Abstract
There are few studies on the occurrence of food insecurity (FI) in pregnant women living with HIV/AIDS (PrWLWHA). Our objective was to estimate the prevalence of food insecurity among PrWLWHA and to analyse the association between HIV and FI. For this we searched eight databases. We used the prevalence and prevalence ratio (PR) with a 95% confidence interval (CI) as the summary measurements for the meta-analysis. We identified 300 studies, 13 of which were eligible. The prevalence of FI was 64%, ranging between 26% (mild), 33% (moderate) and 27% (severe). People living with HIV/AIDS (PLWHA) had a 23% greater chance of facing FI (PR = 1.23, 95% CI 1.16–1.38) compared to those not living with HIV. The results revealed a high prevalence and positive association with FI among PLWHA, which suggests the need for food security assessments in HIV/AIDS clinical care.
Resumen
Existen pocos estudios sobre la ocurrencia de inseguridad alimentaria (IF) en mujeres embarazadas que viven con el VIH (PrWLWHA). Nuestro objetivo fue estimar la prevalencia de IF entre las personas que viven con el VIH/SIDA y analizar la asociación entre el VIH y la IF. Se realizaron búsquedas en ocho bases de datos. La prevalencia y la razón de prevalencia (RP) con un intervalo de confianza (IC) del 95% se utilizaron como medidas de resumen para el metanálisis. Se identificaron 300 estudios y 13 fueron seleccionados. La prevalencia de la IF fue del 64%, oscilando entre el 26% (leve), el 33% (moderada) y el 27% (grave). PrWLWHA tenían un 23% más de posibilidades de afrontar la IF (RP = 1,23, IC del 95% = 1,16–1,38) en comparación con las que no viven con el VIH. Los resultados revelaron una alta prevalencia y una asociación positiva entre la IF entre las PVVS, lo que sugiere la necesidad de una evaluación de la seguridad alimentaria en la atención clínica del VIH/SIDA.
Similar content being viewed by others
Introduction
HIV is a global public health problem [1]. It has been estimated that 38 million people are living with HIV (PLWH) globally, and 1.7 million new infections occurred in 2019 worldwide [2]. Epidemiological data on HIV infections in pregnant women from low- and middle-income countries (LMICs) show a high incidence rate. In particular, pregnant women in Africa have a high HIV incidence rate (4.7/100 persons per year), equivalent to other key populations on the continent, such as professional sex workers and HIV serodiscordant couples [3]. Moreover, recent data have shown that only 82% of pregnant women worldwide have access to antiretroviral medicines to prevent child HIV transmission [2]. In addition, women in the Middle East and North Africa (28%) and Western and Central Africa (59%) have the poorest access to antiretroviral therapy during pregnancy [2].
HIV infection among pregnant women has been associated with a range of factors (biological, behavioural, and structural). Biological factors among pregnant women, such as elevated progesterone concentrations that can induce systemic or genital mucosal changes, make them vulnerable to HIV infection [4]. In addition, behavioural factors such as unprotected sex during pregnancy can increase the risk of HIV infection [3], as can structural factors in LMICs, which are marked by low socioeconomic conditions, limited access to health services, violence, and food insecurity (FI) [5].
FI can be conceptualised as the violation of the human right to adequate food [6]. When there is a lack of adequate food, in both quantitative and qualitative terms, it denies people their right to life through limited or uncertain opportunities to acquire acceptable foods in socially acceptable ways, or through limited or uncertain availability of nutritionally adequate and safe foods [1, 5]. Recent meta-analyses have indicated that food insecurity is associated with incomplete viral suppression among PLWH with lower CD4 rates [1, 7, 8]. Thus, FI may impair immunological recovery and viral suppression in PLWH [1].
