Abstract
Purpose
Brain metastases from breast cancer are frequently managed with brain-directed radiation but the impact of subtype on intracranial recurrence patterns after radiation has not been well-described. We investigated intracranial recurrence patterns of brain metastases from breast cancer after brain-directed radiation to facilitate subtype-specific management paradigms.
Methods
We retrospectively analyzed 349 patients with newly diagnosed brain metastases from breast cancer treated with brain-directed radiation at Brigham and Women’s Hospital/Dana-Farber Cancer Institute between 2000 and 2015. Patients were stratified by subtype: hormone receptor-positive/human epidermal growth factor receptor 2-negative (HR+/HER2−), HER2+ positive (HER2+), or triple-negative breast cancer (TNBC). A per-metastasis assessment was conducted. Time-to-event analyses were conducted using multivariable Cox regression.
Results
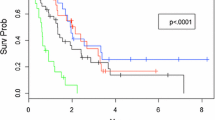
Of the 349 patients, 116 had HR+/HER2− subtype, 164 had HER2+ subtype, and 69 harbored TNBC. Relative to HR+/HER2− subtype, local recurrence was greater in HER2+ metastases (HR 3.20, 95% CI 1.78–5.75, p < 0.001), while patients with TNBC demonstrated higher rates of new brain metastases after initial treatment (HR 3.16, 95% CI 1.99–5.02, p < 0.001) and shorter time to salvage whole brain radiation (WBRT) (HR 3.79, 95% CI 1.36–10.56, p = 0.01) and salvage stereotactic radiation (HR 1.86, 95% CI 1.11–3.10, p = 0.02).
Conclusions
We identified a strong association between breast cancer subtype and intracranial recurrence patterns after brain-directed radiation, particularly local progression for HER2+ and distant progression for TNBC patients. If validated, the poorer local control in HER2+ brain metastases may support evaluation of novel local therapy-based approaches, while the increased distant recurrence in TNBC suggests the need for improved systemic therapy and earlier utilization of WBRT.


Similar content being viewed by others
References
Cagney DN, Martin AM, Catalano PJ et al (2018) Implications of screening for brain metastases in patients with breast cancer and non-small cell lung cancer. JAMA Oncol 4:1001. https://doi.org/10.1001/jamaoncol.2018.0813
Vuong DA, Rades D, Vo SQ, Busse R (2011) Extracranial metastatic patterns on occurrence of brain metastases. J Neurooncol 105:83–90. https://doi.org/10.1007/s11060-011-0563-z
Nayak L, Lee EQ, Wen PY (2012) Epidemiology of brain metastases. Curr Oncol Rep 14:48–54. https://doi.org/10.1007/s11912-011-0203-y
Leyland-Jones B (2009) Human epidermal growth factor receptor 2-positive breast cancer and central nervous system metastases. J Clin Oncol 27:5278–5286. https://doi.org/10.1200/JCO.2008.19.8481
Lin NU, Claus E, Sohl J et al (2008) Sites of distant recurrence and clinical outcomes in patients with metastatic triple-negative breast cancer: high incidence of central nervous system metastases. Cancer 113:2638–2645. https://doi.org/10.1002/cncr.23930
Sanna G, Franceschelli L, Rotmensz N et al (2007) Brain metastases in patients with advanced breast cancer. Anticancer Res 27:2865–2869
Sperduto PW, Kased N, Roberge D et al (2013) The effect of tumor subtype on the time from primary diagnosis to development of brain metastases and survival in patients with breast cancer. J Neurooncol 112:467–472. https://doi.org/10.1007/s11060-013-1083-9
Martin AM, Cagney DN, Catalano PJ et al (2017) Brain metastases in newly diagnosed breast cancer: a population-based study. JAMA Oncol 3:1069–1077. https://doi.org/10.1001/jamaoncol.2017.0001
Corona SP, Sobhani N, Ianza A et al (2017) Advances in systemic therapy for metastatic breast cancer: future perspectives. Med Oncol 34:119. https://doi.org/10.1007/s12032-017-0975-5
