Abstract
Behavioral economics (BE) has been used to study a number of health behaviors such as smoking and drug use, but there is little knowledge of how these insights relate to HIV prevention and care. We present novel evidence on the prevalence of the common behavioral decision-making errors of present-bias, overoptimism, and information salience among 155 Ugandan HIV patients, and analyze their association with subsequent medication adherence. 36 % of study participants are classified as present-biased, 21 % as overoptimistic, and 34 % as having salient HIV information. Patients displaying present-bias were 13 % points (p = 0.006) less likely to have adherence rates above 90 %, overoptimistic clients were 9 % points (p = 0.04) less likely, and those not having salient HIV information were 17 % points (p < 0.001) less likely. These findings indicate that BE may be used to screen for future adherence problems and to better design and target interventions addressing these behavioral biases and the associated suboptimal adherence.
Similar content being viewed by others
Introduction
People commonly fail to act in their own self-interest and behave in ways they later regret such as overeating or smoking [1–3]. Behavioral economists study why and in what circumstances individuals display such decision-making errors or “biases” [4–8]. Insights from behavioral economics (BE) have been applied to study a number of diseases and health behaviors [9], but to date, none have explored HIV. BE is grounded in Traditional Economics (in particular the premise that people make decisions based on costs and benefits) but enriches this framework with insights from psychology. It also shares some characteristics with existing health behavior theories; like Social-cognitive Theory, it starts from the premise that expectations of future events and outcomes are important determinants of behavior [10]. Similarly, it recognizes the importance of beliefs in shaping behaviors stressed in the Health-Belief model [11]. With the Health-Belief model, it shares the recognition that people have limited cognitive capacity and may sometimes feel overwhelmed when carrying out a complex task [12]. Overall, BE is a systematic framework to investigate human actions that recognizes the importance of the behavioral determinants outlined across different health behavior theories. BE posits that people make decisions based on their costs and benefits, but contrary to the Traditional Economics model recognizes that people do not access all available information when making a decision (information salience), are overly confident in their capacity to carry out a task (overoptimism), and face difficulties sticking to their decisions (present-bias) [13]. A trademark of BE is the focus on measurement and quantification of these biases in a simple fashion. For example, compared to the related concept of time preference as used in an HIV context by Préau et al., the BE concept of present-bias as executed commonly is evaluated using only a handful of questions as compared to the 61 items in Zimbardo’s Stanford Time Perspective scale [14]. Questions identifying BE biases could therefore be a more feasible, much-needed tool to screen for likelihood of optimal medication adherence for HIV and other chronic conditions [15].
In what follows, we briefly discuss some key biases that have been found to influence behavior for chronic conditions, and discuss why we believe that these likely also matter for ARV adherence. We then present novel empirical evidence from a sample of HIV clients in Uganda showing that BE biases are common and negatively correlated with subsequent Medication Event Monitoring System (MEMS)-cap measured adherence. We end with a discussion of the results and in the conclusion encourage more research to further study these biases and their association with adherence.
The Importance of BE Biases for Chronic Health Behaviors
We focus on three key behavioral biases that have been found to influence health behaviors for other chronic conditions [9] and that we hypothesize may also be important to components of ARV adherence:
Present-Bias
A key behavioral bias is present-bias, which is the tendency of people to give into current temptation at the price of beneficial future outcomes [16]. For example, a seminal article by Benartzi found that people tend to delay the decision to save (e.g., to forego current consumption in exchange for future benefits) to a tomorrow that—when turning into today—is again pushed off [17]. Chronic HIV care management requires a similar decision, as health is conditional on daily pill-taking with immediate costs such as social stigma, side-effects, and financial costs. The benefits of optimal ARV adherence that include a healthier and longer life, on the other hand, manifest only in the distant future. We therefore hypothesize that patients displaying present-bias will display lower adherence, as they overly discount the future benefits of adherence and may see their actions guided mainly by its daily costs.