Food insecurity and HIV can have a bi-directional relationship, intensified during periods of heightened nutritional needs, such as during reproduction or HIV infection [9]. In LMICs there is an increased prevalence of food insecurity in the population. However, the evidence on iniquities and their relationship with the occurrence of HIV represents an important research agenda. The hope is that systematic review studies involving pregnant women living with HIV can contribute to broadening this debate and understanding the magnitude of FI among pregnant women. Therefore, estimating the prevalence of FI among PLWHA is important to increase the evidence for direct clinical practices and public health policies in LMICs at a local and national level in order to improve maternal-infant health.
There are a limited number of meta-analyses on the relationship between FI and HIV in different populations and age groups, which indicates the need for new evidence on the subject. On the other hand, no meta-analyses were found in the epidemiological literature about the occurrence of FI in pregnant women living with HIV/AIDS (PrWLWHA). Considering that FI is also associated with viral suppression [10], this review estimated the prevalence of FI among PrWLWHA and analysed the association between HIV and FI in pregnant women.
Methodology
This is a systematic review study with a meta-analysis that sought to answer the following question: What is the prevalence of FI in PrWLWHA living in LMICs?
Eligibility Criteria
To define the eligibility criteria, the PECO structure was adopted. Thus, the population of interest (P) was PrWLWHA living in LMICs, the exposure considered (E) was HIV, the comparator (C) was those who were not exposed to HIV, and the outcome of interest (O) was the prevalence of FI. Cross-sectional studies, cohort studies and clinical trials that reported baseline prevalence data were also eligible. Literature reviews and studies that assessed FI postpartum were excluded.
LMICs were defined using the World Bank list of countries (https://datahelpdesk.worldbank.org) based on the year in which each study was conducted.
Data Sources and Searches
The review process followed the Meta-analysis of Observational Studies in Epidemiology guidelines [11]. Two researchers independently searched the Medline/PubMed, Web of Science, Scopus, Science Direct and Lilacs databases in February and March of 2019 (and subsequently reviewed the results in January of 2020) using the search terms ‘pregnant women’, ‘human immunodeficiency viruses’, ‘HIV’, ‘food insecurity’, and ‘food supply’ (Table S1). There were no temporal restrictions for the selected studies.
The publications were chosen based on a combination of these search terms and the key question. The reference list of relevant articles was then manually searched to identify additional articles. Published papers were managed using the Mendeley® program.
Study Selection and Data Collection
The articles identified in the databases were independently selected by the reviewers, who screened the titles and abstracts for relevance and adequacy. Disagreements were resolved by consensus. The articles that potentially met the inclusion criteria were read in full.
The following information was collected from the eligible studies: author, year of publication, period, location, study design, sample, number of PrWLWHA, and diagnostic methods used for FI and FI prevalence. For clinical trials and cohort studies, the data were strained from the pregnancy baseline [9, 12,13,14,15,16,17].
Risk of Bias Assessment for the Included Studies
The methodological quality of the studies was assessed by two independent reviewers using the Prevalence Critical Appraisal tool [18]. This tool includes nine items that examine the internal and external validity of the methodological quality of studies reporting prevalence data. For each criterion met, the study received a ‘yes’. The total number of ‘yes’ answers was counted for each study. The larger the number of ‘yes’ answers, the lower the risk of bias in the study. Any inconsistencies in data abstraction and quality assessment between the reviewers were resolved through consensus.
Statistical Analyses
The study outcome was food insecurity and its different levels, if available in the chosen study. From this perspective, the following can be defined:
-
1.
Food insecurity: this covers any type of violation of the human right to adequate food. A lack of adequate food, in both quantitative and qualitative terms, can deny people their right to life [6].
-
1.1
Mild FI: household sometimes or often worries about not having enough food, and/or is unable to eat preferred foods, and/or eats a more monotonous diet than desired and/or some foods considered undesirable, but only rarely. But it does not cut back on quantity or experience any of the three most severe conditions [19].
-
1.2
Moderate FI: sacrifices quality more frequently, by sometimes or often eating a monotonous diet or undesirable foods, and/or has rarely or sometimes started to cut back on quantity by reducing the size of meals or number of meals [19].
