Abstract
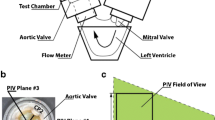
Long-term function of biological heart valve prostheses (BHV) is limited by structural deterioration leading to failure with associated arterial hypertension. The objective of this work was development of an easy to handle real-time pulse reactor for evaluation of biological and tissue engineered heart valves under different pressures and long-term conditions. The pulse reactor was made of medical grade materials for placement in a 37 °C incubator. Heart valves were mounted in a housing disc moving horizontally in culture medium within a cylindrical culture reservoir. The microprocessor-controlled system was driven by pressure resulting in a cardiac-like cycle enabling competent opening and closing of the leaflets with adjustable pulse rates and pressures between 0.25 to 2 Hz and up to 180/80 mmHg, respectively. A custom-made imaging system with an integrated high-speed camera and image processing software allow calculation of effective orifice areas during cardiac cycle. This simple pulse reactor design allows reproducible generation of patient-like pressure conditions and data collection during long-term experiments.









Similar content being viewed by others
Abbreviations
- BHV:
-
Biological heart valve prosthesis
- SBF:
-
Simulated body fluid
- EOA:
-
Effective orifice area
- TAD:
-
Tissue annulus diameter
- fps:
-
Frames per second
References
Aksoy, Y., C. Yagmur, G. O. Tekin, J. Yagmur, E. Topal, E. Kekilli, H. Turhan, F. Kosar, and E. Yetkin. Aortic valve calcification: association with bone mineral density and cardiovascular risk factors. Coron. Artery Dis. 16:379–383, 2005.
Blackman, B. R., G. Garcia-Cardena, and M. A. Gimbrone, Jr. A new in vitro model to evaluate differential responses of endothelial cells to simulated arterial shear stress waveforms. J. Biomech. Eng. 124:397–407, 2002.
Burdon, T. A., D. C. Miller, P. E. Oyer, R. S. Mitchell, E. B. Stinson, V. A. Starnes, and N. E. Shumway. Durability of porcine valves at fifteen years in a representative North American patient population. J. Thorac. Cardiovasc. Surg. 103:238–251, 1992; discussion 251–232.
Butany, J., C. Fayet, M. S. Ahluwalia, P. Blit, C. Ahn, C. Munroe, N. Israel, R. J. Cusimano, and R. L. Leask. Biological replacement heart valves. Identification and evaluation. Cardiovasc. Pathol. 12:119–139, 2003.
CEN Prop. Standard EN 120006-1. European Committee for Standardization, Brussels, Belgium, 1995.
Clark, R. E., and W. M. Swanson. In vitro durability of Hancock Model 242 porcine heart valve. J. Thorac. Cardiovasc. Surg. 78:277–280, 1979.
Deiwick, M., B. Glasmacher, E. Pettenazzo, D. Hammel, W. Castellon, G. Thiene, H. Reul, E. Berendes, and H. H. Scheld. Primary tissue failure of bioprostheses: new evidence from in vitro tests. Thorac. Cardiovasc. Surg. 49:78–83, 2001.
Dumont, K., J. Yperman, E. Verbeken, P. Segers, B. Meuris, S. Vandenberghe, W. Flameng, and P. R. Verdonck. Design of a new pulsatile bioreactor for tissue engineered aortic heart valve formation. Artif. Organs 26:710–714, 2002.
Engelmayr, Jr., G. C., E. Rabkin, F. W. Sutherland, F. J. Schoen, J. E. Mayer, Jr., and M. S. Sacks. The independent role of cyclic flexure in the early in vitro development of an engineered heart valve tissue. Biomaterials 26:175–187, 2005.
Engelmayr, Jr., G. C., V. L. Sales, J. E. Mayer, Jr., and M. S. Sacks. Cyclic flexure and laminar flow synergistically accelerate mesenchymal stem cell-mediated engineered tissue formation: implications for engineered heart valve tissues. Biomaterials 27:6083–6095, 2006.