Overoptimism
Being overly confident in one’s ability to stick to a planned behavior has been found to have important negative consequences for a wide range of behaviors [18]. For ARV adherence, this bias may manifest itself as patients not taking appropriate steps to assure their taking the medicine on time or not taking it at all; for example, most patients in our sample set phone alarms that subsequently prove insufficient to assure optimal adherence. We hypothesize that patients displaying overoptimism will show lower adherence than their peers with more realistic expectations regarding their future adherence behavior. A closely related bias is overplacement, which is being overly confident in one’s own behavior relative to that of a reference group [19], which may be a particularly good indicator of being too confident and not taking enough precaution to ensure high adherence.
Information Salience
Behavioral economists have found that people act on the information that first comes to mind rather than on all the relevant information available [18]. This can lead to people being guided by relatively recent experiences, or those that were experienced by friends and that were particularly memorable. For example, people tend to buy earthquake insurance following an earthquake in their area, even though this occurrence does not change the underlying probability of an earthquake occurring [20]. We argue that HIV as a health threat may not be very salient (e.g., on top of their minds) for people living with HIV, in particular for those who have been on ARV for a number of years as is the case for the sample described below. Such patients often enjoy good health and no longer experience health improvements from taking their medication, therefore the benefits of ARV may become relatively invisible/less salient over time, leading them to fail to perceive adhering to the pill regimen as a priority. We expect that for patients who have received positive feedback on the ARV medication’s health benefits from peers at the HIV clinic this information is salient, leading to higher adherence.
Methods
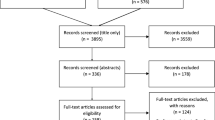
The data for this article come from the Rewarding Adherence Program (RAP) that uses variable rewards to improve ARV adherence and retention in care. The program attempts to reduce present-bias and increase information salience by providing small prizes allocated by a drawing at each clinic visit conditional on keeping scheduled clinic appointments (treatment group 1) and high ARV adherence measured by MEMS caps (treatment group 2). The study was implemented as a small randomized controlled trial (RCT) with about 50 participants in each of the two treatment groups and the control group, which received standard clinical care and answered the survey but did not take part in the prize drawings.
RAP is currently being implemented at Mildmay Uganda, an NGO in the capital Kampala. At the time of enrollment into the RAP program, patients completed a baseline survey before being informed of their randomized treatment assignment and before they were exposed to the intervention. This survey consisted of 11 different modules measuring a variety of characteristics such as patient demographics, household characteristics, or community environment. BE biases were also collected as part of this baseline survey as described below, and form the basis for the analysis in this paper. Eligible participants (18 years of age or older, taking ARVs for at least 2 years, having adherence problems (either self-reported or otherwise indicated in the medical records data) in the last 6 months, willing to follow and able to understand the study procedures) were asked to provide written consent in their preferred language (English or Luganda) that included the survey data collection and use of MEMS caps. RAP was approved by the HSPC Board at RAND (2012-0372), the IRB review board at Mildmay, and the Uganda National Science Counsel (UNCST).
Measurement of BE Biases
Present-Bias
The survey used the common method of asking clients to make a choice between hypothetical rewards that varied in size depending on the delay of payment [21]. The survey question stated: “Imagine you can win a lottery prize and have to choose between receiving 50,000 USh tomorrow, or 75,000 USh in one year. Which would you choose?”. Respondents who chose the immediate reward rather than the more distant, larger reward were subsequently classified as present-biased. This method has been validated across many cultural settings [6], and this particular question was designed for a similarly, resource-poor environment [22].
Overoptimism
Respondents were asked to report the likelihood of forgetting at least one dose in the next month based on a four point Likert-type scale, and to make the same judgment about the likelihood of other clients at the clinic to measure overplacement. As displaying adherence problems in the 6 months preceding the survey was one of the enrollment criteria for the RAP intervention, we expected study participants to realize that on average they are likely to display lower adherence than most other clinic patients. Patients therefore were classified as overconfident if they assigned themselves a lower likelihood of forgetting pill doses relative to the other clients in the clinic.
