Abstract
Purpose
Many women diagnosed with breast cancer have survived previous cancer; yet little is known about the impact of previous cancer on overall and cancer-specific survival.
Methods
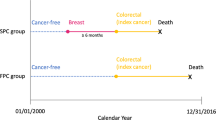
This population-based cohort study using SEER-Medicare data included women (age ≥ 66 years) diagnosed with breast cancer between 2005 and 2015. Separately by breast cancer stage, we estimated effect of previous cancer on overall survival using Cox regression and on cause-specific survival using competing risk regression; all survival analyses adjusted for covariates.
Results
Of 138,576 women diagnosed with breast cancer, 8% had a previous cancer of another organ site, most commonly colorectal or uterine cancer or melanoma. Many of these women (46.3%) were diagnosed within 5 years of breast cancer. For all breast cancer stages except IV wherein there was no difference, women with vs. without previous cancer had worse overall survival. This survival disadvantage was driven by deaths due to the previous cancer and other causes. In contrast, women with previous cancer generally had favorable breast-cancer-specific survival, although this varied by stage. Overall survival varied by previous cancer type, timing, and stage; previous lung cancer, cancer diagnosed within 1 year of incident breast cancer, and previous cancer at a distant stage were associated with the worst survival. In contrast, women with a previous melanoma had equivalent overall survival to women without previous cancer.
Conclusion
We observed variable impact of previous cancer on overall and breast-cancer-specific survival depending on breast cancer stage at diagnosis and the type, timing, and stage of previous cancer.




Similar content being viewed by others
Data availability
This study used SEER-MEDICARE data. The Centers for Medicare and Medicaid Services do not allow the redistribution of their data by researchers. SEER-MEDICARE data are distinct from the publicly available SEER database, and can be obtained by researchers, by following the process described on https://healthcaredelivery.cancer.gov/seermedicare/obtain/requests.html (access requirements include Institutional Review Board approval and the completion of a Data Use Agreement).
Code availability
Available upon request.
References
Bluethmann SM, Mariotto AB, Rowland JH (2016) Anticipating the “silver tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomark Prev 25(7):1029–1036
Glicksman AS (2013) Fulton JP (2013) Metachronous cancer. R I Med J 96(4):41–44
Weir HK, Johnson CJ, Thompson TD (2013) The effect of multiple primary rules on population-based cancer survival. Cancer Causes Control 24(6):1231–1242. https://doi.org/10.1007/s10552-013-0203-3
Ye Y, Neil AL, Wills KE, Venn AJ (2016) Temporal trends in the risk of developing multiple primary cancers: a systematic review. BMC Cancer 16(1):849. https://doi.org/10.1186/s12885-016-2876-y
Jin S, Pazdur R, Sridhara R (2017) Re-evaluating eligibility criteria for oncology clinical trials: analysis of investigational new drug applications in 2015. J Clin Oncol 35(33):3745–3752. https://doi.org/10.1200/JCO.2017.73.4186
Gerber DE, Laccetti AL, Xuan L, Halm EA, Pruitt SL (2014) Impact of prior cancer on eligibility for lung cancer clinical trials. J Natl Cancer Inst. https://doi.org/10.1093/jnci/dju302
Perez M, Murphy CC, Rashdan S, Pruitt SL, Gerber DE (in preparation) Excluding women with prior cancer diagnoses from breast cancer clinical trials: a prevalent but poorly understood practice
Howerton MW, Gibbons MC, Baffi CR, Gary TL, Lai GY, Bolen S, Tilburt J, Tanpitukpongse TP, Wilson RF, Powe NR, Bass EB, Ford JG (2007) Provider roles in the recruitment of underrepresented populations to cancer clinical trials. Cancer 109(3):465–476. https://doi.org/10.1002/cncr.22436
Lara PN Jr, Higdon R, Lim N, Kwan K, Tanaka M, Lau DH, Wun T, Welborn J, Meyers FJ, Christensen S, O’Donnell R, Richman C, Scudder SA, Tuscano J, Gandara DR, Lam KS (2001) Prospective evaluation of cancer clinical trial accrual patterns: identifying potential barriers to enrollment. J Clin Oncol 19(6):1728–1733. https://doi.org/10.1200/JCO.2001.19.6.1728