Muldoon LL, Soussain C, Jahnke K et al (2007) Chemotherapy delivery issues in central nervous system malignancy: a reality check. J Clin Oncol 25:2295–2305. https://doi.org/10.1200/JCO.2006.09.9861
Lin NU, Winer EP (2007) Brain metastases: the HER2 paradigm. Clin Cancer Res 13:1648–1655. https://doi.org/10.1158/1078-0432.CCR-06-2478
Cameron D, Piccart-Gebhart MJ, Gelber RD et al (2017) 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin Adjuvant (HERA) trial. Lancet 389:1195–1205. https://doi.org/10.1016/S0140-6736(16)32616-2
Witzel I, Oliveira-Ferrer L, Pantel K et al (2016) Breast cancer brain metastases: biology and new clinical perspectives. Breast Cancer Res 18:8. https://doi.org/10.1186/s13058-015-0665-1
Brown PD, Ballman KV, Cerhan JH et al (2017) Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC.3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol 18:1049–1060. https://doi.org/10.1016/S1470-2045(17)30441-2
Aoyama H (2011) Radiation therapy for brain metastases in breast cancer patients. Breast Cancer 18:244–251. https://doi.org/10.1007/s12282-010-0207-8
Brown PD, Jaeckle K, Ballman KV et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316:401–409. https://doi.org/10.1001/jama.2016.9839
Hall WA, Djalilian HR, Nussbaum ES, Cho KH (2000) Long-term survival with metastatic cancer to the brain. Med Oncol 17:279–286
Niikura N, Hayashi N, Masuda N et al (2014) Treatment outcomes and prognostic factors for patients with brain metastases from breast cancer of each subtype: a multicenter retrospective analysis. Breast Cancer Res Treat 147:103–112. https://doi.org/10.1007/s10549-014-3090-8
Jin J, Gao Y, Zhang J et al (2018) Incidence, pattern and prognosis of brain metastases in patients with metastatic triple negative breast cancer. BMC Cancer 18:446. https://doi.org/10.1186/s12885-018-4371-0
Darlix A, Griguolo G, Thezenas S et al (2018) Hormone receptors status: a strong determinant of the kinetics of brain metastases occurrence compared with HER2 status in breast cancer. J Neurooncol 138:369–382. https://doi.org/10.1007/s11060-018-2805-9
Kuba S, Ishida M, Nakamura Y et al (2014) Treatment and prognosis of breast cancer patients with brain metastases according to intrinsic subtype. Jpn J Clin Oncol 44:1025–1031. https://doi.org/10.1093/jjco/hyu126
Chong JU, Ahn SG, Lee HM et al (2015) Local control of brain metastasis: treatment outcome of focal brain treatments in relation to subtypes. J Breast Cancer 18:29–35. https://doi.org/10.4048/jbc.2015.18.1.29
Fokas E, Henzel M, Hamm K et al (2012) Brain metastases in breast cancer: analysis of the role of HER2 status and treatment in the outcome of 94 patients. Tumori 98:768–774. https://doi.org/10.1700/1217.13502
Hines SL, Vallow LA, Tan WW et al (2008) Clinical outcomes after a diagnosis of brain metastases in patients with estrogen- and/or human epidermal growth factor receptor 2-positive versus triple-negative breast cancer. Ann Oncol 19:1561–1565. https://doi.org/10.1093/annonc/mdn283
Kress MA, Oermann E, Ewend MG et al (2013) Stereotactic radiosurgery for single brain metastases from non-small cell lung cancer: progression of extracranial disease correlates with distant intracranial failure. Radiat Oncol 8:64. https://doi.org/10.1186/1748-717X-8-64
Brown PD, Jaeckle K, Ballman KV et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases a randomized clinical trial. JAMA 316(4):401–409. https://doi.org/10.1001/jama.2016.9839
Cagney DN, Martin AM, Catalano PJ et al (2018) Impact of pemetrexed on intracranial disease control and radiation necrosis in patients with brain metastases from non-small cell lung cancer receiving stereotactic radiation. Radiother Oncol 126:511–518. https://doi.org/10.1016/j.radonc.2018.01.005