Information Salience
Patients were asked whether they know people who have benefited from ARVs (as a reminder of the benefits of ARVs), and whether they have a close friend or family member who has died from AIDS (which would make the serious consequences of non-adherence more salient). We do not report results for the latter measure as the large majority of the sample (over 90 %) responded in the affirmative, indicating the generalized nature of the HIV epidemic in Uganda.
Adherence Measures
Participants at baseline were provided with a MEMS cap that electronically records the date and time a pill bottle is opened, and were instructed to bring it with them for each clinic or study visit, at which point the adherence data were abstracted. Such an objective measure of adherence has been found to give a more accurate picture of adherence compared with self-reports that are easily manipulated and often overstated [23]. Objectively measuring adherence is particularly important in the current study where eligibility for participating in the prize drawing is conditional on high adherence (treatment group 2). Adherence so measured may differ from actual adherence if participants do not consistently use the caps, which we tried to control for by adjusting the measured adherence by self-reported pocketing or taking of medication from sources other than the MEMS cap. A second possible source of error in this measure is if people open the MEMS cap but do not actually swallow the pill. This would typically occur if people are trying to ‘game the system’. While we cannot control for this possibility, we can largely abstract from this problem for the control group and intervention group 1 as their eligibility in the lottery was not conditional on adherence but only on timely clinic visits.
MEMS data from the first 4 months of study participation are used to calculate the adherence outcome variable; we exclude the first month where we observe significantly higher adherence for all participants that is likely due to the novelty of being part of the study and focus our analysis on months two through four when we hypothesize that the novelty of using a MEMS cap would have worn off. Our main outcome variable is the fraction of clients displaying mean adherence of at least 90 %, where mean adherence is calculated as (# of actual bottle openings/# of prescribed bottle openings). While current regimens seem to be less forgiving than older ones [24], high and consistent adherence is certainly more conducive to viral suppression, and we therefore think that such a cut-off level is justified. Moreover, recent research has shown high risks for the development of disease resistant strains and advanced disease progression at mean adherence rates below 90 % [25, 26].
Approach
Data were analyzed with Stata/SE version 10.1. Statistical significance is reported for levels between 0.10 and 0.01 for hypothesis testing and regression coefficient estimates. Summary statistics are reported as frequency counts (%), and regression results present maximum likelihood estimation (MLE) coefficient estimates for probit regressions along with standard errors. Baseline results were compared among behavioral biases using chi-squared testing within the pooled sample of observations between months two and four. This method is well suited to the binary nature of the outcome variable and the non-normality of the underlying distribution of adherence behavior in the sample. To control for observable patient characteristics, probit regression results provide a secondary analysis of adherence behavior across biases.
Adherence as the primary RAP outcome is likely impacted by the intervention over time. During the first 4 months of the study, RAP’s impact would be little felt as few clients would have participated in a prize drawing during that time. We also repeated the analysis using the control group only (that did not receive the intervention) to ensure that the results observed are not driven by the RAP intervention. Furthermore, as the impact of the biases on ARV adherence can be expected to be muted by RAP (in particular present-bias that is directly targeted by the RAP rewards), our results constitute a lower bound estimate for these effects.
Results
Sample Characteristics (Table 1)
Table 1 presents summary statistics of the sample’s demographics and tests whether characteristics such as gender, age, and education status are equally distributed among the two intervention groups and the control group as would be expected in a RCT. These observable characteristics do not show statistically significant differences between the groups; however, present-bias is higher in the control group compared to the treatment group 2, and overoptimism is more prevalent in the control group than in treatment group 1.
