Abstract
Purpose
Endocrine therapy (ET) in combination with CDK 4/6 inhibitors (CDK 4/6i) is the standard treatment modality for hormone receptor (HR)-positive and HER2-negative metastatic breast cancer (mBC). There is uncertainty about the prognostic and predictive value of HER2-low status and whether HER2-low BC is an individual biologic subtype. In this study, we aimed to investigate the prognostic effect of HER2 expression status on survival in mBC patients treated with first-line ET plus CDK 4/6i.
Methods
This multicenter retrospective study included patients with HR + /HER2-negative mBC cancer who were treated with first-line CDK 4/6i in combination with ET from January 2016 to March 2023. Patients were divided into two groups (HER2-low and zero), and survival and safety analyses were performed.
Results
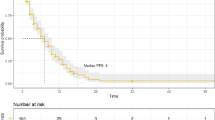
A total of 201 patients were included in this study; of these, 73 (36.3%) had HER2-low disease and 128 (63.7%) had HER2-zero. There were 135 patients (67.2%) treated with ribociclib and 66 (32.8%) with palbociclib. Most of the patients (75.1%) received aromatase inhibitors as combination-endocrine therapy. Baseline characteristics were similar between the two groups. The median follow-up was 19.1 months (range: 2.5–78.4). The most common side effect was neutropenia (22.4%). The frequency of grade 3–4 toxicity was similar between the HER2-zero and low patients (32% vs 31.5%; p = 0.939). Visceral metastases were present in 44.8% of patients. Between the HER2-low and zero groups, median PFS (25.2 vs 22.6 months, p = 0.972) and OS (not reached vs 37.5 months, p = 0.707) showed no statistically significant differences.
Conclusion
The prognostic value of HER2-low status remains controversial. Our study showed no significant effect of HER2 low expression on survival in patients receiving CDK 4/6i plus ET.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the 2020 data from the global cancer database, female breast cancer (BC) surpassed lung cancer and was the most common type of cancer in the world [1]. BC is also one of the leading causes of death among women. Although mBC is still not a curable disease, new therapy agents have led to encouraging results in survival. BC is a very heterogeneous disease, consisting of different biological subtypes with different prognoses. Gene expression profiling studies have shown that breast cancer consists of six main intrinsic subgroups (luminal A, luminal B, basal-like, HER2-enriched, normal breast-like, and claudin-low) [2, 3]. The treatment decision in mBC is generally based on the hormone receptor (HR) and human epidermal growth factor receptor 2 (HER2) receptor results.
HER2 overexpression is observed in approximately 15–20% of all breast cancer patients and is known to be associated with a poor prognosis before the era of anti-HER2 therapy [4]. HER2 low expression is present in approximately 45–55% of HER2-negative mBC patients [5]. Patients with HER2 scores of + 1 and + 2 by immunohistochemistry (IHC) and without HER2 gene amplification by in situ hybridization (ISH) are defined as having HER2-low disease [6]. There is some evidence suggesting that patients with low HER2 expression should be evaluated as a separate subgroup of BC [7]. The different biological characteristics of HER2-low disease or its direct effects on prognosis are not fully known, and there is no consensus on this issue. Although positive results were not obtained with anti-HER2 treatments in this subgroup until recent years, the positive results of trastuzumab-deruxtecan, a new drug-antibody conjugate, on survival in HER2-low disease shown in the DESTINY 04 Breast study have led to increased interest in this subgroup [8].
According to the results of the PALOMA [9,10,11], MONARCH [12, 13], and MONALEESA [14,15,16] studies published in recent years, the use of cyclin-dependent kinase 4 and 6 inhibitors (CDK 4/6i) plus ET has become the first-line standard treatment in most patients with HR-positive, HER2-negative BC [17]. It is known that there is crosstalk between the HER2 and HR pathways, and HER2 expression can be modulated even in the absence of gene amplification [18, 19]. The presence of this bidirectional crosstalk between HR and HER2 may be one of the reasons for resistance to ET. In some studies conducted among BC patients receiving neoadjuvant chemotherapy, it was observed that pathological complete response rates were lower in the HER2-low group compared to HER2-zero [20]. Among patients with HR + /HER2-negative mBC, the effects of low HER2 expression on the efficacy of CDK 4/6i are not yet fully known, and there are limited and controversial data in the literature.
