Abstract
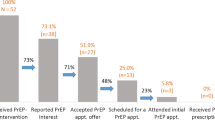
Pre-exposure prophylaxis (PrEP) uptake among women in the United States has been low. To increase uptake, we developed a peer outreach and navigation PrEP intervention. Semi-structured qualitative interviews with 32 cisgender women and 3 transgender women were conducted to assess the intervention. We used a thematic approach to identify barriers to, and facilitators of the intervention. Facilitators included interest in PrEP, offer of health and social services, the intervention’s women-focused approach, and peer outreach and navigation. Barriers were perceived HIV risk, concerns about medication side effects or interactions, housing insecurity and travel, co-occurring health-related conditions, and caregiving responsibilities. We recommend that future interventions consider packaging PrEP in local community settings, such as syringe exchange programs; include services such as food and housing assistance; use peers to recruit and educate women; integrate a culturally appropriate women’s focus; and consider providing same-day PrEP.
Similar content being viewed by others
References
Kral AH, Bluthenthal RN, Lorvick J, Gee L, Bacchetti P, Edlin BR. Sexual transmission of HIV-1 among injection drug users in San Francisco, USA: risk-factor analysis. Lancet. 2001;357(9266):1397–401.
Rondinelli AJ, Ouellet LJ, Strathdee SA, Latka MH, Hudson SM, Hagan H, et al. Young adult injection drug users in the United States continue to practice HIV risk behaviors. Drug Alcohol Depend. 2009;104(1–2):167–74.
Jenness SM, Kobrak P, Wendel T, Neaigus A, Murrill CS, Hagan H. Patterns of exchange sex and HIV infection in high-risk heterosexual men and women. Save Reference. 2011;88(2):329–41.
Blouin K, Leclerc P, Morissette C, Roy E, Blanchette C, Parent R, et al. Sex work as an emerging risk factor for human immunodeficiency virus seroconversion among people who inject drugs in the SurvUDI network. Sex Transm Dis. 2016;43(10):648–55.
Lemert EM. Social pathology: a systematic approach to the theory of sociopathic behavior. New York: McGraw-Hill; 1951.
Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17.
Walters SM, Reilly KH, Neaigus A, Braunstein S. Awareness of pre-exposure prophylaxis (PrEP) among women who inject drugs in NYC: the importance of networks and syringe exchange programs for HIV prevention. Harm Reduct J. 2017;14(1):40.
Peters PJ, Pontones P, Hoover KW, Patel MR, Galang RR, Shields J, et al. HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N Engl J Med. 2016;375(3):229–39.
Cranston K, Alpren C, John B, Dawson E, Roosevelt K, Burrage A, et al. Notes from the field: HIV diagnoses among persons who inject drugs—Northeastern Massachusetts, 2015–2018. Morb Mortal Wkly Rep. 2019;68(10):253.
Golden MR, Lechtenberg R, Glick SN, Dombrowski J, Duchin J, Reuer JR, et al. Outbreak of human immunodeficiency virus infection among heterosexual persons who are living homeless and inject drugs—Seattle, Washington, 2018. Morb Mortal Wkly Rep. 2019;68(15):344.
Walters SM, Rivera AV, Reilly KH, Anderson BJ, Bolden B, Wogayehu A, et al. Exchange sex among persons who inject drugs in the New York metropolitan area: the importance of local context, gender and sexual identity. AIDS Behav. 2018;1:1–15.
Kalichman SC, Williams EA, Cherry C, Belcher L, Nachimson D. Sexual coercion, domestic violence, and negotiating condom use among low-income African American women. J Womens Health. 1998;7(3):371–8.
Pyett PM, Warr DJ. Vulnerability on the streets: female sex workers and HIV risk. AIDS Care. 1997;9(5):539–47.
Nemoto T, Operario D, Keatley J, Villegas D. Social context of HIV risk behaviours among male-to-female transgenders of colour. AIDS Care. 2004;16(6):724–35.
Pulerwitz J, Amaro H, Jong WD, Gortmaker SL, Rudd R. Relationship power, condom use and HIV risk among women in the USA. AIDS Care. 2002;14(6):789–800.
Bennett GA, Velleman RD, Barter G, Bradbury C. Gender differences in sharing injecting equipment by drug users in England. AIDS Care. 2000;12(1):77–87.
