Abstract
Purpose
Family is often overlooked in cancer care. We developed a patient–family agenda setting intervention to engage family in cancer care communication.
Methods
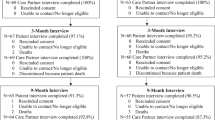
We conducted a pilot randomized controlled trial (NCT03283553) of patients on active treatment for breast cancer and their family “care partner.” Intervention dyads (n = 69) completed a self-administered checklist to clarify care partner roles, establish a shared visit agenda, and facilitate MyChart patient portal access. Control dyads (n = 63) received usual care. We assessed intervention acceptability and initial effects from post-visit surveys and MyChart utilization at 6 weeks.
Results
At baseline, most patients (89.4%) but few care partners (1.5%) were registered for MyChart. Most patients (79.4%) wanted their care partner to have access to their records and 39.4% of care partners reported accessing MyChart. In completing the checklist, patients and care partners endorsed active communication roles for the care partner and identified a similar visit agenda: most (> 90%) reported the checklist was easy, useful, and recommended it to others. At 6 weeks, intervention (vs control) care partners were more likely to be registered for MyChart (75.4% vs 1.6%; p < 0.001), to have logged in (43.5% vs 0%; p < 0.001) and viewed clinical notes (30.4% vs 0%; p < 0.001), but were no more likely to exchange direct messages with clinicians (1.5% vs 0%; p = 0.175). No differences in patients’ MyChart use were observed, but intervention patients more often viewed clinical notes (50.7% vs 9.5%; p < 0.001).
Conclusions
A patient–family agenda setting intervention was acceptable and affected online practices of cancer patients and care partners.



Similar content being viewed by others
Notes
MyChart ® is a registered trademark of Epic Systems Corporation.
References
Kent EE, Rowland JH, Northouse L et al (2016) Caring for caregivers and patients: research and clinical priorities for informal cancer caregiving. Cancer 122:1987–1995
Hobbs GS, Landrum MB, Arora NK et al (2015) The role of families in decisions regarding cancer treatments. Cancer 121:1079–1087
Laidsaar-Powell R, Butow P, Bu S et al (2016) Family involvement in cancer treatment decision-making: a qualitative study of patient, family, and clinician attitudes and experiences. Patient Educ Couns 99:1146–1155
Siminoff LA, Dorflinger L, Agyemang A et al (2012) Oncologists’ assessments of lung cancer patient and family disagreements regarding treatment decision making. Lung Cancer 77(1):212–216
Zhang AY, Zyzanski SJ, Siminoff LA (2010) Differential patient-caregiver opinions of treatment and care for advanced lung cancer patients. Soc Sci Med 70:1155–1158
NASEM (2016) Families caring for an aging America. National Academies Press, Washington, DC
Litzelman K, Kent EE, Mollica M et al (2016) How does caregiver well-being relate to perceived quality of care in patients with cancer? Exploring associations and pathways. J Clin Oncol 34:3554–3561
Hodges LJ, Humphris GM, Macfarlane G (2005) A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med 60:1–12
Wright AA, Zhang B, Ray A et al (2008) Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA J Am Med Assoc 300:1665–1673
Northouse LL, Katapodi MC, Song L et al (2010) Interventions with family caregivers of cancer patients: meta-analysis of randomized trials. CA Cancer J Clin 60:317–339
Griffin JM, Meis LA, Macdonald R et al (2014) Effectiveness of family and caregiver interventions on patient outcomes in adults with cancer: a systematic review. J Gen Intern Med 29:1274–1282
Delbanco T, Walker J, Bell SK et al (2012) Inviting patients to read their doctors’ notes: a quasi-experimental study and a look ahead. Ann Intern Med 157:461–470
Ricciardi L, Mostashari F, Murphy J et al (2013) A national action plan to support consumer engagement via e-health. Health Aff 32:376–384
Wolff JL, Kim V, Mintz S et al (2018) An environmental scan of shared access to the patient portal. J Am Med Inform Assoc JAMIA 25:408–412
Wolff JL, Darer JD, Berger A et al (2016) Inviting patients and care partners to read doctors’ notes: OpenNotes and shared access to electronic medical records. J Am Med Inform Assoc JAMIA 24:e116–e178
Wolff JL, Berger A, Clarke D et al (2016) Patients, care partners, and shared access to the patient portal: online practices at an integrated health system. J Am Med Inform Assoc JAMIA 23:1150–1158
Reed ME, Huang J, Brand R et al (2018) Communicating through a patient portal to engage family care partners. JAMA Intern Med 178:142–144
Mccleary NJ, Greenberg TL, Barysauskas CM et al (2018) Oncology patient portal enrollment at a comprehensive cancer center: a quality improvement initiative. J Oncol Pract 14:e451–e461
Wolff JL, Roter DL, Barron J et al (2014) A tool to strengthen the older patient-companion partnership in primary care: results from a pilot study. J Am Geriatr Soc 62:312–319
Wolff JL, Roter DL, Boyd CM et al (2018) Patient-family agenda setting for primary care patients with cognitive impairment: the SAME page trial. J Gen Intern Med 33:1478–1486
