Abstract
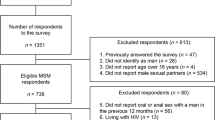
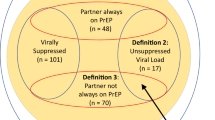
In Brazil, pre-exposure prophylaxis (PrEP) is currently available for gay, bisexual, and other men who have sex with men. As PrEP use depends on an individual’s perceived risk, we explored pathways by which potentially modifiable behaviors lead to high perceived HIV risk. Using online surveys (N = 16,667), we conducted a path analysis on the basis of ordered sequences of multivariate logistic regressions. High perceived HIV risk was low (26.3%) compared to condomless receptive anal sex (41.4%). While younger age increased the odds of binge drinking and of condomless receptive anal sex, it was associated with decreased odds of high perceived HIV risk. In contrast, use of stimulants increased the odds of condomless receptive anal sex and of high perceived HIV risk. Our results suggest that binge drinking and use of stimulants are key points in different pathways to high-risk sexual behavior and may lead to different perceptions of HIV risk.
Resumen
En Brasil, la profilaxis previa a la exposición (PrEP) está disponible actualmente para hombres homosexuales, bisexuales y otros hombres que tienen sexo con hombres. Como el uso de PrEP depende del riesgo percibido de una persona, exploramos vías por las cuales los comportamientos potencialmente modificables conducen a un alto riesgo percibido de VIH. Utilizando datos de encuestas en línea (N = 16.667), realizamos un análisis de ruta sobre la base de secuencias ordenadas de regresiones logísticas multivariadas. El alto riesgo percibido de VIH fue bajo (26,3%) en comparación con el sexo anal receptivo sin condón (41,4%). La edad más joven aumentó las probabilidades de consumo de alcohol en exceso y del sexo anal receptivo sin condón, todavía se asoció con una menor probabilidad de alta percepción de riesgo sobre VIH. Sin embargo, el uso de estimulantes aumentó las probabilidades de tener sexo anal receptivo sin condón y de un alto riesgo percibido de VIH. Nuestros resultados sugieren que el consumo excesivo de alcohol y el uso de estimulantes son puntos clave en diferentes vías de conductas sexuales de alto riesgo y pueden llevar a diferentes percepciones del riesgo de VIH.


Similar content being viewed by others
References
UNAIDS. Communities at the Centre. Available at https://www.unaids.org/sites/default/files/media_asset/2019-global-AIDS-update_en.pdf. 2019.
Ministério da Saúde. Boletim epidemiológico da AIDS e DST. Disponível em https://www.aids.gov.br/pt-br/pub/2018/boletim-epidemiologico-hivaids-2018. Data de acesso 11 janeiro 2018. 2018.
Kerr L, Kendall C, Guimaraes MDC, Salani Mota R, Veras MA, Dourado I, et al. HIV prevalence among men who have sex with men in Brazil: results of the 2nd national survey using respondent-driven sampling. Medicine (Baltimore). 2018;97(1):S9–S15.
Kerr LR, Mota RS, Kendall C, Pinho Ade A, Mello MB, Guimaraes MD, et al. HIV among MSM in a large middle-income country. AIDS. 2013;27(3):427–35.
MS. Protocolo Clínico e Diretrizes Terapêuticas para Profilaxia Pré-Exposição (PrEP) de Risco à Infecção pelo HIV. Available at https://www.aids.gov.br/pt-br/pub/2017/protocolo-clinico-e-diretrizes-terapeuticas-para-profilaxia-pre-exposicao-prep-de-risco. 2018.
Luz PM, Veloso VG, Grinsztejn B. The HIV epidemic in Latin America: accomplishments and challenges on treatment and prevention. Curr Opin HIV AIDS. 2019;14(5):366–73.
Torres TS, Marins LMS, Veloso VG, Grinsztejn B, Luz PM. How heterogeneous are MSM from Brazilian cities? An analysis of sexual behavior and perceived risk and a description of trends in awareness and willingness to use pre-exposure prophylaxis. BMC Infect Dis. 2019;19(1):1067.
Torres TS, Konda KA, Vega-Ramirez EH, Elorreaga OA, Diaz-Sosa D, Hoagland B, et al. Factors associated with willingness to use pre-exposure prophylaxis in Brazil, Mexico, and peru: web-based survey among men who have sex with men. JMIR Public Health Surveill. 2019;5(2):e13771.
