Abstract
Purpose
Sedentary behavior has been previously shown, in a cross-sectional study, to have deleterious associations with biomarkers of postmenopausal breast cancer risk. We examined the associations of change in sedentary behavior [daily television (TV) viewing time, h/day] over a 5-year period with putative markers of postmenopausal breast cancer risk.
Methods
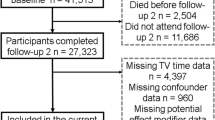
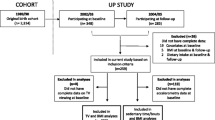
The analytic cohort consisted of 1,001 postmenopausal women from the Australian Diabetes, Obesity and Lifestyle (AusDiab) study (1999–2005). Multivariate linear regression models were used to examine associations of change in TV viewing time with biomarkers of the following risk mechanisms: adiposity (body mass index [BMI], waist circumference); metabolic dysfunction (fasting plasma glucose, 2-h plasma glucose, fasting insulin, insulin resistance [homeostasis model assessment of insulin resistance (HOMA-IR)]); and inflammation (high-sensitivity C-reactive protein (hs-CRP)). All analyses were adjusted for age, baseline TV viewing, and potential confounders.
Results
Hourly increments of change in TV viewing time were positively associated with BMI (β = 0.50, 95 % CI 0.20, 0.81; p = 0.001), waist circumference (β = 1.18, 95 % CI 0.49, 1.87; p = 0.001), fasting insulin (β = 38.13 %, 95 % CI 37.08, 39.20; p = 0.01) and HOMA-IR (β = 37.93 %, 95 % CI 36.92, 38.98; p = 0.03) in fully adjusted models. Significant associations with BMI, waist circumference, fasting insulin and HOMA-IR were also present in analyses using categories of change in TV viewing time (reduced, same, increased).
Conclusions
The findings suggest that increasing habitual sedentary behavior over time could increase breast cancer risk among postmenopausal women. Further investigation into the role of sedentary behavior in breast cancer etiology is warranted.


Similar content being viewed by others
References
Dunstan DW, Howard B, Healy GN, Owen N (2012) Too much sitting—a health hazard. Diabetes Res Clin Pract 97(3):368–376
Archer E, Shook RP, Thomas DM, Church TS, Katzmarzyk PT, Hébert JR et al (2013) 45-year trends in women’s use of time and household management energy expenditure. PLoS One 8(2). doi:10.1371/journal.pone.0056620
Depp CA, Schkade DA, Thompson WK, Jeste DV (2010) Age, affective experience, and television use. Am J Prev Med 39(2):173–178. doi:10.1016/j.amepre.2010.03.020
Matthews CE, George SM, Moore SC, Bowles HR, Blair A, Park Y et al (2012) Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr 95(2):437–445
Patel AV, Bernstein L, Deka A, Spencer Fiegelson H, Campbell PT, Gapstur SM et al (2010) Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol 172:419–429
van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A (2012) Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med 172(6):494–500. doi:10.1001/archinternmed.2011.2174
Hu FB, Leitzmann MF, Stampfer MJ, Colditz GA, Willett WC, Rimm EB (2001) Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch Intern Med 161(12):1542–1548
Hu FB, Li TY, Colditz GA, Willett WC, Manson JE (2003) Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA 289(14):1785–1791. doi:10.1001/jama.289.14.1785
Wijndaele K, Healy GN, Dunstan DW, Barnett AG, Salmon J, Shaw JE et al (2010) Increased cardiometabolic risk is associated with increased TV viewing time. Med Sci Sports Exerc 42(8):1511–1518. doi:10.1249/MSS.0b013e3181d322ac
Hansen ALS, Wijndaele K, Owen N, Magliano DJ, Thorp AA, Shaw JE et al (2012) Adverse associations of increases in television viewing time with 5-year changes in glucose homoeostasis markers: the AusDiab study. Diabetes Med 29(7):918–925. doi:10.1111/j.1464-5491.2012.03656.x
Gardiner PA, Healy GN, Eakin EG, Clark BK, Dunstan DW, Shaw JE et al (2011) Associations between television viewing time and overall sitting time with the metabolic syndrome in older men and women: the Australian Diabetes Obesity and Lifestyle Study. J Am Geriatr Soc 59(5):788–796. doi:10.1111/j.1532-5415.2011.03390.x