Gobat N, Kinnersley P, Gregory JW et al (2015) What is agenda setting in the clinical encounter? Consensus from literature review and expert consultation. Patient Educ Couns 98:822–829
Hawley ST, Li Y, An LC et al (2018) Improving breast cancer surgical treatment decision making: the iCanDecide randomized clinical trial. J Clin Oncol 36:659–666
Rodenbach RA, Brandes K, Fiscella K et al (2017) Promoting end-of-life discussions in advanced cancer: effects of patient coaching and question prompt lists. J Clin Oncol 35:842–851
Clayton JM, Butow PN, Tattersall MH et al (2007) Randomized controlled trial of a prompt list to help advanced cancer patients and their caregivers to ask questions about prognosis and end-of-life care. J Clin Oncol 25:715–723
Shin DW, Cho J, Roter DL et al (2017) Attitudes toward family involvement in cancer treatment decision making: the perspectives of patients, family caregivers, and their oncologists. Psycho-oncology 26:770–778
Wolff JL, Roter DL (2008) Hidden in plain sight: medical visit companions as a quality of care resource for vulnerable older adults. Arch Intern Med 168:1409–1415
Wolff JL, Roter DL (2011) Family presence in routine medical visits: a meta-analytical review. Soc Sci Med 72:823–831
Arroll B, Goodyear-Smith F, Crengle S et al (2010) Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med 8:348–353
Lowe B, Wahl I, Rose M et al (2010) A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord 122:86–95
Kroenke K, Spitzer RL, Williams JB et al (2007) Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med 146:317–325
Wallace LS, Rogers ES, Roskos SE et al (2006) Brief report: screening items to identify patients with limited health literacy skills. J Gen Intern Med 21:874–877
Brady MJ, Cella DF, Mo F et al (1997) Reliability and validity of the functional assessment of cancer therapy-breast quality-of-life instrument. J Clin Oncol 15:974–986
Wolff JL, Boyd CM (2015) A look at person-and family-centered care among older adults: results from a national survey. J Gen Intern Med 30:1497–1504
Yun YH, Lee MK, Park S et al (2011) Use of a decision aid to help caregivers discuss terminal disease status with a family member with cancer: a randomized controlled trial. J Clin Oncol 29:4811–4819
De Souza JA, Yap B, Ratain MJ et al (2015) User beware: we need more science and less art when measuring financial toxicity in oncology. J Clin Oncol 33:1414–1415
Khera N (2014) Reporting and grading financial toxicity. J Clin Oncol 32:3337–3338
Anthony DL, Campos-Castillo C, Lim PS (2018) Who isn’t using patient portals and why? Evidence and implications from a national sample of US adults. Health Aff 37:1948–1954
Epstein RM, Street RL Jr (2011) Shared mind: communication, decision making, and autonomy in serious illness. Ann Fam Med 9:454–461
IOM (2014) Dying in America: improving quality and honoring individual preferences near the end of life. National Academy Press, Washington DC
Bernacki RE, Block SD, For the American College of Physicians High Value Care Task F (2014) Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med 174(12):1994–2003
Mack JW, Cronin A, Taback N et al (2012) End-of-life care discussions among patients with advanced cancer: a cohort study. Ann Intern Med 156:204–210
Apatira L, Boyd EA, Malvar G et al (2008) Hope, truth, and preparing for death: perspectives of surrogate decision makers. Ann Intern Med 149:861–868
Vig E, Starks H, Taylor J et al (2007) Surviving surrogate decision-making: what helps and hampers the experience of making medical decisions for others. J Gen Intern Med 22:1274–1279
Cagle JG, Mcclymont KM, Thai JN et al (2016) “If you don’t know, all of a sudden, they’re gone”: caregiver perspectives about prognostic communication for disabled elderly adults. J Am Geriatr Soc 64:1299–1306
Mack JW, Cronin A, Keating NL et al (2012) Associations between end-of-life discussion characteristics and care received near death: a prospective cohort study. J Clin Oncol 30:4387–4395
Silveira MJ, Kim SY, Langa KM (2010) Advance directives and outcomes of surrogate decision making before death. N Engl J Med 362:1211–1218
Acknowledgements
The authors thank the following individuals without whom the study would not have been possible: Leena Aurora, Aamna Kabani, and Amy Guo for data collection; and the patients, care partners, and clinicians who participated in the study.
Funding
This study was supported by: Susan G. Komen Scholar Grant SAC170001 (ACW), 5R21AG049967 (JLW), P30CA006973, and P30AG048773. The sponsor of this research was not involved in study concept or design, recruitment of subjects, acquisition of data, data analysis or interpretation, or in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wolff, J.L., Aufill, J., Echavarria, D. et al. Sharing in care: engaging care partners in the care and communication of breast cancer patients. Breast Cancer Res Treat 177, 127–136 (2019). https://doi.org/10.1007/s10549-019-05306-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05306-9