In our multicenter study, we aimed to investigate the effects of HER2 status on progression-free survival (PFS) and overall survival (OS) in HR + /HER2-negative mBC patients using CDK 4/6i as the first-line treatment.
Materials and methods
Patients
Patients who were diagnosed with mBC and treated with first-line CDK 4/6i in combination with ET combination therapy between January 2016 and March 2023 in four different oncology clinics were evaluated retrospectively. Baseline data were extracted from databases and medical records. Inclusion criteria were: 1) histopathologically confirmed BC; 2) radiologically proven metastatic disease; 3) HR + /HER2-negative disease proven by IHC staining and ISH; 4) ET plus CDK 4/6i used in the first line. Exclusion criteria were defined as: 1) Less than 3 cycles of CDK 4/6i treatment; 2) Patients who discontinued follow-up in our clinics; 3) Missing treatment response assessment.
HR and HER2 receptor evaluations were performed in each center's own pathology laboratory. In accordance with the American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP) guidelines, patients with IHC + 1, + 2 and no gene amplification by ISH were considered to have HER2-low disease. ER or PR positivity was determined to be > 10% in IHC. Receptor results were based on biopsy results either from the primary tumor or metastatic site (whichever was available). Patients were divided into two groups: HER2-low and HER2-zero. If HER2-low expression was detected in one of the biopsy results obtained from the primary tumor or metastatic area, the patient was included in the HER2-low group. Age at diagnosis, menopausal status, detection of metastatic disease in denovo or recurrent disease, hormone levels, number of metastatic sites, presence of visceral or non-visceral metastasis, which ET they received with CDK 4/6i, grade ≥ 3 toxicities were evaluated. PFS and OS differences between the two groups, treatment-related toxicities and dose reduction rates were analyzed. Objective responses to treatment could not be evaluated because the study was multicentre and the evaluation could not be performed optimally according to Response Evaluation Criteria in Solid Tumors (RECIST) criteria.
This study was approved by the local ethics committee for clinical trials (date: July 12, 2023 and number: E-83045809–604.01.01–731418), and the need for informed consent was waived because of the retrospective nature of this study.
Statistical analysis
The characteristics of the patients were compared with the Fisher or Chi-squared test for categorical data and a t-test for continuous data. OS was defined as the time from the initiation of CDK 4/6i until death from any cause. PFS was defined as the time from the initiation of CDK 4/6i to the date of radiological progression or death from any cause. No-event patients were censored at the end of the last follow-up. Survival curves were estimated by the Kaplan–Meier method and compared with the log-rank test. Cox regression was used to analyze the hazard ratios for PFS and OS. Statistical tests were two-sided, and a p-value less than 0.05 was considered statistically significant. The statistical analyses were conducted using SPSS version 26.
Results
Characteristics of patients
Our study included 201 patients. All patients were female. There were 128 (63.7%) patients in the HER2-zero group and 73 (36.3%) patients in the HER2-low group. The median follow-up time was 19.1 months (range: 2.5–78.4 months). The median age was 55 years (range: 26–82). The median age was similar between the two groups (54 vs 58 years, p = 0.702). The baseline characteristics of the patients are displayed in Table 1. Upon examination of histological subgroups, it was shown that the invasive ductal carcinoma subtype accounted for the majority, comprising 76.6% of cases. Approximately 2/3 of the patients had received ribociclib treatment. The numbers of patients treated with ribociclib or palbociclib were similar between the HER2-zero and low groups. All patients had received CDK 4/6i plus ET as a first-line treatment in the metastatic setting. Most patients (66.7%) were postmenopausal at the time of diagnosis. Although 120 patients (59.7%) had metastatic disease at the time of diagnosis, 81 patients (40.3%) developed metastatic disease at the time of recurrence, and the median time to reccurrence is 62.6 months (range: 12.6–278.7 months). There was no significant difference between the median ER (%) levels between the two groups. The majority of patients (75.1%) received an aromatase inhibitor (AI) treatment in combination with CDK 4/6i.
