Abstract
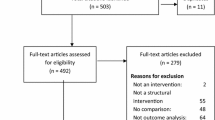
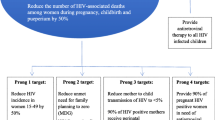
HIV remains a threat to global public health, disproportionately affecting countries across Sub-Saharan Africa. Although treatment and access to care have improved, prevention remains critical to ending new HIV infections by 2030. A variety of prevention strategies exist, yet their effectiveness is difficult to measure and variable due to the nature of the interventions and vulnerability of the intervention during implementation. This systematic review of 51 studies synthesizes data on the implementation and evaluation of evidence-based HIV prevention interventions across Sub-Saharan Africa. Studies were included if they occurred between January 1, 2008, and December 31, 2019, inclusive in Sub-Saharan Africa, were written in English, implemented an HIV prevention intervention in the field, and had reportable results. Using a modified social-ecological model for HIV prevention, we divided studies into three categories: interventions targeting health systems (n = 16), communities (n = 8), and individuals (n = 27). Across all categories, the data emphasized preventing mother-to-child transmission (PMTCT), medical interventions, and psychosocial interventions. The most successful programs bundled several interventions that were integrated into the health system. There is a notable lack of interventions targeting key populations and there are significant rates of loss to follow up (LTFU) across many studies. This review provides insight into the prioritization of evidence-based HIV prevention interventions across Sub-Saharan Africa.



Similar content being viewed by others
Data Availability
Data are fully available without restriction. No primary data were collected as part of this manuscript. The reviewed data are available in all references cited.
Code Availability
Not applicable.
References
November 25 CSH govDate last updated:. 2020. Global Statistics [Internet]. HIV.gov. 2020 [cited 2021 Feb 22]. Available from: https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics.
Africa NRC (US) P on D and RP for AA in S-S, Cohen B, Trussell J. Primary HIV-Prevention Strategies [Internet]. Prev. Mitigating AIDS Sub-Sahar. Afr. Res. Data Priorities Soc. Behav. Sci. National Academies Press (US); 1996 [cited 2021 Feb 25]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK232826/.
Beyrer C. Consolidated Guidelines on Hiv Prevention, Diagnosis, Treatment and Care for Key Populations [Internet]. Place of publication not identified: World Health Organization; 2016 [cited 2021 Feb 22]. Available from: http://proxy.library.carleton.ca/loginurl=https://www.deslibris.ca/ID/10063272.
UNAIDS. Prevention gap report [Internet]. 2016 [cited 2021 Feb 25]. Available from: https://www.unaids.org/en/resources/documents/2016/prevention-gap.
February 24 CSH govDate last updated:. 2020. HIV Treatment as Prevention [Internet]. HIV.gov. 2020 [cited 2021 Feb 25]. Available from: https://www.hiv.gov/tasp.
Magnus M, Castel A. Breaking Down the Siloes: Developing Effective Multidisciplinary HIV Research Teams. AIDS Behav. 2016;20:273–80.
Torrone EA, Levandowski BA, Thomas JC, Isler MR, Leone PA. Identifying gaps in HIV prevention services. Soc Work Public Health. 2010;25:327–40.
Kharsany ABM, Karim QA. HIV Infection and AIDS in Sub-Saharan Africa: Current Status, Challenges and Opportunities. Open AIDS J. 2016;10:34–48.
HIV and AIDS in East and Southern Africa regional overview [Internet]. Avert. 2019 [cited 2021 Oct 18]. Available from: https://www.avert.org/professionals/hiv-around-world/sub-saharan-africa/overview.
Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482.
Mansoor LE, Yende-Zuma N, Baxter C, Mngadi KT, Dawood H, Gengiah TN, et al. Integrated provision of topical pre-exposure prophylaxis in routine family planning services in South Africa: a non-inferiority randomized controlled trial. J Int AIDS Soc. 2019;22:e25381.
Bisio F, Masini G, Blasi Vacca E, Calzi A, Cardinale F, Bruzzone B, et al. Effectiveness of a project to prevent HIV vertical transmission in the Republic of Congo. J Antimicrob Chemother. 2013;68:1862–71.