FDA—Replacement Heart Valve Guide. FDA, Rockland, MD, USA, 1994.
Geens, J. H., S. Trenson, F. R. Rega, E. K. Verbeken, and B. P. Meyns. Ovine models for chronic heart failure. Int. J. Artif. Organs 32:496–506, 2009.
Gerosa, G., V. Tarzia, G. Rizzoli, and T. Bottio. Small aortic annulus: the hydrodynamic performances of 5 commercially available tissue valves. J. Thorac. Cardiovasc. Surg. 131:1058–1064, 2006.
Haaf, P., M. Steiner, T. Attmann, G. Pfister, J. Cremer, and G. Lutter. A novel pulse duplicator system: evaluation of different valve prostheses. Thorac. Cardiovasc. Surg. 57:10–17, 2009.
Hildebrand, D. K., Z. J. Wu, J. E. Mayer, Jr., and M. S. Sacks. Design and hydrodynamic evaluation of a novel pulsatile bioreactor for biologically active heart valves. Ann. Biomed. Eng. 32:1039–1049, 2004.
Hoerstrup, S. P., R. Sodian, S. Daebritz, J. Wang, E. A. Bacha, D. P. Martin, A. M. Moran, K. J. Guleserian, J. S. Sperling, S. Kaushal, J. P. Vacanti, F. J. Schoen, and J. E. Mayer, Jr. Functional living trileaflet heart valves grown in vitro. Circulation 102:III44–III49, 2000.
Hoerstrup, S. P., R. Sodian, J. S. Sperling, J. P. Vacanti, and J. E. Mayer, Jr. New pulsatile bioreactor for in vitro formation of tissue engineered heart valves. Tissue Eng. 6:75–79, 2000.
ISO 5840-2005 Cardiovascular implants—cardiac valve prostheses. http://www.iso.org.
Kokubo, T., and H. Takadama. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 27:2907–2915, 2006.
Lichtenberg, A., I. Tudorache, S. Cebotari, S. Ringes-Lichtenberg, G. Sturz, K. Hoeffler, C. Hurscheler, G. Brandes, A. Hilfiker, and A. Haverich. In vitro re-endothelialization of detergent decellularized heart valves under simulated physiological dynamic conditions. Biomaterials 27:4221–4229, 2006.
Mol, A., N. J. Driessen, M. C. Rutten, S. P. Hoerstrup, C. V. Bouten, and F. P. Baaijens. Tissue engineering of human heart valve leaflets: a novel bioreactor for a strain-based conditioning approach. Ann. Biomed. Eng. 33:1778–1788, 2005.
Montarello, J. K., A. C. Perakis, E. Rosenthal, E. G. Boyd, A. K. Yates, P. B. Deverall, E. Sowton, and P. V. Curry. Normal and stenotic human aortic valve opening: in vitro assessment of orifice area changes with flow. Eur. Heart J. 11:484–491, 1990.
Morsi, Y. S., W. W. Yang, A. Owida, and C. S. Wong. Development of a novel pulsatile bioreactor for tissue culture. J. Artif. Organs 10:109–114, 2007.
Narita, Y., K. Hata, H. Kagami, A. Usui, M. Ueda, and Y. Ueda. Novel pulse duplicating bioreactor system for tissue-engineered vascular construct. Tissue Eng. 10:1224–1233, 2004.
Netter, F. H. “Band 1: Herz.” In: Farbatlanten der Medizin—The Ciba Collection of Medical Illustrations, edited by M. Stauch. Stuttgart: Georg Thieme Verlag Stuttgart-New York, 1990, pp. 45.
Pohl, M., M. O. Wendt, B. Koch, R. Kuhnel, O. Samba, and G. Vlastos. Model fluids of blood for in vitro testing of artificial heart valves. Z. Med. Phys. 11:187–194, 2001.