Metastases were present in three or more anatomical sites in 120 patients (59.7%) and in one or two sites in 81 patients (40.3%). A significant proportion of the patients (44.8%) had visceral organ metastases. Visceral and non-visceral organ involvement was similar between the two groups. A total of 13 patients had brain metastases, 8 of whom were in the HER2-zero group and 5 in the HER2-low group. In 73 patients (36.3%), the diagnosis was confirmed by biopsy from the metastatic site. The distributions of sites are summarized in Table 2.
The evaluation of adverse events during treatment revealed that 64 individuals (31.8%) developed grade 3 or higher toxicity. Neutropenia was the most common adverse event (22.4%). Thrombocytopenia developed in 3 patients, anemia in 5 patients, QT prolongation in 5 patients, diarrhea in 2 patients, hepatitis in 2 patients, and nephropathy in 2 patients. Grade 4 toxicity (hepatitis and neutropenia) developed in two patients. In 49 (24.3%) patients, a dose reduction was performed due to toxicity. The dose reduction rate was similar between the HER2-zero and low groups (26.6% vs 20.5%, p = 0.34). There was no significant difference in toxicities between the HER2-zero and low groups (32% vs 31.5%; p = 0.939). There were no treatment-related mortalities or unexpected adverse events.
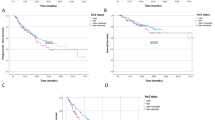
Survival analyses
Patients with HER2-low disease had similar PFS when compared to patients with HER2-zero BC (median PFS: 25.2 vs 22.6 months; HR 0.99, 95% CI: 0.64–1.53, p = 0.972). The median OS in the HER2-low group was not reached (NR), but in the HER2-zero group it was seen to be 37.5 months. There was no statistically significant difference in median OS between the HER2-low and zero groups (HR 0.87, 95% CI: 0.44–1.75, p = 0.707). Survival analyses are shown in Fig. 1.
Discussion
CDK 4/6i + ET combination therapy is the standard treatment regimen used in HR + /HER2-negative mBC, both in first-line and later-line settings. Low expression of HER2 is observed at a rate of ~ 60% among all BC patients [7]. In recent years, there has been data supporting the evaluation of HER2-low disease as a different entity [7, 20,21,22]. In a study by Schettini et al. evaluating 3689 patients, it was observed that low HER2 expression was more frequent in HR-positive disease than in triple-negative breast cancer (TNBC) (65.4% vs 36.5%, p < 0.001), and HER2-low patients were significantly associated with more nodal involvement and a larger primary tumor diameter compared to HER2-zero [5]. In another analysis of 523 patients analyzing genomic data, significant differences were observed between gene mutations seen in HER2-low and zero disease [23]. In this study, patients with low HER2 expression were more frequent in the HR-positive subgroup and had lower Ki67 expression levels than HER2-zero. In the same study, it was shown that PI3K-Akt signal pathway mutations were more frequent in the HER2-low group, and checkpoint factors, Fanconi anemia, p53 signaling, and cell cycle pathway mutations were more frequent in the HER2-zero group. After the use of antibody–drug conjugates such as trastuzumab deruxtecan in HER2-positive patients and the demonstration of its efficacy in HER2-low patients, interest in this subgroup has increased.
It has been observed that HER2-low disease is detected more frequently in HR-positive breast cancer patients than in the HR-negative group [20, 24]. Data have been published showing that low HER2 expression is associated with both lower pathological complete response rates (pCR) and worse survival in HR + BC patients receiving neoadjuvant chemotherapy. In a pooled analysis of four neoadjuvant chemotherapy trials involving a total of 2310 patients, it was observed that pCR rates were significantly lower in patients with HER2 low expression in the HR-positive subgroup compared to HER2-zero (17.5% vs 23.6%, p = 0.024), while there was no significant difference between the two groups in the HR-negative subgroup [20]. There are data supporting the existence of bidirectional crosstalk between HER2 and HR pathways as a potential mechanism of hormonal resistance and unfavorable outcomes on survival [18].