-
1.3
Severe FI: often cuts back on meal size or number of meals, and/or experiences any of the three most severe conditions (running out of food, going to bed hungry, or going a whole day and night without eating), even if infrequently or rarely [19].
The prevalence and prevalence ratio (PR) with a 95% confidence interval (CI) were used as the summary measurement for the meta-analysis, and the results were presented as forest plots. The DerSimonian and Laird method was used to estimate the variability parameter between the studies [20]. Heterogeneity was assessed using the Cochran test and Q test, and its magnitude was calculated using the I-square (I2) [21]. The inconsistency test (I2 > 50%) was used as an indicator of elevated heterogeneity [21].
The data from the studies included in the meta-analysis were transformed through the logit function to satisfy the normality assumption of the meta-analytic model of random effects [22]. The confidence intervals for the results of the individual studies were calculated using the Coppler-Pearson method. Publication bias was not evaluated because this is not appropriate in the case of prevalence assessments in meta-analyses [23].
Meta-regressions identified the causes of heterogeneity using the Knapp and Hartung test to analyse the following variables: quality score, sample size, publication year, and type of scale used to analyse FI. In all analyses, a p value of < 0.05 was considered statistically significant. The STATA 14 statistical program (Stata Corp, College Station, TX, USA) was used for the data analysis.
Results
Characteristics of the Selected Studies
The search strategies are presented in Fig. 1. We identified 366 publications in the 8 databases. After removing duplicate records, we analysed the titles and abstracts of the remaining 300 and ultimately included 13 in this review (9, 10, 11–15, 21–26). The reasons for excluding articles were the absence of an evaluation of FI in PrWLWHA (3) and the lack of an analysis of FI in pregnant women (12) (List S1).
The studies were published between 2007 and 2019, and the majority (8) were developed in Kenya [9, 17, 24, 25] and Uganda [12, 15, 16, 26], with their samples varying from 171 to 1225 participants. The total number of participants was 2901 PrWLWHA.
The majority (10) used cross-sectional [25,26,27,28,29] and cohort [9, 12, 13, 17, 24] designs, with 3 using interventions [14,15,16]. Most [9, 17, 24, 26] of the studies used the Individually Focused Food Insecurity Access Scale to evaluate the FI situation of the pregnant women (Table 1).
When classifying the studies for risk of bias, we found that most entailed a high risk (11). There was also a predominance of articles with flaws in their statistical analyses, which did not report the confidence interval estimates of the prevalence of FI. Other criteria that scored negatively were sample selection, population representativeness, sample size, and not using good FI assessment scales for pregnant women (Fig. 2).
Main Results
The prevalence of FI in PrWLWHA was 64% (95% CI 55–74, I2 = 99.45%), with 26% being mild (95% CI 15–36, I2 = 98.32%), 33% moderate (95% CI 23–43, I2 = 96.35%), and 27% severe (95% CI 17–40, I2 = 98.35%) (Fig. 3).
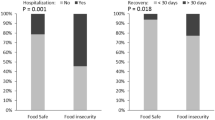
In a meta-analysis that evaluated the association between HIV and FI using five articles [9, 13, 14, 17, 28], PrWLWHA had a higher prevalence of FI (PR = 1.23, 95% CI 1.16–1.38) than those without HIV (Fig. 4). The result of the inconsistency test showed high heterogeneity among the studies analysed (I2 = 64.5%, p = 0.00). Thus, the random effects model was used to calculate the summarisation measurement.
Results of Subgroup Analysis and Meta-regression
The subgroup analysis found a statistically significant difference between the prevalence of FI in the cohort (P = 84%, 95% CI 77–90%, I2 = 98.46%) and transversal (P = 38%, 95% CI 17–60, I2 = 97.78%) studies. Similar results were found for the FI evaluation method (Table 2).
Two meta-regressions were performed to investigate the heterogeneity of the prevalence. In the analysis of the prevalence of IF, the meta-regression for the selected variables indicated that the risk of bias score was a source of heterogeneity (p = 0.04). The sample size, year of publication, study design, and scale used were not possible causes of the heterogeneity found in the analysis of the studies (p > 0.05).