Pohl, M., M. O. Wendt, S. Werner, B. Koch, and D. Lerche. In vitro testing of artificial heart valves: comparison between Newtonian and non-Newtonian fluids. Artif. Organs 20:37–46, 1996.
Reul, H., and K. Potthast. Durability/wear testing of heart valve substitutes. J. Heart Valve Dis. 7:151–157, 1998.
Ruzicka, D. J., W. B. Eichinger, I. M. Hettich, S. Bleiziffer, R. Bauernschmitt, and R. Lange. Hemodynamic performance of the new St. Jude Medical Epic Supra porcine bioprosthesis in comparison to the Medtronic Mosaic on the basis of patient annulus diameter. J. Heart Valve Dis. 17:426–433, 2008; discussion 434.
Schenke-Layland, K., F. Opitz, M. Gross, C. Doring, K. J. Halbhuber, F. Schirrmeister, T. Wahlers, and U. A. Stock. Complete dynamic repopulation of decellularized heart valves by application of defined physical signals—an in vitro study. Cardiovasc. Res. 60:497–509, 2003.
Stock, U. A., J. P. Vacanti, J. E. Mayer, Jr., and T. Wahlers. Tissue engineering of heart valves—current aspects. Thorac. Cardiovasc. Surg. 50:184–193, 2002.
Syedain, Z. H., and R. T. Tranquillo. Controlled cyclic stretch bioreactor for tissue-engineered heart valves. Biomaterials 30:4078–4084, 2009.
Warnock, J. N., S. Konduri, Z. He, and A. P. Yoganathan. Design of a sterile organ culture system for the ex vivo study of aortic heart valves. J. Biomech. Eng. 127:857–861, 2005.
Werner, S., M. O. Wendt, K. Schichl, M. Pohl, and B. Koch. Testing the hydrodynamic properties of heart valve prostheses with a new test apparatus. Biomed. Tech. (Berl) 39:204–210, 1994.
Weston, M. W., and A. P. Yoganathan. Biosynthetic activity in heart valve leaflets in response to in vitro flow environments. Ann. Biomed. Eng. 29:752–763, 2001.
Xing, Y., Z. He, J. N. Warnock, S. L. Hilbert, and A. P. Yoganathan. Effects of constant static pressure on the biological properties of porcine aortic valve leaflets. Ann. Biomed. Eng. 32:555–562, 2004.
Yacoub, M. H., and J. J. Takkenberg. Will heart valve tissue engineering change the world? Nat. Clin. Pract. Cardiovasc. Med. 2:60–61, 2005.
Yoganathan, A. P., Z. He, and S. Casey Jones. Fluid mechanics of heart valves. Annu. Rev. Biomed. Eng. 6:331–362, 2004.
Zapanta, C. M., E. G. Liszka, Jr., T. C. Lamson, D. R. Stinebring, S. Deutsch, D. B. Geselowitz, and J. M. Tarbell. A method for real-time in vitro observation of cavitation on prosthetic heart valves. J. Biomech. Eng. 116:460–468, 1994.
Zeltinger, J., L. K. Landeen, H. G. Alexander, I. D. Kidd, and B. Sibanda. Development and characterization of tissue-engineered aortic valves. Tissue Eng. 7:9–22, 2001.
Acknowledgments
This work was supported by a grant from the German Research Council (Deutsche Forschungsgemeinschaft) Sto 359/2-3, Sto 359/4-1 (U.A.S.), Sche701/2-1, Sche701/3-1 8 (S-L.K) and German Federal Institute for Risk Assessment (BFR-ZEBET) (U.A.S.).
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Jane Grande-Allen oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Schleicher, M., Sammler, G., Schmauder, M. et al. Simplified Pulse Reactor for Real-Time Long-Term In Vitro Testing of Biological Heart Valves. Ann Biomed Eng 38, 1919–1927 (2010). https://doi.org/10.1007/s10439-010-9975-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-010-9975-8