574], 8576.
-
Other specified and unspecified: 8000, 8010, 8013, 8020, 8033, 8041, 8045, 8082, 8089, 8098, 8120, 8144, 8246, 8430, 8560, 8720, 8740.
Appendix 2: Condensed stage into 3 groups according to correspondence between TNM and FIGO [13]
Stage FIGO | T | N | M |
|---|---|---|---|
Localized | |||
Stage I | T1 | N0 | M0 |
Stage IA | T1a | N0 | M0 |
Stage IA1 | T1a1 | N0 | M0 |
Stage IA2 | T1a2 | N0 | M0 |
Stage IB | T1b | N0 | M0 |
Stage IB1 | T1b1 | N0 | M0 |
Regional | |||
Stage IB2 | T1b2 | N0 | M0 |
Stage II | T2 | N0 | M0 |
Stage IIA | T2a | N0 | M0 |
Stage IIA1 | T2a1 | N0 | M0 |
Stage IIA2 | T2a2 | N0 | M0 |
Stage IIB | T2b | N0 | M0 |
Stage III | T3 | N0 | M0 |
Stage IIIA | T3a | N0 | M0 |
Stage IIIB | T3b | Any N | M0 |
T1, T2, T3 | N1 | ||
Stage IVA | T4 | Any N | M0 |
Distant | |||
Stage IVB | Any T | Any N | M1 |
Rights and permissions
About this article
Cite this article
Compaoré, Z.C., Monnet, E., Gérazime, A. et al. To what extent do age, stage and treatment influence survival after invasive cervical cancer: a French population-based study. Cancer Causes Control 33, 403–415 (2022). https://doi.org/10.1007/s10552-021-01536-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-021-01536-9