Amico KR, Mansoor LE, Corneli A, Torjesen K, van der Straten A. Adherence Support Approaches in Biomedical HIV Prevention Trials: Experiences, Insights and Future Directions from Four Multisite Prevention Trials. AIDS Behav. 2013;17:2143–55.
Baeten JM, Heffron R, Kidoguchi L, Mugo NR, Katabira E, Bukusi EA, et al. Integrated Delivery of Antiretroviral Treatment and Pre-exposure Prophylaxis to HIV-1-Serodiscordant Couples: A Prospective Implementation Study in Kenya and Uganda. PLoS Med. 2016;13:e1002099.
Eakle R, Gomez GB, Naicker N, Bothma R, Mbogua J, Escobar MAC, et al. HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: Results from a prospective observational demonstration project. PLOS Med Public Library of Science. 2017;14:e1002444.
Haberer JE, Baeten JM, Campbell J, Wangisi J, Katabira E, Ronald A, et al. Adherence to Antiretroviral Prophylaxis for HIV Prevention: A Substudy Cohort within a Clinical Trial of Serodiscordant Couples in East Africa. PLoS Med [Internet]. 2013 [cited 2020 May 24];10. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3769210/.
Psaros C, Haberer JE, Katabira E, Ronald A, Tumwesigye E, Campbell JD, et al. An intervention to support HIV pre-exposure prophylaxis (PrEP) adherence in HIV serodiscordant couples in Uganda. J Acquir Immune Defic Syndr 1999. 2014;66:522–9.
Wynne J, Muwawu R, Mubiru MC, Kamira B, Kemigisha D, Nakyanzi T, et al. Maximizing participant retention in a phase 2B HIV prevention trial in Kampala, Uganda: The MTN-003 (VOICE) Study. HIV Clin Trials. 2018;19:165–71.
Odeny TA, Bailey RC, Bukusi EA, Simoni JM, Tapia KA, Yuhas K, et al. Text messaging to improve attendance at post-operative clinic visits after adult male circumcision for HIV prevention: a randomized controlled trial. PLoS ONE. 2012;7:e43832.
Abrahams N, Jewkes R, Lombard C, Mathews S, Campbell J, Meel B. Impact of telephonic psycho-social support on adherence to post-exposure prophylaxis (PEP) after rape. AIDS Care Taylor & Francis. 2010;22:1173–81.
Hayes RJ, Donnell D, Floyd S, Mandla N, Bwalya J, Sabapathy K, et al. Impact of a universal testing and treatment intervention on HIV incidence in Zambia and South Africa: results of the HPTN 071 (PopART) community-randomized trial. N Engl J Med. 2019;381:207–18.
Stephenson R, Vwalika B, Greenberg L, Ahmed Y, Vwalika C, Chomba E, et al. A randomized controlled trial to promote long-term contraceptive use among HIV-serodiscordant and concordant positive couples in Zambia. J Womens Health 2002. 2011;20:567–74.
Ahoua L, Tiendrebeogo T, Arikawa S, Lahuerta M, Aly D, Journot V, et al. PMTCT care cascade and factors associated with attrition in the first four years after Option B + implementation in Mozambique. Trop Med Int Health TM IH. 2020;25:222–35.
Bhardwaj S, Barron P, Pillay Y, Treger-Slavin L, Robinson P, Goga A, et al. Elimination of mother-to-child transmission of HIV in South Africa: rapid scale-up using quality improvement. South Afr Med J Suid-Afr Tydskr Vir Geneeskd. 2014;104:239–43.
Edmonds A, Feinstein L, Okitolonda V, Thompson D, Kawende B, Behets F. Decentralization Does Not Assure Optimal Delivery of PMTCT and HIV-Exposed Infant Services in a Low Prevalence Setting. J Acquir Immune Defic Syndr 1999. 2015;70:e130–9.
Gamell A, Glass TR, Luwanda LB, Mapesi H, Samson L, Mtoi T, et al. Implementation and Operational Research: An Integrated and Comprehensive Service Delivery Model to Improve Pediatric and Maternal HIV Care in Rural Africa. J Acquir Immune Defic Syndr 1999. 2016;73:e67–75.
Horwood C, Haskins L, Vermaak K, Phakathi S, Subbaye R, Doherty T. Prevention of mother to child transmission of HIV (PMTCT) programme in KwaZulu-Natal, South Africa: an evaluation of PMTCT implementation and integration into routine maternal, child and women’s health services. Trop Med Int Health TM IH. 2010;15:992–9.