Evans JL, Hahn JA, Page-Shafer K, Lum PJ, Stein ES, Davidson PJ, et al. Gender differences in sexual and injection risk behavior among active young injection drug users in San Francisco (the UFO Study). J Urban Health. 2003;80(1):137–46.
Kurtz SP, Surratt HL, Kiley MC, Inciardi JA. Barriers to health and social services for street-based sex workers. J Health Care Poor Underserv. 2005;16(2):345–61.
Jaiswal J, Dunlap K, Griffin M, Cox A, Singer S, Hascher K, et al. Pre-exposure prophylaxis awareness, acceptability and potential stigma among medical and non-medical clinic staff in methadone treatment settings in northern New Jersey: the key role of non-medical staff in enhancing HIV prevention. J Substance Abuse Treat. 2021;129:108371.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34.
Deutsch MB, Glidden DV, Sevelius J, Keatley J, McMahan V, Guanira J, et al. HIV pre-exposure prophylaxis in transgender women: a subgroup analysis of the iPrEx trial. Lancet HIV. 2015;2(12):e512–9.
Thomson KA, Baeten JM, Mugo NR, Bekker L-G, Celum CL, Heffron R. Tenofovir-based oral preexposure prophylaxis prevents HIV infection among women. Curr Opin HIV AIDS. 2016;11(1):18–26.
Tomko C, Park JN, Allen ST, Glick J, Galai N, Decker MR, et al. Awareness and interest in HIV pre-exposure prophylaxis among street-based female sex workers: results from a US context. AIDS Patient Care STDs. 2019;33:49–57.
Neaigus A, Reilly KH, Jenness SM, Hagan H, Wendel T, Gelpi-Acosta C. Dual HIV risk: receptive syringe sharing and unprotected sex among HIV-negative injection drug users in New York City. AIDS Behav. 2013;17(7):2501–9.
Blackstock OJ, Patel VV, Felsen U, Park C, Jain S. Pre-exposure prophylaxis prescribing and retention in care among heterosexual women at a community-based comprehensive sexual health clinic. AIDS Care. 2017;29(7):866–9.
Seidman DL, Weber S, Timoney MT, Oza KK, et al. Use of HIV pre-exposure prophylaxis during the preconception, antepartum and postpartum periods at two United States medical centers. AIDS Care. 2016;215(5):632.
Hodges-Mameletzis I, Fonner VA, Dalal S, Mugo N, Msimanga-Radebe B, Baggaley R. Pre-exposure prophylaxis for hiv prevention in women: current status and future directions. Drugs. 2019;79(12):1263–76.
Walters SM, Rivera AV, Starbuck L, Reilly KH, Boldon N, Anderson BJ, et al. Differences in awareness of pre-exposure prophylaxis and post-exposure prophylaxis among groups at-risk for HIV in New York State: New York City and Long Island, NY, 2011–2013. JAIDS. 2017;75:S383–91.
Walters SM, Kral AH, Simpson KA, Wenger L, Bluthenthal RN. HIV pre-exposure prophylaxis prevention awareness, willingness, and perceived barriers among people who inject drugs in Los Angeles and San Francisco, CA 2016–2018. Substance Use Misuse. 2020;1:1–11.
Kuhns LM, Reisner SL, Mimiaga MJ, Gayles T, Shelendich M, Garofalo R. Correlates of PrEP indication in a multi-site cohort of young HIV-uninfected transgender women. AIDS Behav. 2015;20:1470–7.
Wilson EC, Jin H, Liu A, Raymond HF. Knowledge, indications and willingness to take pre-exposure prophylaxis among transwomen in San Francisco, 2013. PLoS ONE. 2015;10(6):e0128971.
Bazzi AR, Biancarelli DL, Childs E, Drainoni M-L, Edeza A, Salhaney P, et al. Limited knowledge and mixed interest in pre-exposure prophylaxis for HIV prevention among people who inject drugs. AIDS Patient Care STDs. 2018;32:529–37.
Park CJ, Taylor TN, Gutierrez NR, Zingman BS, Blackstock OJ. Pathways to HIV pre-exposure prophylaxis among women prescribed PrEP at an urban sexual health clinic. J Assoc Nurs AIDS Care. 2019;30:321–9.