Wilton J, Kain T, Fowler S, Hart TA, Grennan T, Maxwell J, et al. Use of an HIV-risk screening tool to identify optimal candidates for PrEP scale-up among men who have sex with men in Toronto, Canada: disconnect between objective and subjective HIV risk. J Int AIDS Soc. 2016;19(1):20777.
Plotzker R, Seekaew P, Jantarapakde J, Pengnonyang S, Trachunthong D, Linjongrat D, et al. Importance of risk perception: predictors of PrEP acceptance among thai MSM and TG women at a community-based health service. J Acquir Immune Defic Syndr. 2017;76(5):473–81.
Guimaraes MDC, Magno L, Ceccato M, Gomes R, Leal AF, Knauth DR, et al. HIV/AIDS knowledge among MSM in Brazil: a challenge for public policies. Rev Bras Epidemiol. 2019;1(1):e190005.
Cummings KM, Jette AM, Rosenstock IM. Construct validation of the health belief model. Health Educ Monogr. 1978;6(4):394–405.
Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15(2):175–83.
Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior: an AIDS risk reduction model (ARRM). Health Educ Q. 1990;17(1):53–72.
Kahneman D. Thinking, fast and slow. New York: Farrar, Straus and Giroux; 2013.
Kahneman D, Tversky A. Choices, values and frames. Am Psychol. 1984;39:341–50.
Blumenthal-Barby JS, Krieger H. Cognitive biases and heuristics in medical decision making: a critical review using a systematic search strategy. Med Decis Making. 2015;35(4):539–57.
Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: systematic review and meta-analysis of experimental studies. Addiction. 2012;107(1):51–9.
Torres TS, Bastos LS, Kamel L, Bezerra DRB, Fernandes NM, Moreira RI, et al. Do men who have sex with men who report alcohol and illicit drug use before/during sex (chemsex) present moderate/high risk for substance use disorders? Drug Alcohol Depend. 2020;209:107908.
Torres TS, De Boni RB, de Vasconcellos MT, Luz PM, Hoagland B, Moreira RI, et al. Awareness of prevention strategies and willingness to use preexposure prophylaxis in brazilian men who have sex with men using apps for sexual encounters: online cross-sectional study. JMIR Public Health Surveill. 2018;4(1):e11.
Torres TS, Luz PM, De Boni RB, de Vasconcellos MTL, Hoagland B, Garner A, et al. Factors associated with PrEP awareness according to age and willingness to use HIV prevention technologies: the 2017 online survey among MSM in Brazil. AIDS Care. 2019;31(10):1193–202.
Hoagland B, Moreira RI, De Boni RB, Kallas EG, Madruga JV, Vasconcelos R, et al. High pre-exposure prophylaxis uptake and early adherence among men who have sex with men and transgender women at risk for HIV Infection: the PrEP Brasil demonstration project. J Int AIDS Soc. 2017;20(1):1–14.
Becker C, Fried R, Kuhnt S. Robustness and complex data structures. 1st ed. New York: Springer; 2013.
Cox DR, Wermuth N. Multivariate dependencies : models, analysis, and interpretation. Boca Raton: Chapman & Hall/CRC; 1998.
Almeida-Brasil CC, Moodie EEM, McLinden T, Hamelin AM, Walmsley SL, Rourke SB, et al. Medication nonadherence, multitablet regimens, and food insecurity are key experiences in the pathway to incomplete HIV suppression. AIDS. 2018;32(10):1323–32.
Blumenthal J, Jain S, Mulvihill E, Sun S, Hanashiro M, Ellorin E, et al. Perceived versus calculated HIV risk: implications for pre-exposure prophylaxis uptake in a randomized trial of men who have sex with men. J Acquir Immune Defic Syndr. 2019;80(2):e23–e2929.
Khawcharoenporn T, Mongkolkaewsub S, Naijitra C, Khonphiern W, Apisarnthanarak A, Phanuphak N. HIV risk, risk perception and uptake of HIV testing and counseling among youth men who have sex with men attending a gay sauna. AIDS Res Ther. 2019;16(1):13.