Malaju MT, Alene GD. Assessment of utilization of provider-initiated HIV testing and counseling as an intervention for prevention of mother to child transmission of HIV and associated factors among pregnant women in Gondar town, North West Ethiopia. BMC Public Health. 2012;12:226.
Mandala J, Kasonde P, Badru T, Dirks R, Torpey K. HIV Retesting of HIV-Negative Pregnant Women in the Context of Prevention of Mother-to-Child Transmission of HIV in Primary Health Centers in Rural Zambia: What Did We Learn? J Int Assoc Provid AIDS Care. 2019;18:2325958218823530.
Moses A, Zimba C, Kamanga E, Nkhoma J, Maida A, Martinson F, et al. Prevention of mother-to-child transmission: program changes and the effect on uptake of the HIVNET 012 regimen in Malawi. AIDS Lond Engl. 2008;22:83–7.
Penda CI, Tejiokem MC, Sofeu CL, Ndiang ST, Ateba Ndongo F, Kfutwah A, et al. Low rate of early vertical transmission of HIV supports the feasibility of effective implementation of the national PMTCT guidelines in routine practice of referral hospitals in Cameroon. Paediatr Int Child Health. 2019;39:208–15.
Agarwal S, Lasway C, L’Engle K, Homan R, Layer E, Ollis S, et al. Family Planning Counseling in Your Pocket: A Mobile Job Aid for Community Health Workers in Tanzania. Glob Health Sci Pract. 2016;4:300–10.
Bachanas P, Kidder D, Medley A, Pals SL, Carpenter D, Howard A, et al. Delivering Prevention Interventions to People Living with HIV in Clinical Care Settings: Results of a Cluster Randomized Trial in Kenya, Namibia, and Tanzania. AIDS Behav. 2016;20:2110–8.
Fatti G, Shaikh N, Jackson D, Goga A, Nachega JB, Eley B, et al. Low HIV incidence in pregnant and postpartum women receiving a community-based combination HIV prevention intervention in a high HIV incidence setting in South Africa. PLoS ONE. 2017;12:e0181691.
Futterman D, Shea J, Besser M, Stafford S, Desmond K, Comulada WS, et al. Mamekhaya: a pilot study combining a cognitive-behavioral intervention and mentor mothers with PMTCT services in South Africa. AIDS Care. 2010;22:1093–100.
Hamela G, Kabondo C, Tembo T, Zimba C, Kamanga E, Mofolo I, et al. Evaluating the benefits of incorporating traditional birth attendants in HIV prevention of mother to child transmission service delivery in Lilongwe, Malawi. Afr J Reprod Health. 2014;18:27–34.
Napierala S, Kang M-S, Chipato T, Padian N, van der Straten A. Female Condom Uptake and Acceptability in Zimbabwe. AIDS Educ Prev. 2008;20:121–34.
Jones D, Weiss SM, Arheart K, Cook R, Chitalu N. Implementation of HIV Prevention Interventions in Resource Limited Settings: The Partner Project. J Community Health. 2014;39:151–8.
Karamagi E, Sensalire S, Nabwire J, Byabagambi J, Awio AO, Aluma G, et al. Quality improvement as a framework for behavior change interventions in HIV-predisposed communities: a case of adolescent girls and young women in northern Uganda. AIDS Res Ther. 2018;15:4.
Kalichman SC, Cain D, Eaton L, Jooste S, Simbayi LC. Randomized Clinical Trial of Brief Risk Reduction Counseling for Sexually Transmitted Infection Clinic Patients in Cape Town, South Africa. Am J Public Health American Public Health Association. 2011;101:e9–17.
Maman S, Moodley D, McNaughton-Reyes HL, Groves AK, Kagee A, Moodley P. Efficacy of Enhanced HIV Counseling for Risk Reduction during Pregnancy and in the Postpartum Period: A Randomized Controlled Trial. PLOS ONE Public Library of Science. 2014;9:e97092.
Miller WC, Rutstein SE, Phiri S, Kamanga G, Nsona D, Pasquale DK, et al. Randomized Controlled Pilot Study of Antiretrovirals and a Behavioral Intervention for Persons With Acute HIV Infection: Opportunity for Interrupting Transmission. Open Forum Infect Dis. 2019;6:ofy341.