In the second meta-regression, which analysed the association between HIV and FI using five articles, sample size (p = 0.46), year of publication (p = 0.74), study design (p = 0.99), scale (p = 0.26), and bias risk score (p = 0.32) did not present a statistically significant result; that is, they were not possible sources of the heterogeneity.
Discussion
HIV and FI During Pregnancy
The results of the first meta-analysis on the FI situation of PrWLWHA identified a high occurrence of FI, with a predominance of moderate and severe forms of FI. Pregnant women living with HIV are 23% more likely to experience FI compared to HIV-negative pregnant women. Thus, the results available in the literature indicate a high prevalence of FI, with hunger or food deprivation, among PrWLWHA.
Most of the reviewed studies were conducted in sub-Saharan African countries, which did not permit an estimation of FI on other continents. The results of this study are valuable for the epidemiological context of Africa, considering that the studies were developed on that continent. The epidemiological scenario of vulnerability in many African countries, marked by social and health inequalities, means that the HIV/AIDS epidemic is prevalent among women [2]. The UNAIDS estimates for 2018 indicated that in sub-Saharan Africa, young women between 15 and 24 years old were twice as likely to be living with HIV than men [2].
In these countries, pregnant women may be particularly vulnerable to FI. This is probably due to their high social vulnerability because of poor schooling in low- and middle-income countries as well as women’s reduced decision-making power regarding how to spend financial resources [8, 30]. The requirements of gestation increase women’s specific nutritional needs but reduce their physical ability to earn income and obtain and prepare food [31]. Thus, the high occurrence of FI in pregnant women may be due to gender inequalities, social class, and biological determinants.
The association between FI and HIV in pregnant women can be bi-directional. The absence of food in a household may contribute to the adoption of strategies to fight hunger, such as having unprotected sex for money, increasing the chance of HIV transmission and infection [5, 31]. This can have a negative effect on mental health, making women vulnerable to depression and increased drug abuse [5, 31]. This, in turn, can increase the risk of HIV transmission and immune system depletion, leading to incomplete viral suppression, non-compliance with antiretroviral therapy, treatment interruptions, and the emergence of AIDS-related illnesses.
Another aspect is that PrWLWHA are more vulnerable to FI because their ability to generate income can be affected by discrimination, stigma, and reduced job opportunities due to them having the infection [5, 30]. For a household, when most of the productive members of the family have HIV, its economic capacity may be reduced [30], which results in lower regular and permanent access to a sufficient quantity and quality of food to meet the nutritional, cultural, and biological needs of the individuals.
The high occurrence of FI among pregnant women indicated the possibility of gender inequities. A recent review found that women living with HIV have a higher probability of experiencing FI than men [8]. Other estimates show that FI in African countries is more prevalent in households headed by women [32].
FI makes PrWLWHA vulnerable to having a poor nutritional status, which has been associated with adverse pregnancy outcomes such as low birth weight and prematurity [16]. Inadequate weight gain during pregnancy and nutritional deficiencies, especially in macro- and micro-nutrients, have also been observed [16, 30, 33]. Such conditions may favour decreased adherence to antiretroviral therapy, a reduced baseline CD4 cell count, incomplete virologic suppression, and decreased survival [30, 33], as well as an increased chance of vertical HIV transmission [5]. The results of our study are a public health concern, since FI in PrWLWHA can increase maternal–foetal morbidity and mortality and represents a measurable, modifiable, and early marker of maternal and child vulnerability [5, 8, 30].
In this context, reducing FI is essential to ensure the human right to adequate food and it would positively impact global health goals, including UN Sustainable Development Goal 3 and UNAIDS 90-90-90, as well as those relating specifically to maternal and child health, notably the UNAIDS super fast-track target of fewer than 20,000 new paediatric HIV infections by 2020 [34].