Seekaew P, Pengnonyang S, Jantarapakde J, Meksena R, Sungsing T, Lujintanon S, et al. Discordance between self-perceived and actual risk of HIV infection among men who have sex with men and transgender women in Thailand: a cross-sectional assessment. J Int AIDS Soc. 2019;22(12):e25430.
MS. Boletim epidemiologico de DST e AIDS. Departamento de DST/AIDS e Hepatites Virais. Secretaria de Vigilancia em Saude. Ministerio da Saude. Brasilia. Available at www.aids.gov.br. 2018
MacKellar DA, Valleroy LA, Secura GM, Behel S, Bingham T, Celentano DD, et al. Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: opportunities for advancing HIV prevention in the third decade of HIV/AIDS. J Acquir Immune Defic Syndr. 2005;38(5):603–14.
Sharot T. The optimism bias. Curr Biol. 2011;21(23):R941–R945945.
Prestage G, Down IA, Bradley J, McCann PD, Brown G, Jin F, et al. Is optimism enough? Gay men's beliefs about HIV and their perspectives on risk and pleasure. Sex Transm Dis. 2012;39(3):167–72.
Sharma A, Kahle EM, Sullivan SP, Stephenson R. Birth cohort variations across functional knowledge of HIV prevention strategies, perceived risk, and HIV-associated behaviors among gay, bisexual, and other men who have sex with men in the United States. Am J Mens Health. 2018;12(6):1824–34.
Grucza RA, Sher KJ, Kerr WC, Krauss MJ, Lui CK, McDowell YE, et al. Trends in adult alcohol use and binge drinking in the early 21st-century United States: a meta-analysis of 6 national survey series. Alcohol Clin Exp Res. 2018;42(10):1939–50.
Guimaraes MDC, Kendall C, Magno L, Rocha GM, Knauth DR, Leal AF, et al. Comparing HIV risk-related behaviors between 2 RDS national samples of MSM in Brazil, 2009 and 2016. Medicine (Baltimore). 2018;97(1):S62–S6868.
Laranjeira R, Marques AC, Ramos Sde P, Campana A, Luz E Jr, Franca J. Who runs alcohol policy in Brazil? Addiction. 2007;102(9):1502–3.
Laranjeira R, Pinsky I, Sanches M, Zaleski M, Caetano R. Alcohol use patterns among Brazilian adults. Braz J Psychiatry. 2010;32(3):231–41.
Warren EA, Paterson P, Schulz WS, Lees S, Eakle R, Stadler J, et al. Risk perception and the influence on uptake and use of biomedical prevention interventions for HIV in sub-Saharan Africa: a systematic literature review. PLoS ONE. 2018;13(6):e0198680.
Bavinton BR, Jin F, Prestage G, Zablotska I, Koelsch KK, Phanuphak N, et al. The Opposites Attract Study of viral load, HIV treatment and HIV transmission in serodiscordant homosexual male couples: design and methods. BMC Public Health. 2014;14:917.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375(9):830–9.
Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Degen O, et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. Lancet. 2019;393(10189):2428–38.
Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, van Lunzen J, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316(2):171–81.
Wang L, Moqueet N, Lambert G, Grace D, Rodrigues R, Cox J, et al. Population-level sexual mixing By HIV status and pre-exposure prophylaxis use among men who have sex with men in Montreal, Canada: implications for HIV prevention. Am J Epidemiol. 2019. https://doi.org/10.1093/aje/kwz231.
MS. Boletim epidemiologico de DST e AIDS. Departamento de DST/AIDS e Hepatites Virais. Secretaria de Vigilancia em Saude. Ministerio da Saude. Brasilia. Available at www.aids.gov.br. 2019.
Massignam FM, Bastos JL, Nedel FB. Discrimination and health: a problem of access. Epidemiologia e Serviços de Saúde. 2015;24(3):541–4.
Latalova K, Kamaradova D, Prasko J. Perspectives on perceived stigma and self-stigma in adult male patients with depression. Neuropsychiatr Dis Treat. 2014;10:1399–405.
Skagerlund K, Forsblad M, Slovic P, Vastfjall D. The affect heuristic and risk perception-stability across elicitation methods and individual cognitive abilities. Front Psychol. 2020;11:970.
Slovic P, Finucane ML, Peters E, MacGregor DG. The affect heuristic. Eur J Oper Res. 2007;177:1333–522.
