Abstract
Purpose
Time to surgery (TTS) is a potentially modifiable factor associated with survival after breast cancer diagnosis and can serve as a proxy for quality of oncologic care coordination. We sought to determine whether factors associated with delays in TTS vary between patients who receive neoadjuvant systemic therapy (NST) vs upfront surgery and whether the impact of these delays on overall survival (OS) varies with treatment sequence.
Methods
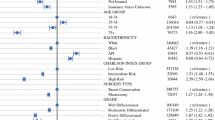
Women ≥ 18 years old with Stage I–III breast cancer were identified in the National Cancer Database (2004–2014). Multivariate linear regression stratified by treatment sequence (upfront surgery vs NST [neoadjuvant chemotherapy {NAC}, neoadjuvant endocrine therapy {NAE}, or both {NACE}]) was used to identify factors associated with TTS. Cox proportional hazards models were used to estimate the effect of TTS on overall survival (OS).
Results
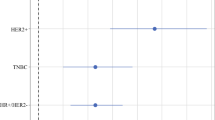
Of 693,469 patients, 14.8% (n = 102,326) received NST (NAC n = 85,143, NAE n = 10,004, NACE n = 7179). Non-White race/ethnicity, no or government-issued insurance, more extensive surgery (i.e., mastectomy and contralateral prophylactic mastectomy vs breast-conserving surgery), and post-mastectomy reconstruction were associated with significantly longer adjusted TTS for NAC and upfront-surgery recipients, but only upfront-surgery patients had progressively worse OS with increasing TTS (> 180 vs ≤ 30 days: HR = 1.31, all p < 0.001).
Conclusions
Surgery extent, race/ethnicity, and insurance were associated with TTS across treatment groups, but longer TTS was only associated with worse OS in upfront-surgery patients. Our findings can help inform surgeon–patient communication, shared decision making, care coordination, and patients’ expectations throughout both NST and in the perioperative period.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the National Cancer Database (NCDB) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the NCDB.
References
Siu AL (2016) Force USPST screening for breast cancer: U.S. preventive services task force recommendation statement. Ann Intern Med. 164:279–296
Hendrick RE, Baker JA, Helvie MA (2019) Breast cancer deaths averted over 3 decades. Cancer 125(9):1482–1488
Canadian Task Force On Preventive Health Care, Tonelli M, Connor GS, et al. Recommendations on screening for breast cancer in average‐risk women aged 40–74 years. CMAJ 2011; 183:1991–2001.
Rosselli Del Turco M, Ponti A, Bick U et al (2010) Quality indicators in breast cancer care. Eur J Cancer 46(13):2344–2356
Wagner JL, Warneke CL, Mittendorf EA et al (2011) Delays in primary surgical treatment are not associated with significant tumor size progression in breast cancer patients. Ann Surg 254(1):119–124
Brazda A, Estroff J, Euhus D et al (2010) Delays in time to treatment and survival impact in breast cancer. Ann Surg Oncol 17(Suppl 3):291–296
Neal RD, Tharmanathan P, France B et al (2015) Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review Br J Cancer 112(Suppl 1):92–107
Eaglehouse YL, Georg MW, Shriver CD et al (2019a) Time-to-surgery and overall survival after breast cancer diagnosis in a universal health system. Br Cancer Res Treat 178(2):441–450
Bleicher RJ, Ruth K, Sigurdson ER et al (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330–339
Smith EC, Ziogas A, Anton-Culver H et al (2013) Delay in surgical treatment and survival after breast cancer diagnosis in young women by race/ethnicity. JAMA Surg 148(6):516–523
Eaglehouse YL, Georg MW, Shriver CD et al (2019b) Racial differences in time to breast cancer surgery and overall survival in the US military health system. JAMA Surg 154(3):e185113
Solomon M, Cochrane CT, Grieve DA et al (2015) Insurance status and time to completion of surgery for breast cancer. ANZ J Surg 86(1–2):84–87
Landercasper J, Linebarger JH, Ellis RL et al (2010) A quality review of the timeliness of breast cancer diagnosis and treatment in an integrated breast center. J Am Coll Surg 210(4):449–455
Murphy BL, Day CN, Hoskin TL et al (2018) Neoadjuvant chemotherapy use in breast cancer is greatest in excellent responders: triple-negative and HER2+ subtypes. Ann Surg Oncol 25(8):2241–2248
American College of Surgeons. National Cancer Database. 1996–2016 [cited January 22, 2020]. Available at: https://www.facs.org/quality%20programs/cancer/ncdb.
Jagsi R, Jiang J, Momoh AO et al (2014) Trends and variation in use of breast reconstruction in patients with breast cancer undergoing mastectomy in the United States. J Clin Oncol 32(9):919–926
Cemal Y, Albornoz CR, Disa JJ et al (2013) A paradigm shift in the U.S. breast reconstruction part 2 The influence of changing mastectomy patterns on reconstructive rate and method. Plast Reconstr Surg. 131(3):320e–326e
Jabo B, Lin AC, Aljehani MA et al (2018) Impact of breast reconstruction on time to definitive surgical treatment, adjuvant therapy, and breast cancer outcomes. Ann Surg Oncol 25(10):3096–3105
Omarini C, Guaitoli G, Noventa S et al (2017) Impact of time to surgery after neoadjuvant chemotherapy in operable breast cancer patients. Eur J Surg Oncol 43(4):613–618
Sanford RA, Lei X, Barcenas CH et al (2016) Impact of time from completion of neoadjuvant chemotherapy to surgery on survival outcomes in breast cancer patients. Ann Surg Oncol 23(5):1515–1521
Suleman K, Almalik O, Haque E et al. Does the timing of surgery after neoadjuvant therapy in breast cancer patients affect the outcome? Oncology. 2020; 1–6.