Developing intervention strategies to reduce FI in PrWLWHA constitutes a strategic prevention action aimed at reducing iniquities and complications associated with HIV in this group [35]. The results of the PROMOTE trial, carried out in Uganda in Africa, showed that PrWLWHA who had started ART and were exposed to food insecurity presented lower chances of sustained viral suppression during pregnancy and breastfeeding and after five years of monitoring [36].
Interventions to reduce poverty and FI primarily aim to improve access to food, through food vouchers and money transfers [35]. Studies in Sub-Saharan Africa, Haiti, and Honduras have recorded that food supplementation provided as part of HIV treatment can lead to better adhesion to TARV and better clinical adhesion [37,38,39]. In Zambia, it was recorded that more participants in the food supplementation group achieved higher adhesion compared with the controls [38].
Notably, although money transfers and food supplementation may be appropriate during initial treatment and the start of TARV, they are limited in scalability and sustainability in the absence of financial commitments from the government or other fund providers. It should also be noted that these interventions for confronting poverty and FI have been carried in weak and heterogeneous way in poor countries and have been unable to resolve social inequality [40], which can directly impact the FI situation of PrWLWHA. Moreover, they do not address the determinants of food insecurity [35, 41]
It is suggested that the interventions needed to deal with food insecurity should include programs and policies that involve means of subsistence and support for pregnant women, the adoption of effective behavioural changes, communication regarding gender roles to improve nutritional state, and the integration of foods and nutritional security programs into HIV treatment and care [35, 41]
On the other hand, we recognize the need to expand the supply of combination HIV prevention among fertile-aged women living in African countries. Monitoring of the cascade of care for HIV should be strengthened within the context of public policies [42]. Moreover, we recognize the positive implications of community interventions aimed at empowering the community, reducing violence against women, and increasing HIV testing [43]. In the prenatal context, the partner’s presence should be strengthened [44], when possible, given that the man’s participation in the prenatal stage can improve adhesion to TARV and prevent perinatal complications.
Limitations and Future Research
This meta-analysis has several limitations. Because the studies were carried out solely in African countries, they did not reflect the estimates of FI in other countries. In addition, due to the different study designs adopted, methodological comparisons were difficult. Nevertheless, the methodological rigour and well-established criteria made this study consistent.
The studies contained a variable risk of bias due to the following aspects: samples selected without adopting probabilistic criteria, samples not being representative of the population, sample size not being calculated, FI assessment scales not being used for pregnant women, and statistical analyses of prevalence not reporting estimates of the variability of FI in the population. Therefore, many of the selected studies were considered to have a severe risk of bias. Good planning, an appropriate sampling process, and high methodological and statistical quality should be considered in future research to minimise the risk of bias.
One of the strengths of this review is the use of different databases and the inclusion of grey literature to select studies, which reduced the risk of selection bias. In addition, possible causes of heterogeneity were investigated through meta-regression and subgroup analyses to permit a better understanding of the high variability between the studies, observing that the risk of bias in the studies was one of the sources of heterogeneity.
Finally, the results of the present study indicate that FI is a problem that commonly occurs in PrWLWHA in African countries, more so than in the world population estimates [32]. However, new studies covering not only the criteria already mentioned but also other epidemiological scenarios and contexts of vulnerability are necessary for the impact of FI to be widely investigated in PrWLWHA, in order to facilitate the development of interventions.
The conclusions of this analysis will help to support the development of programs and appropriate interventions to help eliminate problems related to FI and poor quality of life among PrWLWHA. Our results demonstrate a high incidence of IF in pregnant women with HIV and suggest the need to consider evaluating the food security situation in clinical practice, especially in the treatment of HIV infections.
FI in Pregnant Women with HIV in the COVID-19 Pandemic: Necessary Considerations
We observed a high prevalence of FI in pregnant women from low-income countries, constituting a challenge in fighting HIV/AIDS. In 2020, the COVID-19 pandemic brought a new challenge in coping with IF and HIV care and treatment, aggravating the occurrence of both grievances.