Gotay CC (1991) Accrual to cancer clinical trials: directions from the research literature. Soc Sci Med 33(5):569–577
IOM Institute of Medicine (2010) A national cancer clinical trials system for the 21st century: reinvigorating the NCI Cooperative Group program. The National Academies Press, Washington, DC
Simon MS, Du W, Flaherty L, Philip PA, Lorusso P, Miree C, Smith D, Brown DR (2004) Factors associated with breast cancer clinical trials participation and enrollment at a large academic medical center. J Clin Oncol 22(11):2046–2052. https://doi.org/10.1200/JCO.2004.03.005
Tournoux C, Katsahian S, Chevret S, Levy V (2006) Factors influencing inclusion of patients with malignancies in clinical trials. Cancer 106(2):258–270. https://doi.org/10.1002/cncr.21613
Murthy VH, Krumholz HM, Gross CP (2004) Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA 291(22):2720–2726. https://doi.org/10.1001/jama.291.22.2720
Breastcancer.org, Ardmore. https://www.breastcancer.org/treatment/clinical_trials/. Accessed 17 Dec 2020
American Cancer Society cancer facts and figures 2020. American Cancer Society, Atlanta. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf. Accessed 28 May 2020
Murphy CC, Gerber DE, Pruitt SL (2018) Prior cancer among persons newly diagnosed with cancer: an initial report from the Surveillance, Epidemiology, and End Results program. JAMA Oncol 4(6):832–836. https://doi.org/10.1001/jamaoncol.2017.3605
American Cancer Society breast cancer facts and figures 2019–2020. American Cancer Society, Atlanta. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf. Accessed 28 May 2020
Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence—SEER Research Data. National Cancer Institute, DCCPS, Surveillance Research Program. Age at diagnosis calculated based on SEER 18 data using November 2017 submission. www.seer.cancer.gov
Lichtman SM, Harvey RD, Damiette Smit MA, Rahman A, Thompson MA, Roach N, Schenkel C, Bruinooge SS, Cortazar P, Walker D, Fehrenbacher L (2017) Modernizing clinical trial eligibility criteria: recommendations of the American Society of Clinical Oncology-Friends of Cancer Research organ dysfunction, prior or concurrent malignancy, and comorbidities working group. J Clin Oncol. https://doi.org/10.1200/JCO.2017.74.4102
Kim ES, Bruinooge SS, Roberts S, Ison G, Lin NU, Gore L, Uldrick TS, Lichtman SM, Roach N, Beaver JA, Sridhara R, Hesketh PJ, Denicoff AM, Garrett-Mayer E, Rubin E, Multani P, Prowell TM, Schenkel C, Kozak M, Allen J, Sigal E, Schilsky RL (2017) Broadening eligibility criteria to make clinical trials more representative: American Society of Clinical Oncology and Friends of Cancer Research joint research statement. J Clin Oncol 35(33):3737–3744. https://doi.org/10.1200/JCO.2017.73.7916
Cancer clinical trial eligibility criteria: patients with organ dysfunction or prior or concurrent malignancies. Draft guidance released March 2019 (2019). U.S. Department of Health and Human Services, Food and Drug Administration, Oncology Center of Excellence, Center for Drug Evaluation and Research and Center for Biologics Evaluation and Research, Washington, DC. https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm. Accessed 28 May 2020
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF (2002) Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. https://doi.org/10.1097/01.MLR.0000020942.47004.03
Laccetti AL, Pruitt SL, Xuan L, Halm EA, Gerber DE (2015) Effect of prior cancer on outcomes in advanced lung cancer: implications for clinical trial eligibility and accrual. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djv002
Pruitt SL, Gerber DE, Zhu H, Heitjan DF, Maddineni B, Xiong D, Singal AG, Tavakkoli A, Halm EA, Murphy CC. Survival of patients newly diagnosed with colorectal cancer and with a history of previous cancer (Under Review)
