Abstract
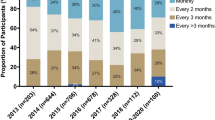
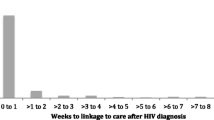
Retention in early HIV care has been associated with virologic suppression and improved survival, but remains understudied in Brazil. We estimated retention in early HIV care for the period 2000–2013, and identified socio-demographic and clinical factors associated with good retention in an urban cohort from Rio de Janeiro, Brazil. Antiretroviral therapy-naïve, HIV-infected persons ≥18 years old linked to care between 2000 and 2011 were included. Retention in the first 2 years post-linkage (i.e. early care) was defined by the proportion of 6-month intervals with ≥1 HIV laboratory result. “Good” retention was defined as ≥1 HIV laboratory result recorded in at least three intervals. Overall, 80 % of participants met criteria for good retention and retention significantly improved over the study period. Older age, higher education level and early antiretroviral therapy initiation were associated with good retention. Efforts to improve retention in early care in this population should target younger and less-educated HIV-infected persons.
Resumen
La retención temprana en el tratamiento del VIH ha sido asociada con supresión virológica y mejora de la sobrevida, pero esto ha sido poco estudiado en Brasil. Estimamos la retención temprana en el tratamento del VIH durante el período 2000-2013 e identificamos los factores socio-demográficos y clínicos relacionados con buena retención en una cohorte urbana de Río de Janeiro, Brasil. Personas infectadas con el VIH, sin tratamiento antiretroviral previo, con al menos 18 años de edad y que empezaron tratamento entre 2000 y 2011 fueron incluídos. La retención en los dos primeros años después del comienzo de tratamiento (es decir, “temprana en el tratamiento”) fue definida por la proporción de intervalos de seis meses en los que hubo al menos 1 resultado de laboratorio del VIH reportado. Definimos “buena” retención como tener un resultado de laboratorio para monitorear el VIH en al menos tres intervalos. En general, 80 % de los participantes cumplieron con el criterio para “buena retención” y esta mejoró significativamente durante el período del estudio. Mayor edad, nivel de educación superior y la iniciación temprana de la terapia antirretroviral estuvieron asociados con buena retención. Los esfuerzos para mejorar la retención temprana en el tratamiento en esta población deben dirigirse a las personas infectadas por el VIH más jóvenes y menos educados.


Similar content being viewed by others
References
Giordano TP, Gifford AL, White AC, et al. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis. 2007;44(11):1493–9.
Geng EH, Nash D, Kambugu A, et al. Retention in care among HIV-infected patients in resource-limited settings: emerging insights and new directions. Curr HIV/AIDS Rep. 2010;7(4):234–44.
Mugavero MJ, Norton WE, Saag MS. Health care system and policy factors influencing engagement in HIV medical care: piecing together the fragments of a fractured health care delivery system. Clin Infect Dis. 2011;52(Suppl 2):S238–46.
Metsch LR, Pereyra M, Messinger S, et al. HIV transmission risk behaviors among HIV-infected persons who are successfully linked to care. Clin Infect Dis. 2008;47(4):577–84.
Crawford TN, Sanderson WT, Breheny P, Fleming ST, Thornton A. Impact of non-HIV related comorbidities on retention in HIV medical care: does retention improve over time? AIDS Behav. 2014;18(3):617–24.
Mugavero MJ, Amico KR, Westfall AO, et al. Early retention in HIV care and viral load suppression: implications for a test and treat approach to HIV prevention. J Acquir Immune Defic Syndr. 2012;59(1):86–93.
Yehia BR, Rebeiro P, Althoff KN, et al. The impact of age on retention in care and viral suppression. J Acquir Immune Defic Syndr. 2014;68(4):413–9.
Ulett KB, Willig JH, Lin HY, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS. 2009;23(1):41–9.
Giordano TP, Hartman C, Gifford AL, Backus LI, Morgan RO. Predictors of retention in HIV care among a national cohort of US veterans. HIV Clin Trials. 2009;10(5):299–305.
Tripathi A, Youmans E, Gibson JJ, Duffus WA. The impact of retention in early HIV medical care on viro-immunological parameters and survival: a statewide study. AIDS Res Hum Retrovir. 2011;27(7):751–8.
Boletim Epidemiológico-AIDS e DST: Secretariat of Health Surveillance, Brazilian Ministry of Health, Department of STD AIDS and Viral Hepatitis; 2014.
CDC. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV—United States, 2011. MMWR. 2014;63:1113–7.
Rosen S, Fox M. Retention in HIV care between testing and treatment in Sub-Saharan Africa: a systematic review. PLoS Med. 2011;8(7):e1001056.