Lynch BM (2010) Sedentary behavior and cancer: a systematic review of the literature and proposed biological mechanisms. Cancer Epidemiol Biomark Prev 19(11):2691–2709. doi:10.1158/1055-9965.EPI-10-0815
Lynch BM, Friedenreich CM, Winkler EAH, Healy GN, Vallance JK, Eakin EG et al (2011) Associations of objectively assessed physical activity and sedentary time with biomarkers of breast cancer risk in postmenopausal women: findings from NHANES (2003–2006). Breast Cancer Res Treat 130(1):183–194
Dunstan DW, Zimmet PZ, Welborn TA, Cameron AJ, Shaw J, de Courten M et al (2002) The Australian Diabetes, Obesity and Lifestyle Study (AusDiab)—methods and response rates. Diabetes Res Clin Pract 57(2):119–129. doi:10.1016/S0168-8227(02)00025-6
Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling. Diabetes Care 27(6):1487–1495. doi:10.2337/diacare.27.6.1487
Hodge A, Maple-Brown L, Cunningham J, Boyle J, Dunbar T, Weeramanthri T et al (2010) Abdominal obesity and other risk factors largely explain the high CRP in Indigenous Australians relative to the general population, but not gender differences: a cross-sectional study. BMC Public Health 10(1). doi:10.1186/1471-2458-10-700
Hodge A, Patterson AJ, Brown WJ, Ireland P, Giles G (2000) The Anti Cancer Council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. ANZ J Public Health 24(6):576–583
Giles G, Ireland P (1996) Dietary Questionnaire for epidemiological studies, vol 2. The Cancer Council Victoria, Melbourne
Haines PS, Siega-Riz AM, Popkin BM (1999) The Diet Quality Index revised: a measurement instrument for populations. J Am Diet Assoc 99(6):697–704. doi:10.1016/S0002-8223(99)00168-6
McNaughton SA, Dunstan DW, Ball K, Shaw J, Crawford D (2009) Dietary quality is associated with diabetes and cardio-metabolic risk factors. J Nutr 139(4):734–742. doi:10.3945/jn.108.096784
Brown WJ, Trost SG, Bauman A, Mummery K, Owen N (2004) Test–retest reliability of four physical activity measures used in population surveys. J Sci Med Sport 7(2):205–215. doi:10.1016/s1440-2440(04)80010-0
Australian Institute of Health and Welfare (2003) The Active Australia Survey: a guide and manual for implementation, analysis and reporting. AIHW: Canberra
Twisk JWR (2003) Applied longitudinal data analysis for epidemiology: a practical guide. Cambridge University Press, Cambridge
Saunders TJ, Tremblay MS, Despres J-P, Bouchard C, Tremblay A, Chaput J-P (2013) Sedentary behaviour, visceral fat accumulation and cardiometabolic risk in adults: a 6-year longitudinal study from the Quebec Family Study. PLoS One 8(1). doi:10.1371/journal.pone.0054225
Wijndaele K, Duvigneaud N, Matton L, Duquet W, Delecluse C, Thomis M et al (2009) Sedentary behaviour, physical activity and a continuous metabolic syndrome risk score in adults. Eur J Clin Nutr 63(3):421–429
Thorp AA, Healy GN, Owen N, Salmon J, Ball K, Shaw JE et al (2010) Deleterious associations of sitting time and television viewing time with cardiometabolic risk biomarkers Australian Diabetes, Obesity and Lifestyle (AusDiab) study 2004–2005. Diabetes Care 33(2):327–334. doi:10.2337/dc09-0493
Cleary MP, Grossmann ME (2009) Obesity and breast cancer: the estrogen connection. Endocrinology 150(6):2537–2542. doi:10.1210/en.2009-0070
Lovejoy JC, Champagne CM, de Jonge L, Xie H, Smith SR (2008) Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes 32(6):949–958. doi:10.1038/ijo.2008.25
Santosa S, Jensen MD (2013) Adipocyte fatty acid storage factors enhance subcutaneous fat storage in postmenopausal women. Diabetes 62(3):775–782
James RE, Lukanova A, Dossus L, Becker S, Rinaldi S, Tjønneland A et al (2011) Postmenopausal serum sex steroids and risk of hormone receptor-positive and -negative breast cancer: a Nested Case–Control Study. Cancer Prev Res 4(10):1626–1635
Lann D, LeRoith D (2008) The role of endocrine insulin-like growth factor-I and insulin in breast cancer. J Mammary Gland Biol Neoplasia 13(4):371–379. doi:10.1007/s10911-008-9100-x
Pinto Pereira SM, Ki M, Power C (2012) Sedentary behaviour and biomarkers for cardiovascular disease and diabetes in mid-life: the role of television-viewing and sitting at work. PLoS One 7(2). doi:10.1371/journal.pone.0031132