Prevalence of BE Biases in the Sample (Table 1)
Present-Bias
36.3 % of respondents chose an immediate hypothetical reward over a larger reward in 1 year, and are therefore classified as present-biased.
Overoptimism
89 % of patients believe they are unlikely to miss a dose in the month following the baseline survey despite being recruited because of recent adherence problems. 20.7 % of clients believe that they have a better chance than the other patients at Mildmay clinic to fully adhere in the following month, indicating that they suffer from the bias of overplacement and leading to their being classified as overoptimistic.
Information Salience
More than 33 % of patients have received positive feedback on the effectiveness of the ARV medication from other HIV patients.
Association of Behavioral Economics Biases with Subsequent ARV Adherence (Table 2)
The biases presented in Table 1 may influence patients’ decision-making and consequently their adherence behavior. Table 2 provides empirical evidence on the impact of these biases on the fraction of patients taking 90 % or more of their medication.
Present-Bias
Patients who more heavily weigh the immediate costs of pill-taking than its future benefits are 13.4 % points less likely to attain mean adherence rates of at least 90 % (p = 0.006).
Overoptimism
Participants who report being ‘very likely’ to fully adhere in the next month are 13.4 % points more likely to have mean adherence rates equal or above 90 % (p = 0.07). The 20.7 % of patients who believe that they are more likely to show optimal adherence relative to others (i.e. those displaying overplacement), have an 9.4 % points lower chance to display 90 % adherence (p = 0.11).
Information Salience
The percentage of patients with mean adherence rates of 90 % or greater increases from 31.1 to 48.3 % for those who recently received positive feedback about the HIV medication from other patients (p = 0.001).
In Table 3, we investigate the association of the same BE biases with adherence when controlling for the observable characteristics of gender, age, and education of the participants to examine whether the behavioral biases exert an additional influence on adherence that cannot be inferred from these observable characteristics. Each column in the table represents a separate regression of adherence on the respective bias when controlling for the observable characteristics. We find that present-bias and information salience remain statistically significant; overoptimism has a negative impact on adherence that is however not statistically significant.
Robustness Check: Results in the Control Group
Above we discussed the potentially confounding influence of participation in the RAP program and uneven distribution of bias prevalence between control and treatment groups on adherence. We therefore repeated the analyses for the control group only (n = 50) that is not subjected to the intervention. The results confirm that patients with present-bias have a significantly lower mean adherence and are 15.3 % points less likely to achieve adherence over 90 % (p = 0.02). Similarly, the same patterns in adherence across patients’ overoptimism and information salience discussed above continue when restricting our analysis to this subgroup, but the small sample size limits the power of statistical inference.
Discussion
In this paper, we argue that the characteristics of HIV as a chronic disease make it likely that the systematic decision-making errors (‘biases’) of people living with HIV significantly interfere with optimal ARV adherence, and that measuring these biases and their association with ARV adherence is an important research topic. We focus on three key biases identified in the BE literature: present-bias (the tendency many people display of preferring immediate rewards to temporally more distant ones), overoptimism (excessive confidence in the ability to stick to a planned behavior), and information salience (the tendency of people to act on information that is more readily available). Our hypotheses that we subsequently test are that present-bias leads to lower adherence as adherence has current costs (stigma, financial costs, …) but the benefits of taking pills only manifest in the distant future (improved life expectancy and life quality). We also hypothesize that overoptimism may lead people not to implement enough precautions to take their daily drug dose(s) resulting in lower adherence, and that the long-term and relatively invisible nature of HIV reduces its information salience, making it likely for people to put the demands of daily life before HIV, again leading to lower adherence.