Vern-Gross TZ, Lawrence JA, Case LD et al (2012) Breast cancer subtype affects patterns of failure of brain metastases after treatment with stereotactic radiosurgery. J Neurooncol 110:381–388. https://doi.org/10.1007/s11060-012-0976-3
Grubb CS, Jani A, Wu CC et al (2016) Breast cancer subtype as a predictor for outcomes and control in the setting of brain metastases treated with stereotactic radiosurgery. J Neurooncol 127:103–110. https://doi.org/10.1007/s11060-015-2014-8
Schuttrumpf LH, Niyazi M, Nachbichler SB et al (2014) Prognostic factors for survival and radiation necrosis after stereotactic radiosurgery alone or in combination with whole brain radiation therapy for 1-3 cerebral metastases. Radiat Oncol 9:105. https://doi.org/10.1186/1748-717X-9-105
Abraham C, Garsa A, Badiyan SN et al (2018) Internal dose escalation is associated with increased local control for non-small cell lung cancer (NSCLC) brain metastases treated with stereotactic radiosurgery (SRS). Adv Radiat Oncol 3:146–153. https://doi.org/10.1016/j.adro.2017.11.003
Lux F, Tran VL, Thomas E et al (2018) AGuIX((R)) from bench to bedside-Transfer of an ultrasmall theranostic gadolinium-based nanoparticle to clinical medicine. Br J Radiol 92(1093):20180365. https://doi.org/10.1259/bjr.20180365
Kwon HC, Oh SY, Kim SH et al (2010) Clinical outcomes and breast cancer subtypes in patients with brain metastases. Onkologie 33:146–152. https://doi.org/10.1159/000286281
Schmid P, Adams S, Rugo HS et al (2018) Atezolizumab and Nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med 379:2108–2121. https://doi.org/10.1056/NEJMoa1809615
Gondi V, Deshmukh S, Brown PD et al (2018) Preservation of neurocognitive function (NCF) with conformal avoidance of the hippocampus during whole-brain radiotherapy (HA-WBRT) for brain metastases: preliminary results of phase III trial NRG Oncology CC001. Int J Radiat Oncol Biol Phys 102:1607. https://doi.org/10.1016/j.ijrobp.2018.08.056
Priedigkeit N, Hartmaier RJ, Chen Y et al (2017) Intrinsic subtype switching and acquired ERBB2/HER2 amplifications and mutations in breast cancer brain metastases. JAMA Oncol 3:666. https://doi.org/10.1001/jamaoncol.2016.5630
Thomson AH, McGrane J, Mathew J et al (2016) Changing molecular profile of brain metastases compared with matched breast primary cancers and impact on clinical outcomes. Br J Cancer 114:793–800. https://doi.org/10.1038/bjc.2016.34
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Daniel N. Cagney is a recipient of research support from NH Theraguix. Paul Brown reports personal fees from UpToDate (current) and personal fees as DSMB member Novella Clinical (2016) outside the submitted work. Dr. Leone reports that the institution (University of Iowa) received research funding from Merck. Dr. Leone reports funding from Kazia, Lilly, and Seattle Genetics. Daphne A. Haas-Kogan is advisory board member for Cellworks and reports clinical trial support from Novartis. Dr. Lin reports research grants from Pfizer, Genentech/Roche, Novartis, Seattle Genetics, and consulting fees from Pfizer, Genentech/Roche, Novartis, Seattle Genetics, Daichii, and Puma. Dr Alexander reports personal fees from Foundation Medicine, AbbVie, Schlesinger Associates, Bristol Myers Squibb, Precision Health Economics; grants from Puma, Celgene, Eli Lilly outside the submitted work. Dr. Aizer reports research funding from Varian Medical Systems and consulting fees from Novartis. The remaining authors declare no conflict of interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cagney, D.N., Lamba, N., Montoya, S. et al. Breast cancer subtype and intracranial recurrence patterns after brain-directed radiation for brain metastases. Breast Cancer Res Treat 176, 171–179 (2019). https://doi.org/10.1007/s10549-019-05236-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05236-6