Nunn A, Zaller N, Cornwall A, Mayer KH, Moore E, Dickman S, et al. Low perceived risk and high HIV prevalence among a predominantly African American population participating in Philadelphia’s rapid HIV testing program. AIDS Patient Care STDS. 2011;25(4):229–35.
Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDS. 2015;29(2):102–10.
Flash CA, Stone VE, Mitty JA, Mimiaga MJ, Hall KT, Krakower D, et al. Perspectives on HIV prevention among urban Black women: a potential role for HIV pre-exposure prophylaxis. AIDS Patient Care STDS. 2014;28(12):635–42.
Rael CT, Martinez M, Giguere R, Bockting W, Maccrate C, Mellman W, et al. Barriers and facilitators to oral PrEP use among transgender women in New York City. AIDS Behav. 2018;22:3627–36.
Park C, Taylor T, Rios N, Khedimi R, Weiss C, Dolce E, et al editors. Perspectives of women prescribed HIV pre-exposure prophylaxis (PrEP). Open forum infectious diseases. Oxford: Oxford University Press; 2017.
Braksmajer A, Senn TE, McMahon J. the potential of pre-exposure prophylaxis for women in violent relationships. AIDS Patient Care STDS. 2016;30(6):274–81.
Sevelius JM, Keatley J, Calma N, Arnold E. ‘I am not a man’: trans-specific barriers and facilitators to PrEP acceptability among transgender women. Glob Public Health. 2016;11(7–8):1060–75.
Bradley E, Forsberg K, Betts JE, DeLuca JB, Kamitami E, Porter SE, et al. Factors affecting pre-exposure prophylaxis implementation for women in the United States: A systematic review. J Women’s Health. 2019;28:1272–85.
Aaron E, Blum C, Seidman D, Hoyt MJ, Simone J, Sullivan M, et al. Optimizing delivery of hiv preexposure prophylaxis for women in the United States. AIDS Patient Care STDS. 2018;32(1):16–23.
Johnson LM, Green HD Jr, Koch B, Stockman JK, Felsher M, Roth AM, et al. Role of social networks and social norms in future PrEP use in a racially diverse sample of at-risk women and members of their social networks. JAIDS. 2021;86(4):422–9.
Glick JL, Russo R, Jivapong B, Rosman L, Pelaez D, Footer KHA, et al. The PrEP care continuum among cisgender women who sell sex and/or use drugs globally: a systematic review. AIDS Behav. 2020;24(5):1312–33.
Bradford JB, Coleman S, Cunningham W. HIV system navigation: an emerging model to improve HIV care access. AIDS Behav. 2007;21(s1):S49–58.
Higa DH, Marks G, Crepaz N, Liau A, Lyles CM. Interventions to improve retention in HIV primary care: a systematic review of US studies. Curr HIV/AIDS Rep. 2012;9(4):313–25.
Rajabiun S, Cabral H, Tobias C, Relf M. Program design and evaluation strategies for the special projects of national significance outreach initiative. AIDS Patient Care STDs. 2007;21(s1):S9–19.
Davidson L, Amy CB, Guy K, Er RAM. Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry. 2012;11(2):123–8.
Sledge WH, Lawless M, Sells D, Wieland M, O’Connell MJ, Davidson L. Effectiveness of peer support in reducing readmissions of persons with multiple psychiatric hospitalizations. Psychiatr Serv. 2011;62(5):541–4.
Bassuk EL, Hanson J, Greene RN, Richard M, Laudet A. Peer-delivered recovery support services for addictions in the United States: a systematic review. J Subst Abuse Treat. 2016;63:1–9.
Bardwell G, Kerr T, Boyd J, McNeil R. Characterizing peer roles in an overdose crisis: preferences for peer workers in overdose response programs in emergency shelters. Drug Alcohol Depend. 2018;190:6–8.
Lennox R, Lamarche L, O’Shea T. Peer support workers as a bridge: a qualitative study exploring the role of peer support workers in the care of people who use drugs during and after hospitalization. Harm Reduct J. 2021;18(1):467.
Blackstock OJ, Platt J, Golub SA, Anakaraonye AR, Norton BL, Walters SM, et al. A pilot study to evaluate a novel pre-exposure prophylaxis peer outreach and navigation intervention for women at high risk for HIV infection. AIDS Behav. 2020;25:1411–22.