We then go on to test for the presence of these biases using commonly used, simple survey measures. We find that these biases are prevalent in a sample of clients in HIV care in an urban clinic in Uganda; more importantly, we find that these biases are associated with lower subsequent ARV adherence. These results represent the first empirical evidence for the importance of BE in studying ARV adherence, an area in need of further research and understanding, in particular in resource-limited settings [27]. While the biases empirically confirm the hypotheses we started out with, there was one unexpected finding: optimistic clients (i.e. those who think that they have taken good precautions to make sure to adhere to their regimen) manage to show higher adherence than their more pessimistic peers, indicating that some confidence in one’s ability to adhere to the medication regimen is actually beneficial. However, if patients are too confident in their ability to adhere (those who suffer from overplacement, i.e. the tendency to overstate their own ability to adhere compared to the general clinic population), they seem to not create an environment susceptible to good adherence and display lower adherence.
Our results point to several potential uses of BE for improving ARV adherence: first, BE biases could be a low-cost, quick way to screen for patients who are likely to show low adherence and are thus in need of additional adherence support. However, how useful biases are as a screening tool depends on the extent to which they cannot be inferred from observable characteristics such as age, gender or education that have been found to be associated with adherence and that are likely used by providers to infer the likelihood of a patient to show good adherence [28]. Our findings do indicate that BE biases are not systematically correlated with age, gender, or education, and therefore provide additional information that a provider would not be able to gather based on these observable client characteristics.
Our findings also point to the potential use of BE as way to design interventions that use the biases identified as entry points. For example, the finding that participants with present-bias display lower adherence indicates that interventions such as the RAP program may be able to improve adherence by providing short-term rewards to adherence. Similarly, the finding that information salience is associated with improved adherence suggests the importance of increasing the tangibility of the costs of non-adherence and benefits of adherence. This could for example take the form of reminders about the importance of adhering to the ARV regimen at times such as on weekend nights when individuals may be engaging in activities (drinking, drug use, …) that can lead them to forget to take their drugs.
Limitations of the study include that it is relatively small in size and may be contaminated by the RAP study that took place after the information on the biases was collected at baseline. However, the results for the control group that was not exposed to the intervention are equally robust. As this subsample consists of only 50 patients, the ability to detect any significant differences in mean adherence underscores the robustness of our results.
Conclusion
This paper presents first empirical evidence that BE can shed new light on ARV adherence behaviors. The finding that BE biases are common and are associated with subsequent ARV adherence supports the view of BE as a novel and low-cost way to screen for people in HIV care who are likely to show suboptimal adherence. We therefore encourage future research on the topic of BE biases and their impact on adherence using larger samples, using studies with the sole purpose of investigating the role of biases (i.e. not measuring biases as part of an intervention study), utilizing refined survey tools to detect biases, and using experiments in controlled settings to gain further insights. If the promising result in this study holds in these later studies, it would offer a simple tool to screen for clients likely needing additional treatment support. BE is increasingly being used to design and refine behavioral interventions for a range of (health) behaviors, and based on this literature and our results, we hope that BE methods can improve interventions for HIV-related behaviors as well. The RAP study discussed in this paper will provide first such evidence when it is completed in late 2015.
References
Charness G, Gneezy U. Incentives to exercise. Econometrica. 2009;77(3):909–31.
Heil S, Higgins S, Bernstein I, et al. Effects of voucher-based incentives on abstinence from cigarette smoking and fetal growth among pregnant women. Addiction. 2008;103:1009–18.
Barsky R, Juster T, Kimball M, Shapiro M. Preference parameters and behavioral heterogeneity: an experimental approach in the health and retirement study. Q J Econ. 1997;112(2):537–79.
Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science. 1974;185(4157):1124–31.
Kahneman D, Tversky A. Prospect theory: an analysis of decisions under risk. Econometrica. 1979;47(2):263–91.
Frederick S, Loewenstein G, O’Donoghue T. Time discounting and time preference: a critical review. J Econ Lit. 2002;14:351–401.
Thaler R, Sunstein C. Libertarian paternalism. Am Econ Rev. 2003;93(2):175–9.
Loewenstein G, Brennan T, Volpp K. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298(20):2415–7.