The effects of the economic crisis may be worse for low- and very-low-income countries, especially in vulnerable populations [45, 46]. Pregnant women with HIV form part of such populations. Several factors can be associated with the greater vulnerability of pregnant women to FI during the COVID-19 pandemic [47].
It could be suggested that access to adequate and healthy food may be impaired because of unemployment, reduced access to locally sourced or street market food, and the risk of food shortages [48]. Thus, it can be predicted that the pandemic may increase nutritional deficiencies, the consumption of ultra-processed foods, and hunger in pregnant women exposed to social inequities and HIV during the pandemic.
On the other hand, it must be considered that access to resources to fight hunger may be compromised. Outbreaks of COVID-19 have been observed among workers at popular restaurants and in the food production sector with low-cost food supplies, leading to the closure of these spaces, which can decrease the supply of meals for people in a vulnerable context. Another important dimension is that pandemic mitigation strategies may decrease access to health services for prenatal care, antiretroviral treatment, and childbirth assistance due to transport limitations, fear of COVID-19 infections, and a lack of financial resources. It is suggested that any small reduction in the coverage and use of maternal and child health services will significantly increase maternal and child mortality in different populations. Thus, telehealth strategies could be adopted when appropriate to enable care during pregnancy and to avoid an increase in vertical HIV transmission rates and adverse perinatal events.
We recognise the need to develop and focus social programs to guarantee the human right to adequate food and care for HIV/AIDS, especially in this pandemic context, bearing in mind that pregnant women and people in a vulnerable context are more exposed to COVID-19 because their adherence to social isolation can be compromised due to their need to gso to work and earn an income. In low-income countries in particular, macroeconomic actions must focus on tackling new social inequities related to COVID-19.
References
Aibibula W, Cox J, Hamelin A-M, McLinden T, Klein MB, Brassard P. Association between food insecurity and HIV viral suppression: a systematic review and meta-analysis. AIDS Behav. 2017;21:754–65.
UNAIDS. UNAIDS 2019 Data [Internet]. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2019. p. 1–248. Available from: https://www.unaids.org/sites/default/files/media_asset/2019-UNAIDS-data_en.pdf.
Mugo NR, Heffron R, Donnell D, et al. Increased risk of HIV-1 transmission in pregnancy: a prospective study among African HIV-1-serodiscordant couples. AIDS. 2011;25:1887–95.
Sheffield JS, Wendel GDJ, McIntire DD, Norgard MV. The effect of progesterone levels and pregnancy on HIV-1 coreceptor expression. Reprod Sci. 2009;16:20–31.
Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, Tien PC, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94:1729S-1739S.
Demetrio F, de Santos ST, Santos DB, Pereira M. Food insecurity in pregnant women is associated with social determinants and nutritional outcomes: a systematic review and meta-analysis. Cien Saude Colet. 2020;25(7):2663–76.
Aibibula W, Cox J, Hamelin A-M, Mamiya H, Klein MB, Brassard P. Food insecurity and low CD4 count among HIV-infected people: a systematic review and meta-analysis. AIDS Care. 2016;28:1577–85.
Boneya DJ, Ahmed AA, Yalew AW. The effect of gender on food insecurity among HIV-infected people receiving anti-retroviral therapy: a systematic review and meta-analysis. PLoS ONE. 2019;14:e0209903.
Widen EM, Tsai I, Collins SM, et al. HIV infection and increased food insecurity are associated with adverse body composition changes among pregnant and lactating Kenyan women. Eur J Clin Nutr. 2019;73(3):474–82.
The Lancet HIV. The syndemic threat of food insecurity and HIV. Lancet HIV. 2020;7:e75.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
Young SL, Plenty AHJ, Luwedde FA, et al. Household food insecurity, maternal nutritional status, and infant feeding practices among HIV-infected Ugandan women receiving combination antiretroviral therapy. Matern Child Health J. 2014;18(9):2044–53.