Lund JL, Sturmer T, Harlan LC, Sanoff HK, Sandler RS, Brookhart MA, Warren JL (2013) Identifying specific chemotherapeutic agents in Medicare data: a validation study. Med Care 51(5):e27–e34. https://doi.org/10.1097/MLR.0b013e31823ab60f
Koroukian SM, Dahman B, Copeland G, Bradley CJ (2010) The utility of the state buy-in variable in the Medicare denominator file to identify dually eligible Medicare-Medicaid beneficiaries: a validation study. Health Serv Res 45(1):265–282. https://doi.org/10.1111/j.1475-6773.2009.01051.x
Nieman CL, Pitman KT, Tufaro AP, Eisele DW, Frick KD, Gourin CG (2018) The effect of frailty on short-term outcomes after head and neck cancer surgery. Laryngoscope 128(1):102–110. https://doi.org/10.1002/lary.26735
Nass Sharyl J MHLaMJ (2010) Healthcare Delivery Research Program. Comorbidity SAS Macro (2014 version). National Cancer Institute, Division of Cancer Control and Population Sciences. https://healthcaredelivery.cancer.gov/seermedicare/considerations/macro-2014.html. Accessed 5 March 2019
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43(11):1130–1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509
SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA
R Core Team (2017) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. https://www.R-project.org/. Accessed 17 Nov 2020
Ji F, Yang CQ, Li XL, Zhang LL, Yang M, Li JQ, Gao HF, Zhu T, Cheng MY, Li WP, Wu SY, Zhong AL, Wang K (2020) Risk of breast cancer-related death in women with a prior cancer. Aging (Albany NY) 12(7):5894–5906. https://doi.org/10.18632/aging.102984
Kim BK, Oh SJ, Song JY, Lee HB, Park MH, Jung Y, Park WC, Lee J, Sun WY, Soc KBC (2018) Clinical characteristics and prognosis associated with multiple primary cancers in breast cancer patients. J Breast Cancer 21(1):62–69. https://doi.org/10.4048/jbc.2018.21.1.62
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics. CA Cancer J Clin 70(1):7–30. https://doi.org/10.3322/caac.21590
Zhou H, Huang Y, Qiu Z, Zhao H, Fang W, Yang Y, Zhao Y, Hou X, Ma Y, Hong S, Zhou T, Zhang Y, Zhang L (2018) Impact of prior cancer history on the overall survival of patients newly diagnosed with cancer: a pan-cancer analysis of the SEER database. Int J Cancer 143(7):1569–1577. https://doi.org/10.1002/ijc.31543
Lin C, Wu J, Ding S, Goh C, Andriani L, Shen K, Zhu L (2019) Impact of prior cancer history on the clinical outcomes in advanced breast cancer: a propensity score-adjusted, population-based study. J Korean Cancer Assoc. https://doi.org/10.4143/crt.2019.210
Adamo MB, Dickie L, Ruhl J (2018) SEER program coding and staging manual 2018. National Cancer Institute, U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute, Bethesda. https://seer.cancer.gov/manuals/2018/SPCSM_2018_maindoc.pdf. Accessed 9 March 2020
Acknowledgements
The authors also acknowledge the efforts of the Applied Research Program, NCI; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database. Contents of this paper are solely the responsibility of the authors and do not necessarily represent the official view of the NIH.
Funding
This work was supported by the National Cancer Institute (NCI) (R01CA229834-02 to SLP and K24CA201543 to DEG).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data analysis was performed by BM. The first draft of the manuscript was written by SP and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
DH reports consulting for Braintree Labs, Creatics LLC, Abbott Labs, and Macrogenics, Inc., and legal consulting for Noven and Women’s Talc Project; AR reports consulting and advisory board for Hologic and research grant and educational speaker for Accuray; and DEG reports research funding from Astra-Zeneca, BerGenBio, and Karyopharm, Gilead stock ownership and consulting for Samsung Bioepis and Catalyst Pharmaceuticals. SLP, HZ, BM, DX, AT, EAH, and CCM have no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pruitt, S.L., Zhu, H., Heitjan, D.F. et al. Survival of women diagnosed with breast cancer and who have survived a previous cancer. Breast Cancer Res Treat 187, 853–865 (2021). https://doi.org/10.1007/s10549-021-06122-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06122-w