Mugavero MJ, Davila JA, Nevin CR, Giordano TP. From access to engagement: measuring retention in outpatient HIV clinical care. AIDS Patient Care STDS. 2010;24(10):607–13.
Mugavero MJ, Westfall AO, Zinski A, et al. Measuring retention in HIV care: the elusive gold standard. J Acquir Immune Defic Syndr. 2012;61(5):574–80.
Crawford TN, Sanderson WT, Thornton A. A comparison study of methods for measuring retention in HIV medical care. AIDS Behav. 2013;17(9):3145–51.
Yehia BR, Fleishman JA, Metlay JP, et al. Comparing different measures of retention in outpatient HIV care. AIDS. 2012;26(9):1131–9.
Rosen S, Fox MP, Gill CJ. Patient retention in antiretroviral therapy programs in sub-Saharan Africa: a systematic review. PLoS Med. 2007;4(10):e298.
Boletim Epidemiologico-AIDS e DST: Secretariat of Health Surveillance, Brazilian Ministry of Health, Department of STD AIDS and Viral Hepatitis; 2013.
Grinsztejn B, Veloso VG, Friedman RK, et al. Early mortality and cause of deaths in patients using HAART in Brazil and the United States. AIDS. 2009;23(16):2107–14.
Moreira RI, Luz PM, Struchiner CJ, et al. Immune status at presentation for HIV clinical care in Rio de Janeiro and Baltimore. J Acquir Immune Defic Syndr. 2011;57(Suppl 3):S171–8.
Grinsztejn B, Veloso VG, Pilotto JH, Campos DP, Keruly JC, Moore RD. Comparison of clinical response to initial highly active antiretroviral therapy in the patients in clinical care in the United States and Brazil. J Acquir Immune Defic Syndr. 2007;45(5):515–20.
Protocolo clínico e diretrizes terapêuticas para manejo da infecção pelo HIV em adultos: Brazilian Ministry of Health, Department of STD, AIDS and Viral Hepatitis; 2013.
Cohen SM, Hu X, Sweeney P, Johnson AS, Hall HI. HIV viral suppression among persons with varying levels of engagement in HIV medical care, 19 US jurisdictions. J Acquir Immune Defic Syndr. 2014;67(5):519–27.
Reveles KR, Juday TR, Labreche MJ, et al. Comparative value of four measures of retention in expert care in predicting clinical outcomes and health care utilization in HIV patients. PLoS ONE. 2015;10(3):e0120953.
1993 Revised Classification Systems for HIV Infection and Expanded Surveillance Case Definition for AIDS Among Adolescents and Adults. Vol 41. MMWR Recomm Rep: Centers for Disease Control and Prevention.
Nemes MI, Alencar TM, Basso CR, et al. Assessment of outpatient services for AIDS patients, Brazil: comparative study 2001/2007. Rev Saude Publica. 2013;47(1):137–46.
Recomendações para terapia anti-retroviral em adultos infectados pelo HIV: Brazilian Ministry of Health, National AIDS and STDs Program; 2008.
Grinsztejn B, Hosseinipour MC, Ribaudo HJ, et al. Effects of early versus delayed initiation of antiretroviral treatment on clinical outcomes of HIV-1 infection: results from the phase 3 HPTN 052 randomised controlled trial. Lancet Infect Dis. 2014;14(4):281–90.
Group ISS. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795–807.
Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
UNAIDS Global AIDS Response Progress Reporting: Brazil: Secretariat of Health Surveillance, Brazilian Ministry of Health, Department of STD AIDS and Viral Hepatitis; 2014.
Brito AM, Castilho EA, Szwarcwald CL. Regional patterns of the temporal evolution of the AIDS epidemic in Brazil following the introduction of antiretroviral therapy. Braz J Infect Dis. 2005;9(1):9–19.
Berkman A, Garcia J, Munoz-Laboy M, Paiva V, Parker R. A critical analysis of the Brazilian response to HIV/AIDS: lessons learned for controlling and mitigating the epidemic in developing countries. Am J Public Health. 2005;95(7):1162–72.
Szwarcwald CL, Souza-Junior PR, Damacena GN. Socioeconomic inequalities in the use of outpatient services in Brazil according to health care need: evidence from the World Health Survey. BMC Health Serv Res. 2010;10:217.
Carthery-Goulart MT, Anghinah R, Areza-Fegyveres R, et al. Performance of a Brazilian population on the test of functional health literacy in adults. Rev Saude Publica. 2009;43(4):631–8.
Silveira CM, Viana MC, Siu ER, de Andrade AG, Anthony JC, Andrade LH. Sociodemographic correlates of transitions from alcohol use to disorders and remission in the Sao Paulo megacity mental health survey, Brazil. Alcohol Alcoholism. 2011;46(3):324–32.