Thomas E, Kuo C, Cohen S, et al. Mental health predictors of breastfeeding initiation and continuation among HIV infected and uninfected women in a South African birth cohort study. Prev Med. 2017;102:100–11.
Rotheram-Borus MJ, Tomlinson M, Scheffler A, Harris DM, Nelson S. Adjustment of a population of South African children of mothers living with/and without HIV through three years post-birth. AIDS Behav. 2017;21:1601–10.
Bartelink IH, Savic RM, Mwesigwa J, et al. Pharmacokinetics of lopinavir/ritonavir and efavirenz in food insecure HIV-infected pregnant and breastfeeding women in Tororo, Uganda. J Clin Pharmacol. 2014;54(2):121–32.
Koss CA, Natureeba P, Nyafwono D, et al. Brief report: food insufficiency is associated with lack of sustained viral suppression among HIV-infected pregnant and breastfeeding Ugandan women. J Acquir Immune Defic Syndr. 2016;71(3):310–5.
Murnane PM, Miller JD, Tuthill EL, et al. Perinatal food insecurity and postpartum psychosocial stress are positively associated among Kenyan women of mixed HIV status. AIDS Behav. 2020;24(6):1632–42.
Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. 2014;3(3):123–8.
Coates J, Swindale A, Bilinsky P. USAID food and nutrition technical assistance: Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide. J Chem Inf Model. 2007. 2017 [cited 2019 Mar 14]. Available from http://www.fao.org/fileadmin/user_upload/eufao-fsi4dm/doc-training/hfias.pdf.
Laird N, DerSimonian R. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Harris RJ, Bradburn MJ, Deeks JJ, Altman DG, Harbord RM, Sterne JAC. Metan: fixed- and random-effects meta-analysis. Stata J. 2008;8:3–28.
Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67:974–8.
Hunter JP, Saratzis A, Sutton AJ, Boucher RH, Sayers RD, Bown MJ. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol. 2014;67(8):897–903.
Tsai AC, Tomlinson M, Comulada WS, Rotheram-Borus MJ. Food insufficiency, depression, and the modifying role of social support: evidence from a population-based, prospective cohort of pregnant women in peri-urban South Africa. Soc Sci Med. 2016;151:69–77.
Ronen K, Osborn L, Khasimwa B, et al. Food insecurity is common and associated with unsuppressed viral load in HIV-infected pregnant women in Kenya. J Gen Intern Med. 2011;26(9):1012–8.
Natamba BK, Kilama H, Arbach A, Achan J, Griffiths JK, Young SL. Reliability and validity of an individually focused food insecurity access scale for assessing inadequate access to food among pregnant Ugandan women of mixed HIV status. Public Health Nutr. 2015;18(16):2895–905.
Perez-Escamilla R, Lartey A, Mazur R, Sellen D, Hromi-Fiedler A, Marquis GS. Food insecurity and HIV status among pregnant Ghanaian women: preliminary results from the RIING study. FASEB J. 2007;21:A311–A311.
Abrahams Z, Lund C, Field S, Honikman S. Factors associated with household food insecurity and depression in pregnant South African women from a low socio-economic setting: a cross-sectional study. Soc Psychiatry Psychiatr Epidemiol. 2018;53(4):363–72.
Ngocho JS, Watt MH, Minja L, et al. Depression and anxiety among pregnant women living with HIV in Kilimanjaro region, Tanzania. PLoS ONE. 2019;14:10224515.
Anema A, Vogenthaler N, Frongillo EA, Kadiyala S, Weiser SD. Food insecurity and HIV/AIDS: current knowledge, gaps, and research priorities. Curr HIV/AIDS Rep. 2009;6:224–31.
Weiser SD, Leiter K, Bangsberg DR, et al. Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLoS Med. 2007;4:1589–97.
Food and Agriculture Organization (FAO). State of food security and nutrition in the world 2017 [Internet]. 2017 [cited 2019 Mar 14]. Available from http://www.fao.org/gender/news/detail/en/c/1038453.