Rice T. The behavioral economics of health and health care. Annu Rev Publ Health. 2013;34:431–7.
Gebhardt W, Maes S. Integrating social-psychological frameworks for health behavior research. Am J Health Behav. 2001;25:528–36.
Janz N, Becker M. The health belief model: a decade later. Health Educ Behav. 1984;11(1):1–47.
Armitage C, Conner M. Social cognition models and health behavior: a structured review. Psychol Health. 2000;15:173–89.
Ariely D. Predictably irrational. New York: Harper Collins; 2008.
Préau M, Apostolidis T, Francois C, Raffi F, Spire B. Time perspective and quality of life among HIV-infected patients in the context of HAART. AIDS Care. 2007;19(4):449–58.
McHorney C. The adherence estimator: a brief, proximal screener for patient propensity to adhere to prescription medications for chronic disease. Curr Med Res Opin. 2009;25(1):215–38.
O’Donoghue T, Rabin M. Doing it now or later. Am Econ Rev. 1999;89(1):103–24.
Benartzi S. Save more tomorrow. New York: Pengiun; 2012.
Kahneman D. Thinking, fast and slow. New York: Macmillan; 2011.
Moore D, Healy P. The trouble with overconfidence. Psychol Rev. 2008;115(2):502–17.
Palm R, Hodgson M. After a California Earthquake: attitude and behavior change. The University of Chicago Geography Research Paper No. 233; 1992.
Coller M, Williams M. Eliciting individual discount rates. Exp Econ. 1999;2:107–27.
Cameron L, Shah M. Risk-taking behavior in the wake of natural disasters. J Hum Resour. 2015;50(12):484–515.
Arnsten J, Demas P, Farzadegan H, et al. Antiretroviral therapy adherence and viral suppression in HIV-infected drug users: comparison of self-report and electronic monitoring. Clin Infect Dis. 2001;33:1417–23.
Bangsberg D, Ware N, Simoni J. Adherence without access to antiretroviral therapy in sub-Saharan Africa? AIDS. 2006;20:140–1.
Turner B. Adherence to antiretroviral therapy by human immunodeficiency virus-infected patients. J Infect Dis. 2002;185:S143–51.
Raffa J, Tossonian H, Grebely J, Petkau J, DeVlaming S, Conway B. Intermediate highly active antiretroviral therapy adherence thresholds and empirical models for the development of drug resistance mutations. J AIDS. 2008;47(3):397–9.
Scanlon M, Vreeman R. Current strategies for improving access and adherence to antiretroviral therapies in resource-limited settings. HIV/AIDS–Res Palliat Care. 2013;5:1–17.
Fogarty L, Roter D, Larson S, Burke J, Gillespie J, Levy R. Patient adherence to HIV medication regimens: a review of published and abstract reports. Patient Educ Couns. 2002;46(2):93–108.
Acknowledgments
We would like to thank Mildmay Clinic under the leadership of Dr. Barbara Mukasa and study coordinator Tonny Kizza for their invaluable help in implementing the study. Thanks to Dr. Glenn Wagner, Dr. Arleen Leibowitz and Dr. Tom Rice for comments on an early draft, and two referees for insightful comments. Our gratitude goes most importantly to the study participants who gave so generously of their time and insights. This project was funded by the National Institute of Mental Health (NIMH), Grant Number R34MH096609. Sebastian Linnemayr is the principal investigator for the NIMH grant, and organized and coordinated the data collection efforts at the Mildmay Clinic in Kampala, Uganda. Both authors contributed equally to the data analyses and writing the paper. In memory of Esther Kawuma who made this study possible and who will be dearly missed by the RAND team.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Linnemayr, S., Stecher, C. Behavioral Economics Matters for HIV Research: The Impact of Behavioral Biases on Adherence to Antiretrovirals (ARVs). AIDS Behav 19, 2069–2075 (2015). https://doi.org/10.1007/s10461-015-1076-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1076-0