In our study, there were 36.3% of patients with low HER2 expression. Compared to previous studies [25,26,27,28], this rate was lower in our research. There could be several factors leading to this occurrence. One of them is the absence of a centralized pathology assessment. A recent study shows the lack of concordance between pathologists in distinguishing tumors with a HER2 score of 0 and those with a score of 1 + [29]. Another possible factor is that not all recurrent metastatic patients undergo a re-biopsy.
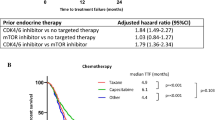
We investigated the effects of first-line ET in combination with CDK 4/6i treatment on OS and PFS in HER2-low and zero groups in patients with metastatic HR + /HER2-negative BC and we found no significant difference between the two groups in both OS and PFS. The literature has discrepancies in the findings of retrospective studies on this issue. Similar to the results in our study, Yildirim et al. conducted a multicenter retrospective analysis with 204 patients, and they found no significant impact of low HER2 expression on survival [30]. In another study conducted with a small group of patients, no significant difference was observed between objective response rates (ORR) in the HER2-low and zero patient groups [31].
Zattarin et al. [27] retrospectively evaluated 436 patients who received CDK 4/6i in the first line of the metastatic disease. In this study, it was observed that low HER2 expression was associated with poor OS and PFS, independent of other risk factors. In a retrospective analysis of 106 patients by Bao et al. [25], 77.3% of patients had HER2 low expression, and this subgroup had a shorter PFS (8.9 vs 18.8 months, p = 0.01) compared to HER2-zero patients. In this study, most patients (84.9%) were treated with palbociclib, and only half of the patients received first-line CDK 4/6 inhibitors.
It's not yet clear what the prognostic value of HER2 expression status is in HR + /HER2-negative mBC that is treated by CDK 4/6i plus ET. Studies on this subject in the literature are limited to retrospective analyses. Various factors might be responsible for the disparities shown in the findings of the studies. The assessment of HER2 status using different methodologies may be the most crucial among these factors. Another possible reason for the observed disparities among studies might originate from alterations to the patient group, including disparities in tumor-related parameters. A recent review evaluated nine retrospective analyses encompassing 2705 individuals [32]. The findings revealed a statistically significant increase in the risk of disease progression and death among patients with mBC who had low expression of HER2 and were treated with CDK 4/6 inhibitors.
Our study has several limitations that result from its retrospective design, which encompasses selection bias. Another limitation of our study is the short follow-up time for an optimal evaluation of survival outcomes. We consider the absence of centralization in the HER2 expression evaluation to constitute a significant limitation of our study that may have contributed to discrepancies in the results. According to the latest ASCO/CAP guideline, cases with tumor cell staining between 1 and 10% should be classified as ER-low positive [33]. However, in our country, insurance coverage for CDK 4/6 inhibitors is limited to patients with ER levels exceeding 10%. Therefore, patients classified as ER-low were not included in our study. Approximately 2 − 3% of breast cancers have been reported to be ER-low and there is limited data on the overall benefit of endocrine therapy in these patients [34]. Consequently, we suspect the exclusion of this patient subgroup from our study may have influenced our results.