Normén L, Chan K, Braitstein P, et al. Food insecurity and hunger are prevalent among HIV-positive individuals in British Columbia, Canada. J Nutr. 2005;135(4):820–5.
Bailey H, Zash R, Rasi V, Thorne C. HIV treatment in pregnancy. Lancet HIV. 2018;5:e457–67.
Haberer JE, Sabin L, Amico KR, Orrell C, Galárraga O, Tsai AC, et al. Improving antiretroviral therapy adherence in resource-limited settings at scale: a discussion of interventions and recommendations. J Int AIDS Soc. 2017;20(1):21371. https://doi.org/10.7448/IAS.20.1.21371
Koss CA, Natureeba P, Kwarisiima D, Ogena M, Clark TD, Olwoch P, et al. Viral suppression and retention in care up to 5 years after initiation of lifelong ART during pregnancy (Option B plus ) in rural Uganda. J Acquir Immune Defic Syndr. 2017;74(3):279–84.
Byron E, Gillespie S, Nangami M. Integrating nutrition security with treatment of people living with HIV: lessons from Kenya. Food Nutr Bull. 2008;29(2):87–97.
Cantrell RA, Sinkala M, Megazinni K, Lawson-Marriott S, Washington S, Chi BH, et al. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food-insecure adults in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2008;49(2):190–5.
Martinez H, Palar K, Linnemayr S, Smith A, Derose KP, Ramirez B, et al. Tailored nutrition education and food assistance improve adherence to HIV antiretroviral therapy: evidence from Honduras. AIDS Behav. 2014;18(Suppl 5):S566–77.
Pereira M, Oliveira AM. Poverty and food insecurity may increase as the threat of COVID-19 spreads. Public Health Nutr. 2020;23(17):3236–40.
Young S, Wheeler AC, McCoy SI, Weiser SD. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav. 2014;18(Suppl 5):S505–15.
Avert. HIV and AIDS in East and Southern Africa regional overview. [Internet]. Global information and education on HIV and AIDS. 2020. Available from https://www.avert.org/professionals/hiv-around-world/sub-saharan-africa.
Colombini M, James C, Ndwiga C, Team I, Mayhew SH. The risks of partner violence following HIV status disclosure, and health service responses: narratives of women attending reproductive health services in Kenya. J Int AIDS Soc. 2016;19(1):20766.
Maeri I, El Ayadi A, Getahun M, Charlebois E, Akatukwasa C, Tumwebaze D, et al. “How can I tell?” Consequences of HIV status disclosure among couples in eastern African communities in the context of an ongoing HIV “test-and-treat” trial. AIDS Care. 2016;28(Suppl 3):59–66.
McLinden T, Stover S, Hogg RS. HIV and Food insecurity: a syndemic amid the COVID-19 pandemic. AIDS Behav. 2020;24:2766–9.
Arndt C, Davies R, Gabriel S, et al. Covid-19 lockdowns, income distribution, and food security: an analysis for South Africa. Glob Food Sec. 2020;26:100410.
Akseer N, Kandru G, Keats EC, Bhutta ZA. COVID-19 pandemic and mitigation strategies: implications for maternal and child health and nutrition. Am J Clin Nutr. 2020;112(2):251–6.
Pu M, Zhong Y. Rising concerns over agricultural production as COVID-19 spreads: lessons from China. Glob Food Sec. 2020;26:100409.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
MP contributed to the study conception, design, data collection, analysis and the draft of the manuscript. LSG contributed to design, data collection and writing the article. LM and ID revising it for important intellectual content. All authors commented on previous versions of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conficts of interest to disclose.
Research Involving in Human and Animal Rights
No human or animal subjects were asked to participate for this review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pereira, M., Magno, L., da Silva Gonçalves, L. et al. HIV Infections and Food Insecurity Among Pregnant Women from Low- and Middle-Income Countries: A Systematic Review and Meta-analysis. AIDS Behav 25, 3183–3193 (2021). https://doi.org/10.1007/s10461-021-03280-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03280-2