Silveira MF, Beria JU, Horta BL, Tomasi E, Victora CG. Factors associated with risk behaviors for sexually transmitted disease/AIDS among urban Brazilian women: a population-based study. Sex Transm Dis. 2002;29(9):536–41.
de Souza CT, Diaz T, Sutmoller F, Bastos FI. The association of socioeconomic status and use of crack/cocaine with unprotected anal sex in a cohort of men who have sex with men in Rio de Janeiro, Brazil. J Acquir Immune Defic Syndr. 2002;29(1):95–100.
Cardoso SW, Luz PM, Velasque L, et al. Effectiveness of first-line antiretroviral therapy in the IPEC cohort, Rio de Janeiro, Brazil. AIDS Res Ther. 2014;11:29.
Nemes MI, Carvalho HB, Souza MF. Antiretroviral therapy adherence in Brazil. AIDS. 2004;18(Suppl 3):S15–20.
Cardoso SW, Luz PM, Velasque L, et al. Outcomes of second-line combination antiretroviral therapy for HIV-infected patients: a cohort study from Rio de Janeiro, Brazil. BMC Infect Dis. 2014;14:699.
Tobias CR, Cunningham W, Cabral HD, et al. Living with HIV but without medical care: barriers to engagement. AIDS Patient Care STDS. 2007;21(6):426–34.
Gardner LI, Giordano TP, Marks G, et al. Enhanced personal contact with HIV patients improves retention in primary care: a randomized trial in 6 US HIV clinics. Clin Infect Dis. 2014;59(5):725–34.
Ashman JJ, Conviser R, Pounds MB. Associations between HIV-positive individuals’ receipt of ancillary services and medical care receipt and retention. AIDS Care. 2002;14(Suppl 1):S109–18.
Lo W, MacGovern T, Bradford J. Association of ancillary services with primary care utilization and retention for patients with HIV/AIDS. AIDS Care. 2002;14(Suppl 1):S45–57.
Messeri PA, Abramson DM, Aidala AA, Lee F, Lee G. The impact of ancillary HIV services on engagement in medical care in New York City. AIDS Care. 2002;14(Suppl 1):S15–29.
Barclay TR, Hinkin CH, Castellon SA, et al. Age-associated predictors of medication adherence in HIV-positive adults: health beliefs, self-efficacy, and neurocognitive status. Health Psychol. 2007;26(1):40–9.
Ryscavage P, Anderson EJ, Sutton SH, Reddy S, Taiwo B. Clinical outcomes of adolescents and young adults in adult HIV care. J Acquir Immune Defic Syndr. 2011;58(2):193–7.
Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS Care. 2007;19(1):28–33.
Dowshen N, Binns HJ, Garofalo R. Experiences of HIV-related stigma among young men who have sex with men. AIDS Patient Care STDS. 2009;23(5):371–6.
Naar-King S, Green M, Wright K, Outlaw A, Wang B, Liu H. Ancillary services and retention of youth in HIV care. AIDS Care. 2007;19(2):248–51.
Wohl AR, Garland WH, Wu J, et al. A youth-focused case management intervention to engage and retain young gay men of color in HIV care. AIDS Care. 2011;23(8):988–97.
Davila JA, Miertschin N, Sansgiry S, Schwarzwald H, Henley C, Giordano TP. Centralization of HIV services in HIV-positive African-American and Hispanic youth improves retention in care. AIDS Care. 2013;25(2):202–6.
Olatosi BA, Probst JC, Stoskopf CH, Martin AB, Duffus WA. Patterns of engagement in care by HIV-infected adults: South Carolina, 2004-2006. AIDS. 2009;23(6):725–30.
Sevelius JM, Patouhas E, Keatley JG, Johnson MO. Barriers and facilitators to engagement and retention in care among transgender women living with human immunodeficiency virus. Ann Behav Med. 2014;47(1):5–16.
Acknowledgments
We would like to thank all the participants enrolled in the INI HIV/AIDS program, as well as the hard working and dedicated staff at INI. We would also like to thank Eddy Segura for his assistance in translating our abstract into Spanish. Support for DS provided by the NIH R25 MH087222 (South American Program in HIV Prevention Research), the Infectious Disease Society of America and the American Society of Tropical Medicine and Hygiene. Support for JEL provided by the NIH K23 AI110532. PL and BG acknowledge funding from the National Council of Technological and Scientific Development (CNPq) and the Research Funding Agency of the State of Rio de Janeiro (FAPERJ).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
None.
Rights and permissions
About this article
Cite this article
Silva, D.S., De Boni, R.B., Lake, J.E. et al. Retention in Early Care at an HIV Outpatient Clinic in Rio de Janeiro, Brazil, 2000–2013. AIDS Behav 20, 1039–1048 (2016). https://doi.org/10.1007/s10461-015-1235-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1235-3