In conclusion, our multicenter research suggests that low HER2 expression does not significantly affect survival outcomes in HR + mBC patients treated with first-line ET plus CDK4/6 inhibitors. Prospective analyses are needed to more accurately evaluate the effects of HER2 expression levels on treatment responses and survival in mBC patients treated with CDK 4/6 inhibitors.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72:7–33. https://doi.org/10.3322/caac.21708
Prat A, Parker JS, Karginova O et al (2010) Phenotypic and molecular characterization of the claudin-low intrinsic subtype of breast cancer. Breast Cancer Res. https://doi.org/10.1186/bcr2635
Sørlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. https://doi.org/10.1073/pnas.191367098
Seshadri R, Firgaira FA, Horsfall DJ et al (1993) Clinical significance of HER-2/neu oncogene amplification in primary breast cancer. J Clin Oncol. https://doi.org/10.1200/JCO.1993.11.10.1936
Schettini F, Chic N, Brasó-Maristany F et al (2021) Clinical, pathological, and PAM50 gene expression features of HER2-low breast cancer. NPJ Breast Cancer. https://doi.org/10.1038/s41523-020-00208-2
Wolff AC, Elizabeth M, Hammond H et al (2018) Human epidermal growth factor receptor 2 testing in breast cancer: American society of clinical oncology/college of American pathologists clinical practice guideline focused update. J Clin Oncol 36:2105–2122. https://doi.org/10.1200/JCO
Tarantino P, Hamilton E, Tolaney SM, et al (2020) HER2-Low Breast Cancer: Pathological and Clinical Landscape
Modi S, Jacot W, Yamashita T et al (2022) Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med 387:9–20. https://doi.org/10.1056/nejmoa2203690
Cristofanilli M, Turner NC, Bondarenko I et al (2016) Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol 17:425–439. https://doi.org/10.1016/S1470-2045(15)00613-0
Rugo HS, Finn RS, Gelmon K et al (2020) Progression-free survival outcome is independent of objective response in patients with estrogen receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer treated with palbociclib plus letrozole compared with letrozole: analysis from PALOMA-2. Clin Breast Cancer 20:e173–e180. https://doi.org/10.1016/j.clbc.2019.08.009
Finn RS, Crown JP, Lang I et al (2015) The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): A randomised phase 2 study. Lancet Oncol 16:25–35. https://doi.org/10.1016/S1470-2045(14)71159-3
Goetz MP, Toi M, Campone M et al (2017) MONARCH 3: Abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol 35:3638–3646. https://doi.org/10.1200/JCO
Dickler MN, Tolaney SM, Rugo HS et al (2017) MONARCH 1, a phase II study of abemaciclib, a CDK4 and CDK6 inhibitor, as a single agent, n patients with refractory HR+/HER2- metastatic breast cancer. Clin Cancer Res 23:5218–5224. https://doi.org/10.1158/1078-0432.CCR-17-0754
Lu YS, Im SA, Colleoni M et al (2022) Updated overall survival of ribociclib plus endocrine therapy versus endocrine therapy alone in pre- and perimenopausal patients with HR+/HER2- advanced breast cancer in MONALEESA-7: A phase III randomized clinical trial. Clin Cancer Res 28:851–859. https://doi.org/10.1158/1078-0432.CCR-21-3032
Hortobagyi GN, Stemmer SM, Burris HA et al (2018) Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann Oncol 29:1541–1547. https://doi.org/10.1093/annonc/mdy155
Slamon DJ, Neven P, Chia S et al (2021) Ribociclib plus fulvestrant for postmenopausal women with hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer in the phase III randomized MONALEESA-3 trial: updated overall survival. Ann Oncol 32:1015–1024. https://doi.org/10.1016/j.annonc.2021.05.353
Mcandrew NP, Finn RS (2021) Clinical review on the management of hormone receptor-positive metastatic breast cancer. JCO Oncol Pract 18:319–327. https://doi.org/10.1200/OP.21
Giuliano M, Trivedi MV, Schiff R (2013) Bidirectional crosstalk between the estrogen receptor and human epidermal growth factor receptor 2 signaling pathways in breast cancer: Molecular basis and clinical implications. Breast Care 8:256–262
Osborne CK, Shou J, Massarweh S, Schiff R (2005) Crosstalk between estrogen receptor and growth factor receptor pathways as a cause for endocrine therapy resistance in breast cancer. Clin Cancer Res 11:865s-s870
Denkert C, Seither F, Schneeweiss A et al (2021) Clinical and molecular characteristics of HER2-low-positive breast cancer: pooled analysis of individual patient data from four prospective, neoadjuvant clinical trials. Lancet Oncol 22:1151–1161. https://doi.org/10.1016/S1470-2045(21)00301-6