Fisher B, Brown A, Mamounas E et al (1997) Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol 15(7):2483–2493
Van der Hage JA, Van de Velde CJ, Julien JP et al (2001) Preoperative chemotherapy in primary operable breast cancer: results from the European organization for research and treatment of cancer trial 10902. J Clin Oncol 19:4224–4237
Rastogi P, Anderson SJ, Bear HD et al (2008) Preoperative chemotherapy: updates of national surgical adjuvant breast and bowel project protocols B-18 and B-27. J Clin Oncol 26(5):778–785
Cortazar P, Zhang L, Untch M et al (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384:164–172
Boughey JC, McCall LM, Ballman KV et al (2014) Tumor biology correlates with rates of breast-conserving surgery and pathologic complete response after neoadjuvant chemotherapy for breast cancer: findings from the ACOSOG (Alliance) Z1071 Prospective Multicenter Clinical Trial. Ann Surg 260:608–614
Fayanju OM, Ren Y, Thomas SM et al (2018) The clinical significance of breast-only and node-only pathologic complete response (pCR) after neoadjuvant chemotherapy (NACT): a review of 20,000 breast cancer patients in the National Cancer Data Base (NCDB). Ann Surg 268(4):591–601
Von Minckwitz G, Untch M, Blohmer JU et al (2012) Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol 30(15):1796–1804
Spring LM, Gupta A, Reynolds KL et al (2016) Neoadjuvant endocrine therapy for estrogen-receptor-positive breast cancer: a systematic review and meta-analysis. JAMA Oncol 2(11):1477–1486
Balic M, Thomssen C, St WR, Gallen V et al (2019) a brief summary of the consensus discussion on the optimal primary breast cancer treatment. Breast Care 2019(14):103–110
Barroso-Sousa R, Silva DD, Alessi JV et al (2016) Neoadjuvant endocrine therapy in breast cancer: current role and future perspectives. Ecancermedicalscience 10:609. https://doi.org/10.3332/ecancer.2016.609
Andersen BL, Cacioppo JT (1995) Delay in seeking a cancer diagnosis: delay stages and psychophysiological comparison processes. The British journal of social psychology 34(1):33–52
Walter F, Webster A, Scott S, Emery J (2012) The Andersen Model of Total Patient Delay: a systematic review of its application in cancer diagnosis. J Health Serv Res Policy 17(2):110–118
Gooiker GA, van Gijn W, Post PN, van de Velde CJ, Tollenaar RA, Wouters MW (2010) A systematic review and meta-analysis of the volume-outcome relationship in the surgical treatment of breast cancer Are breast cancer patients better of with a high volume provider? Eur J Surg Oncol. 36(1):S27-35
Greenup RA, Obeng-Gyasi S, Thomas S et al (2018) The effect of hospital volume on breast cancer mortality. Ann Surg 267:375–381
Reeder-Hayes KE, Anderson BO (2017) Breast cancer disparities at home and abroad: a review of the challenges and opportunities for system-level change. Clin Cancer Res 23(11):2655–2664
Sheppard VB, Oppong BA, Hampton R et al (2015) Disparities in breast cancer surgery delay: the lingering effect of race. Ann Surg Oncol 22(9):2902–2911
Tammemagi CM (2007) Racial/ethnic disparities in breast and gynecologic cancer treatment and outcomes. Curr Opin Obstet Gynecol 19:31–36
Shaves VL, Brown ML (2002) Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst 94:332–357
Sutton TL, Schlitt A, Gardiner SK, Johnson N, Garreau JR. Time to Surgery Following Neoadjuvant Chemotherapy for Breast Cancer Impacts Residual Cancer Burden, Recurrence, and Survival. Society of Surgical Oncology (SSO) International Conference on Surgical Cancer; 2020.
Funding
Dr. Fayanju is supported by the National Institutes of Health (NIH) under Award Number 1K08CA241390 (PI: Fayanju). This work is also supported by the Duke Cancer Institute through NIH grant P30CA014236 (PI: Kastan). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Ipshita Prakash, Rachel A. Greenup, Jennifer K. Plichta, Laura H. Rosenberger, and Oluwadamilola M. Fayanju declare that they have no conflicts of interest to disclose. Samantha M. Thomas and Terry Hyslop were previously consultants for AbbVie.
Ethical approval
This retrospective study involving de-identified data from human participants was conducted in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The institutional review board (IRB) at Duke University determined that our study did not need ethical approval, and our study was granted exempt status with a waiver of informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Prakash, I., Thomas, S.M., Greenup, R.A. et al. Time to surgery among women treated with neoadjuvant systemic therapy and upfront surgery for breast cancer. Breast Cancer Res Treat 186, 535–550 (2021). https://doi.org/10.1007/s10549-020-06012-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-06012-7