Herlihy JM, Hamomba L, Bonawitz R, Goggin CE, Sambambi K, Mwale J, et al. Integration of PMTCT and Antenatal Services Improves Combination Antiretroviral Therapy Uptake for HIV-Positive Pregnant Women in Southern Zambia: A Prototype for Option B+? J Acquir Immune Defic Syndr 1999. 2015;70:e123–9.
Fayorsey RN, Chege D, Wang C, Reidy W, Peters Z, Syengo M, et al. Mother Infant Retention for Health (MIR4Health): Study Design, Adaptations, and Challenges With PMTCT Implementation Science Research. J Acquir Immune Defic Syndr 1999. 2016;72 Suppl 2:S137-144.
Yotebieng M, Moracco KE, Thirumurthy H, Edmonds A, Tabala M, Kawende B, et al. Conditional cash transfers improve retention in PMTCT services by mitigating the negative effect of not having money to come to the clinic. J Acquir Immune Defic Syndr 1999. 2017;74:150–7.
Yotebieng M, Thirumurthy H, Moracco KE, Edmonds A, Tabala M, Kawende B, et al. Conditional Cash Transfers to Increase Retention in PMTCT Care, Antiretroviral Adherence, and Postpartum Virological Suppression: A Randomized Controlled Trial. J Acquir Immune Defic Syndr 1999. 2016;72:S124–9.
Yotebieng M, Thirumurthy H, Moracco KE, Kawende B, Chalachala JL, Wenzi LK, et al. Conditional cash transfers increase uptake of and retention in PMTCT care: A randomized controlled trial. Lancet HIV. 2016;3:e85–93.
Kassaye SG, Ong’ech J, Sirengo M, Kose J, Matu L, McOdida P, et al. Cluster-Randomized Controlled Study of SMS Text Messages for Prevention of Mother-to-Child Transmission of HIV in Rural Kenya. AIDS Res Treat. 2016;2016:1289328.
Peltzer K, Weiss SM, Soni M, Lee TK, Rodriguez VJ, Cook R, et al. A cluster randomized controlled trial of lay health worker support for prevention of mother to child transmission of HIV (PMTCT) in South Africa. AIDS Res Ther [Internet]. 2017 [cited 2021 Feb 28];14. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5732507/.
Phiri S, Tweya H, van Lettow M, Rosenberg NE, Trapence C, Kapito-Tembo A, et al. Impact of Facility- and Community-Based Peer Support Models on Maternal Uptake and Retention in Malawi’s Option B + HIV Prevention of Mother-to-Child Transmission Program: A 3-Arm Cluster Randomized Controlled Trial (PURE Malawi). J Acquir Immune Defic Syndr 1999. 2017;75 Suppl 2:S140–8.
Richter L, Rotheram-Borus MJ, Van Heerden A, Stein A, Tomlinson M, Harwood JM, et al. Pregnant women living with HIV (WLH) supported at clinics by peer WLH: a cluster randomized controlled trial. AIDS Behav. 2014;18:706–15.
Konate I, Traore L, Ouedraogo A, Sanon A, Diallo R, Ouedraogo J-L, et al. Linking HIV Prevention and Care for Community Interventions Among High-Risk Women in Burkina Faso—The ARNS 1222 “Yerelon” Cohort. JAIDS J Acquir Immune Defic Syndr. 2011;57:50.
Akama E, Mburu M, Mutegi E, Nyanaro G, Otieno JP, Ndolo S, et al. Impact of a Rapid Results Initiative Approach on Improving Male Partner Involvement in Prevention of Mother to Child Transmission of HIV in Western Kenya. AIDS Behav. 2018;22:2956–65.
Kanyuuru L, Kabue M, Ashengo TA, Ruparelia C, Mokaya E, Malonza I. RED for PMTCT: an adaptation of immunization’s Reaching Every District approach increases coverage, access, and utilization of PMTCT care in Bondo District, Kenya. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 2015;130(Suppl 2):68–73.