HIV Surveillance Annual Report, 2018 (Rep.). (2019, November). Retrieved May 07, 2020, from New York City Department of Health and Mental Hygiene website: https://www1.nyc.gov/assets/doh/downloads/pdf/dires/hiv-surveillance-annualreport-2018.pdf
DiClemente RJ, Crosby RA, Kegler MC. Emerging theories in health promotion practice and research. Hoboken: Wiley; 2009.
Grant RM, Pellegrini M, Defechereux PA, Anderson PL, Yu M, Glidden DV, et al. Sex hormone therapy and tenofovir diphosphate concentration in dried blood spots: primary results of the iBrEATHe study. Clin Infect Dis. 2020. https://doi.org/10.1093/cid/ciaa1160.
Lee R, Cui RR, Muessig KE, Thirumurthy H, Tucker JDJA. Incentivizing HIV/STI testing: a systematic review of the literature. Behavior. 2014;18(5):905–12.
Stopka TJ, Marshall C, Bluthenthal RN, Webb DS, Truax SR. HCV and HIV counseling and testing integration in California: an innovative approach to increase HIV counseling and testing rates. Public Health Rep. 2007;122(2 suppl):68–73.
Abadie R, Brown B, Fisher CB. “Money Helps”: people who inject drugs and their perceptions of financial compensation and its ethical implications. Ethics Behav. 2018;29:607–29.
Charmaz K. Constructing grounded theory. Thousand Oaks: Sage; 2014.
Braun V, Clarke V. Thematic analysis. Washington: APA; 2012.
MacQueen KM, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. CAM J. 1998;10(2):31–6.
Miles MB, Huberman AM, Saldana J. Qualitative data analysis. Tbousand Oaks: Sage; 2013.
Orne J, Bell M. An invitation to qualitative fieldwork: a multilogical approach. New York: Routledge; 2015.
Aidala A, Cross JE, Stall R, Harre D, Sumartojo E. Housing status and HIV risk behaviors: implications for prevention and policy. AIDS Behav. 2005;9(3):251–65.
Stoner MCD, Haley DF, Golin CE, Adimora AA, Pettifor A. The relationship between economic deprivation, housing instability and transactional sex among women in North Carolina (HPTN 064). AIDS Behav. 2019;23:2946–55.
Dunkle KL, Wingood GM, Camp CM, DiClemente RJ. Economically motivated relationships and transactional sex among unmarried African American and white women: Results from a US national telephone survey. Public Health Rep. 2010;125:90–100.
Qin Y, Price C, Rutledge R, Puglisi L, Madden LM, Meyer JP. Women’s decision-making about PrEP for HIV prevention in drug treatment contexts. JIAPAC. 2020;19:232595821990009.
Wilson EC, Turner CM, Arayasirikul S, Lightfoot M, Scheer S, Raymond HF, et al. Disparities in the PrEP continuum for trans women compared to MSM in San Francisco, California: Results from population-based cross-sectional behavioural surveillance studies. J Int AIDS Soc. 2020;23:S3.
Nydegger LA, Dickson-Gomez J, Ko TK. Structural and syndemic barriers to PrEP adoption among Black women at high risk for HIV: a qualitative exploration. Cult Health Sex. 2020;23:659–73.
Felsher M, Ziegler E, Smith LR, Sherman SG, Amico KR, Fox R, et al. An Exploration of pre-exposure prophylaxis (PrEP) initiation among women who inject drugs. Arch Sex Behav. 2020;49:2205–10.
Felsher M, Piecara B, Krakower D, Bellamy S, Laurano R, Van Der Pol B, et al., editors. Offering PrEP Care within a Community-based Syringe Exchange Facilitates Uptake among Women Who Inject Drugs. APHA's 2019 Annual Meeting and Expo (Nov 2-Nov 6); 2019: American Public Health Association.
Kamis KF, Marx GE, Scott KA, Gardner EM, Wendel KA, Scott ML, et al. Same-day HIV pre-exposure prophylaxis (PrEP) initiation during drop-in sexually transmitted diseases clinic appointments is a highly acceptable, feasible, and safe model that engages individuals at risk for HIV into PrEP care. Open Forum Infect Dis. 2019;6:7.
Rowan SE, Patel RR, Schneider JA, Smith DK. Same-day prescribing of daily oral pre-exposure prophylaxis for HIV prevention. Lancet HIV. 2020;8:e114–20.