Agostinetto E, Rediti M, Fimereli D et al (2021) Her2-low breast cancer: Molecular characteristics and prognosis. Cancers (Basel). https://doi.org/10.3390/cancers13112824
Mutai R, Barkan T, Moore A et al (2021) Prognostic impact of HER2-low expression in hormone receptor positive early breast cancer. Breast 60:62–69. https://doi.org/10.1016/j.breast.2021.08.016
Zhang G, Ren C, Li C et al (2022) Distinct clinical and somatic mutational features of breast tumors with high-, low-, or non-expressing human epidermal growth factor receptor 2 status. BMC Med. https://doi.org/10.1186/s12916-022-02346-9
De Calbiac O, Lusque A, Mailliez A et al (2022) Comparison of management and outcomes in ERBB2 -low vs ERBB2 -zero metastatic breast cancer in France. JAMA Netw Open 5:E2231170. https://doi.org/10.1001/jamanetworkopen.2022.31170
Bao KKH, Sutanto L, Tse SSW et al (2021) The association of ERBB2 -low expression with the efficacy of cyclin-dependent kinase 4/6 inhibitor in hormone receptor-positive, ERBB2 -negative metastatic breast cancer. JAMA Netw Open 4:e2133132. https://doi.org/10.1001/jamanetworkopen.2021.33132
Sharaf B, Abu-Fares H, Tamimi F et al (2023) Differences in treatment outcomes between patients with HER2-Low versus HER2-Zero, hormone receptor-positive advanced-stage breast cancer treated with ribociclib. Breast Cancer 15:541–548. https://doi.org/10.2147/BCTT.S415432
Zattarin E, Presti D, Mariani L et al (2023) Prognostic significance of HER2-low status in HR-positive/HER2-negative advanced breast cancer treated with CDK4/6 inhibitors. NPJ Breast Cancer. https://doi.org/10.1038/s41523-023-00534-1
Douganıotıs G, Kesısıs G, Lalla E et al (2022) Prognostic significance of low HER2 expression in patients with metastatic hormone receptor-positive breast cancer treated with first line CDK4/6 ınhibitors: a greek multicenter real-world data analysis. Cancer Diagnosis Prognosis 2:585–591
Fernandez AI, Liu M, Bellizzi A et al (2022) Examination of Low ERBB2 protein expression in breast cancer tissue. JAMA Oncol 8:1–4. https://doi.org/10.1001/jamaoncol.2021.7239
Caliskan Yildirim E, Atag E, Coban E et al (2023) The effect of low HER2 expression on treatment outcomes in metastatic hormone receptor positive breast cancer patients treated with a combination of a CDK4/6 inhibitor and endocrine therapy: A multicentric retrospective study. Breast 70:56–62. https://doi.org/10.1016/j.breast.2023.06.006
Shao Y, Luo Z, Yu Y et al (2022) HER2-low expression does not affect the clinical outcomes of metastatic breast cancer treated with CDK4/6 inhibitor: A real-world study. Front Endocrinol (Lausanne). https://doi.org/10.3389/fendo.2022.1000704
Guven DC, Sahin TK (2024) The association between HER2-low status and survival in patients with metastatic breast cancer treated with Cyclin-dependent kinases 4 and 6 inhibitors: a systematic review and meta-analysis. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-023-07226-1
Allison KH, Elizabeth; M, Hammond H, et al (2020) Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP Guideline Update. J Clin Oncol. https://doi.org/10.1200/JCO.19
Kim MC, Park MH, Choi JE et al (2022) Characteristics and prognosis of estrogen receptor low-positive breast cancer. J Breast Cancer 25:318–326. https://doi.org/10.4048/jbc.2022.25.e31
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK). The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Murad Guliyev: Conceptualization, data curation, writing-original draft preparation. Ali Ahadzade, İlkay Gültürk, Nargiz Majidova, Goncagül Akdağ: Material preparation, data collection. Gülin Alkan Şen: Visualization, investigation. The first draft of the manuscript was written by Murad Guliyev and all authors commented on previous versions of the manuscript. Hande Turna: Supervision, editing. Nebi Serkan Demirci: Reviewing and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of İstanbul University Cerrahpaşa (Date: July 12, 2023 and Number: E-83045809–604.01.01–731418).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guliyev, M., Şen, G.A., Gültürk, İ. et al. The effects of low HER2 expression on survival in patients with metastatic breast cancer treated with CDK 4/6 inhibitors: a multicenter retrospective study. Breast Cancer Res Treat 205, 633–640 (2024). https://doi.org/10.1007/s10549-024-07291-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-024-07291-0