Nsubuga-Nyombi T, Karamagi E, Nabitaka L, Namukose S, Calnan J, Nyakwezi S, et al. Increasing HIV-Free Survival of Infants: Reorganizing Care Using Quality Improvement for the Optimal Health and Nutrition of HIV-Positive Women and Their Exposed Infants in Uganda. J Int Assoc Provid AIDS Care. 2019;18:2325958219857724.
Phaswana-Mafuya N, Peltzer K, Ladzani R, Mlambo G, Davids A, Phaweni K, et al. Pre- and post-intervention assessment of a PMTCT-programme-strengthening initiative in a rural area of the Eastern Cape, South Africa. Afr J AIDS Res AJAR. 2011;10:83–93.
Nyondo AL, Choko AT, Chimwaza AF, Muula AS. Invitation Cards during Pregnancy Enhance Male Partner Involvement in Prevention of Mother to Child Transmission (PMTCT) of Human Immunodeficiency Virus (HIV) in Blantyre, Malawi: A Randomized Controlled Open Label Trial. 10: PLOS ONE. Public Library of Science; 2015. p. e0119273.
Sifunda S, Peltzer K, Rodriguez VJ, Mandell LN, Lee TK, Ramlagan S, et al. Impact of male partner involvement on mother-to-child transmission of HIV and HIV-free survival among HIV-exposed infants in rural South Africa: Results from a two phase randomised controlled trial. PLoS ONE. 2019;14:e0217467.
Corneli A, Pettifor A, Kamanga G, Golin C, McKenna K, Ou S-S, et al. HPTN 062: A feasibility and acceptability pilot intervention to reduce HIV transmission risk behaviors among individuals with acute and early HIV infection in Lilongwe, Malawi. AIDS Behav. 2014;18:1785–800.
Jani N, Vu L, Kay L, Habtamu K, Kalibala S. Reducing HIV-related risk and mental health problems through a client-centred psychosocial intervention for vulnerable adolescents in Addis Ababa, Ethiopia. J Int AIDS Soc. 2016;19:20832.
Rosenberg NE, Bhushan NL, Vansia D, Phanga T, Maseko B, Nthani T, et al. Comparing Youth-Friendly Health Services to the Standard of Care Through “Girl Power-Malawi”: A Quasi-Experimental Cohort Study. J Acquir Immune Defic Syndr 1999. 2018;79:458–66.
ELOPRE L, KUDROFF K, WESTFALL AO, OVERTON ET, MUGAVERO MJ. The Right People, Right Places, and Right Practices: Disparities in PrEP access among African American Men, Women and MSM in the Deep South. J Acquir Immune Defic Syndr 1999. 2017;74:56–9.
Kroon EDMB, Phanuphak N, Shattock AJ, Fletcher JLK, Pinyakorn S, Chomchey N, et al. Acute HIV infection detection and immediate treatment estimated to reduce transmission by 89% among men who have sex with men in Bangkok. J Int AIDS Soc. 2017;20:21708.
Söderlund N, Lavis J, Broomberg J, Mills A. The costs of HIV prevention strategies in developing countries. Bull World Health Organ. 1993;71:595–604.
Funding
The authors are grateful for the support of the National Institute of Mental Health (Award Number R01 MH110358) and the National Institute of Nursing Research of the National Institutes of Health (NIH) (Award Number R01 NR016650).
Author information
Authors and Affiliations
Contributions
BH, SB and GT conceived the study; CL, GT, BH, EH, and SR developed the initial search strategy and completed the initial search, SFR, ADP, NV, and BH completed data abstraction for the selected articles and updated the search; SFR, ADP, and BH contributed to the synthesis of the results and the writing of the manuscript; all authors reviewed, edited and approved of the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethics approval
Not applicable.
Informed consent
This study is a systematic review of the peer-reviewed published literature so informed consent was not needed as no patient level were included in this study.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
Appendix 1: Overview of search strategies. (Supplementary material 2).
Appendix 2: Appendix of all HIV prevention articles included in this review. (Supplementary material 3).
Rights and permissions
About this article
Cite this article
Rapaport, S.F., Peer, A.D., Viswasam, N. et al. Implementing HIV Prevention in Sub-Saharan Africa: A Systematic Review of Interventions Targeting Systems, Communities, and Individuals. AIDS Behav 27, 150–160 (2023). https://doi.org/10.1007/s10461-022-03751-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03751-0