Lapice E, Maione S, Patti L, Cipriano P, Rivellese AA, Riccardi G et al (2009) Abdominal adiposity is associated with elevated C-reactive protein independent of BMI in healthy nonobese people. Diabetes Care 32(9):1734–1736. doi:10.2337/dc09-0176
Silva DC, Costa LO, Vasconcelos AA, Cerqueira JC, Fantato D, Torres DC et al (2014) Waist circumference and menopausal status are independent predictors of endothelial low-grade inflammation. Endocr Res 39(1):22–25. doi:10.3109/07435800.2013.797431
Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR et al (2008) Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol 167(7):875–881
Winzer BM, Whiteman DC, Reeves MM, Paratz JD (2011) Physical activity and cancer prevention: a systematic review of clinical trials. Cancer Causes Control 22(6):811–826. doi:10.1007/s10552-011-9761-4
Healy GN, Clark BK, Winkler EAH, Gardiner PA, Brown WJ, Matthews CE (2011) Measurement of adults’ sedentary time in population-based studies. Am J Prev Med 41(2):216–227. doi:10.1016/j.amepre.2011.05.005
Salmon J, Owen N, Crawford D, Bauman A, Sallis JF (2003) Physical activity and sedentary behavior: population-based study of barriers, enjoyment, and preference. Health Psychol 22:178–188
Clark BK, Sugiyama T, Healy GN, Salmon J, Dunstan DW, Owen N (2009) Validity and reliability of measures of television viewing time and other non-occupational sedentary behaviour of adults: a review. Obes Rev 10(1):7–16
Acknowledgments
Lynch and Cameron are supported by Early Career Fellowships from the National Health and Medical Research Council (586727 and 1013313). Dunstan is supported by a Future Fellowship from the Australian Research Council (FT100100918). Baker IDI Heart and Diabetes Institute receives support from the Victorian Government’s Operational Infrastructure Support Program. The AusDiab study, co-coordinated by Baker IDI Heart and Diabetes Institute, gratefully acknowledges the generous support given by National Health and Medical Research Council (NHMRC Grant 233200), Australian Government Department of Health and Ageing, Abbott Australasia Pty Ltd, Alphapharm Pty Ltd, AstraZeneca, Bristol-Myers Squibb, City Health Centre-Diabetes Service—Canberra, Department of Health and Community Services—Northern Territory, Department of Health and Human Services—Tasmania, Department of Health—New South Wales, Department of Health—Western Australia, Department of Health—South Australia, Department of Human Services—Victoria, Diabetes Australia, Diabetes Australia Northern Territory, Eli Lilly Australia, Estate of the Late Edward Wilson, GlaxoSmithKline, Jack Brockhoff Foundation, Janssen-Cilag, Kidney Health Australia, Marian and FH Flack Trust, Menzies Research Institute, Merck Sharp and Dohme, Novartis Pharmaceuticals, Novo Nordisk Pharmaceuticals, Pfizer Pty Ltd, Pratt Foundation, Queensland Health, Roche Diagnostics Australia, Royal Prince Alfred Hospital, Sydney, Sanofi Aventis, Sanofi Synthelabo. The AusDiab study was also supported in part by the Victorian Government’s OIS Program. We acknowledge the AusDiab project manager Shirley Murray and administrative associate Sue Fournel for the contribution to the study. We also thank the field coordinators Marita Dalton (1999–2000), Theresa Whalen (2004–2005) and Annaliese Bonney (2004–2005), as well as all the AusDiab support staff from 1999/2000 and 2004/2005. We would like to thank the participants for volunteering their time to participate in the AusDiab study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All Australian legal and ethical standards and protocols were adhered to during the implementation of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wiseman, A.J., Lynch, B.M., Cameron, A.J. et al. Associations of change in television viewing time with biomarkers of postmenopausal breast cancer risk: the Australian Diabetes, Obesity and Lifestyle Study. Cancer Causes Control 25, 1309–1319 (2014). https://doi.org/10.1007/s10552-014-0433-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-014-0433-z