Muncan B, Walters SM, Ezell J, Ompad DC. “They look at us like junkies”: influences of drug use stigma on the healthcare engagement of people who inject drugs in New York City. Harm Reduct J. 2020;17:1.
Earnshaw V, Smith L, Copenhaver M. Drug addiction stigma in the context of methadone maintenance therapy: an investigation into understudied sources of stigma. Int J Ment Health Addict. 2013;11(1):110–22.
Goparaju L, Praschan NC, Jeanpiere LW, Experton LS, Young MA, Kassaye S. Stigma, partners, providers and costs: Potential barriers to PrEP uptake among US women. J AIDS Clin Res. 2017;08:09.
Auerbach JD, Moran L, Watson C, Weber S, Keatley J, Sevelius J. We are all women: barriers and facilitators to inclusion of transgender women in HIV treatment and support services designed for cisgender women. AIDS Patient Care STDS. 2020;34(9):392–8.
Martinez AN, Lorvick J, Kral AH. Activity spaces among injection drug users in San Francisco. Int J Drug Policy. 2014;25(3):516–24.
Butner JL, Gupta N, Fabian C, Henry S, Shi JM, Tetrault JM. Onsite treatment of HCV infection with direct acting antivirals within an opioid treatment program. J Subst Abuse Treat. 2017;75:49–53.
Carey KJ, Huang W, Linas BP, Tsui JI. Hepatitis C virus testing and treatment among persons receiving buprenorphine in an office-based program for opioid use disorders. J Subst Abuse Treat. 2016;66:54–9.
Masson CL, Delucchi KL, McKnight C, Hettema J, Khalili M, Min A, et al. A randomized trial of a hepatitis care coordination model in methadone maintenance treatment. Am J Public Health. 2013;103(10):e81–8.
Muncan B, Jordan AE, Perlman DC, Frank D, Ompad DC, Walters SM. Acceptability and effectiveness of hepatitis C care at syringe service programs for people who inject drugs in New York city. Subst Use Misuse. 2021;1:1–10.
Walters SM, Coston B, Neaigus A, Rivera AV, Starbuck L, Ramirez V, et al. The role of syringe exchange programs and sexual identity in awareness of pre-exposure prophylaxis (PrEP) for male persons who inject drugs. Int J Drug Policy. 2020;77:102671.
Roth AM, Aumaier BL, Felsher MA, Welles SL, Martinez-Donate AP, Chavis M, et al. An exploration of factors impacting preexposure prophylaxis eligibility and access among syringe exchange users. Sex Transm Dis. 2018;45(4):217–21.
Pinto RM, Berringer KR, Melendez R, Mmeje O. Improving PrEP implementation through multilevel interventions: a synthesis of the literature. AIDS Behav. 2018;22(11):3681–91.
New York City Department of Health and Mental Hygiene. Risk factors that contributed to HIV outbreaks in Massachusetts are present in New York City. 2019 Advisory (No. 3). https://www1.nyc.gov/assets/doh/downloads/pdf/han/advisory/2019/risk-factors-HIV-outbreaks-present-in-NYC.pdf. Published 2019. Accessed 7 May 2020.
Walters S. COVID-19 and people who use drugs: a commentary. Health Behav Policy Rev. 2020;7(5):489–97.
Acknowledgements
We are grateful to Tonia Poteat, PhD, PA-C, MPH, and Hilary Surratt, PhD for insightful discussions during the early stages of this project and to Axcel Barboza for his input into planning and implementation phases of this study. The authors would also like to thank colleagues at NDRI for their assistance with Peer training. This project was supported by a Centers for Disease Control and Prevention Minority HIV/AIDS Research Initiative Grant (1U01PS005111-01).
Funding
This work was funded by the Centers for Disease Control and Prevention Minority HIV/AIDS Research Initiative Grant (1U01PS005111-01), PI: Oni J. Blackstock; T32 DA007233-31, PI: Falkin; and R25DA026401, PI Avelardo Valdez.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Walters, S.M., Platt, J., Anakaraonye, A. et al. Considerations for the Design of Pre-exposure Prophylaxis (PrEP) Interventions for Women: Lessons Learned from the Implementation of a Novel PrEP Intervention. AIDS Behav 25, 3987–3999 (2021). https://doi.org/10.1007/s10461-021-03353-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03353-2