Fitzgerald-Husek A, Van Wert MJ, Ewing WF, Grosso AL, Holland CE, Katterl R, et al. Measuring stigma affecting sex workers (SW) and men who have sex with men (MSM): a systematic review. PLoS ONE. 2017;12(11):e0188393.
Sabido M, Kerr LR, Mota RS, Benzaken AS, deGuimaraes APA, et al. Sexual violence against men who have sex with men in Brazil: a respondent-driven sampling survey. AIDS Behav. 2015;19(9):1630–41.
Macinko J, Mullachery P, Proietti FA, Lima-Costa MF. Who experiences discrimination in Brazil? Evidence from a large metropolitan region. Int J Equity Health. 2012;11:80.
Smolen JR, Araujo EM. Race/skin color and mental health disorders in Brazil: a systematic review of the literature. Cien Saude Colet. 2017;22(12):4021–30.
Pascoe EA, Smart RL. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–54.
Andersson GZ, Reinius M, Eriksson LE, Svedhem V, Esfahani FM, Deuba K, et al. Stigma reduction interventions in people living with HIV to improve health-related quality of life. Lancet HIV. 2020;7(2):e129–e140140.
Grinsztejn B, Hoagland B, Moreira RI, Kallas EG, Madruga JV, Goulart S, et al. Retention, engagement, and adherence to pre-exposure prophylaxis for men who have sex with men and transgender women in PrEP Brasil: 48 week results of a demonstration study. Lancet HIV. 2018;5(3):e136–e145145.
CGIBR. Comitê Gestor da Internet no Brasil (CGIBR). TIC Domicílios. Usuários de Internet, indicador ampliado. Centro Regional para o Desenvolvimento da Sociedade da Informação. Available at: https://www.cetic.br/tics/domicilios/2018/individuos/C2A/. 2018.
Ferrer RA, Klein WM, Persoskie A, Avishai-Yitshak A, Sheeran P. The Tripartite model of risk perception (TRIRISK): distinguishing deliberative, affective, and experiential components of perceived risk. Ann Behav Med. 2016;50(5):653–63.
Napper LE, Fisher DG, Reynolds GL. Development of the perceived risk of HIV scale. AIDS Behav. 2012;16(4):1075–83.
Chandler J, Shapiro D. Conducting clinical research using crowdsourced convenience samples. Ann Rev Clin Psychol. 2016;12:53–81.
Lambert G, Cox J, Hottes TS, Tremblay C, Frigault LR, Alary M, et al. Correlates of unprotected anal sex at last sexual episode: analysis from a surveillance study of men who have sex with men in Montreal. AIDS Behav. 2011;15(3):584–95.
Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482.
Acknowledgements
Gilead Sciences covered the costs related to advertisement of the 2016 and 2017 surveys. The 2018 survey was made possible thanks to Unitaid’s funding and support. Unitaid accelerates access to innovative health products and lays the foundations for their scale-up by countries and partners. Gilead and Unitaid played no role in the study design, collection, analysis, or interpretation of data, the writing of the manuscript, or the decision to submit this manuscript for publication.
Funding
PML acknowledges funding from Coordenação de Aperfeiçoamento Pessoal de Nível Superior (CAPES) and Programa de Internacionalização da Fundação Oswaldo Cruz (PrInt-FIOCRUZ-CAPES). EEMM acknowledges receipt of a chercheur boursier career award from the Fonds de recherche du Québec—Santé.
Author information
Authors and Affiliations
Contributions
TST, LM, VGV and BG conceived and implemented the surveys. TST, CCAB, JC, EEMM and PML conceived this study. TST and PML analyzed the data and generated the tables and figures. CCAB, JC, and EEMM provided guidance on statistical analyses and results interpretation. TST and PML reviewed the literature and drafted the manuscript. All authors critically revised the manuscript for important intellectual content and approved the final version of the manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luz, P.M., Torres, T.S., Almeida-Brasil, C.C. et al. High-Risk Sexual Behavior, Binge Drinking and Use of Stimulants are Key Experiences on the Pathway to High Perceived HIV Risk Among Men Who Have Sex with Men in Brazil. AIDS Behav 25, 748–757 (2021). https://doi.org/10.1007/s10461-020-03035-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-03035-5