Abstract
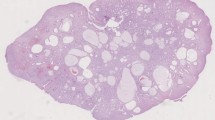
Hamartomatous polyposis syndromes are characterized by an overgrowth of cells or tissues native to the area in which they normally occur. Juvenile polyposis syndrome (JPS) results from germ-line mutations in the SMAD-4 gene (18q21.1) that encodes for an enzyme involved in transforming growth factor beta(TGF-β) signal transduction. The increased neoplastic risk may result from SMAD-4 mutations in the stromal component, which stimulate epithelial dysplasia and progression to invasive malignancy. Peutz-Jeghers syndrome (PJS) is associated with germ-line mutations in the LKB1 gene (19p13.3) that encodes a multifunctional serine-threonine kinase. These mutations occur in the epithelial component, suggesting a direct tumor suppressor effect. Patients are at an increased risk of intestinal and extraintestinal malignancies, including breast, pancreatic, ovarian, testicular, and cervical cancer. Cowden’s disease is associated with germ-line mutations in the PTEN gene (10q22–23) and an increased risk of breast and thyroid malignancies. Ruvalcaba-Myhre-Smith syndrome is less common; controversy suggests that it may represent a variant of Cowden’s disease.
Conclusions: Genetic alterations underlying hamartomatous polyposis syndromes are diverse. Carcinogenesis may result from either germ-line mutations in the stroma (JPS) or as a direct result of functional deletion of tumor suppressor genes (PJS). Diagnosis depends on clinical presentation and patterns of inheritance within families. Suggested surveillance guidelines for the proband and first-degree relatives are outlined.
Similar content being viewed by others
References
Haggitt RC, Reid BJ. Hereditary gastrointestinal polyposis syndromes. Am J Surg Pathol 1986; 10: 871–87.
Vogelstein B, Kinzler KW. The multistep nature of cancer. Trends Genet 1993; 9: 138–41
Kinzler KW, Vogelstein B. Landscaping the cancer terrain. Science 1998; 280: 1036–7.
McColl I, Bussey HJR, Veale AMO, Morrison BC. Juvenile polyposis coli. Proc R Soc Med 1964; 57: 896–7.
Desai DC, Neale KF, Talbot IC, Hodgson SV, Phillips RKS. Juvenile polyposis. Br J Surg 1995; 82: 14–17.
Giardiello FM, Hamilton SR, Kern SE. Colorectal neoplasia in juvenile polyposis or juvenile polyposis. Arch Dis Child 1991; 66: 971–5.
Sachatello CR, Hahn IS, Carrington CB. Juvenile gastrointestinal polyposis in a female infant: Report of a case and review of the literature of a recently recognized syndrome. Surgery 1974; 75: 107–14.
Jacoby RF, Schlack S, Cole CE, Skarbek M, Harris C, Meisner LF. A juvenile polyposis tumor suppressor locus at 10q22 is deleted from nonepithelial cells in the lamina propria. Gastroenterology 1997; 112: 1398–403.
Olschwang S, Serova-Sinilnikova OM, Lenoir GM, Gilles T. PTEN germ-line mutations in juvenile polyposis coli. Nat Genet 1998; 18: 12–14.
Liaw D, Marsh DJ, LiJ, et al. Germ-line mutations of the PTEN gene in Cowden’s disease, an inherited breast and thyroid cancer syndrome. Nat Genet 1997; 16: 64–7.
Marsh DJ, Dahia PLM, Coulon V, et al. Germ-line mutations in PTEN are present in Bannayan-Zonana syndrome. Nat Genet 1997; 16: 333–4.
Dahia PLM, Marsh DJ, Zheng Z, et al. Somatic deletions and mutations in the Cowden Disease gene, PTEN, in sporadic thyroid tumors. Cancer Res 1997; 57: 4710–13.
Howe JR, Roth S, Ringold JC, et al. Mutations in the SMAD4/DPC4 gene in juvenile polyposis. Science 1998; 280: 1086–8.
Jass JR, Williams CB, Bussay HJR, Morson BC. Juvenile polyposis-a precancerous condition. Histopathology 1988; 13: 619–30.
Bevan S, Woodford-Richens K, Rozen P, et al. Screening SMAD1, SMAD2, SMAD3 and SMAD5 for germline mutations in juvenile polyposis syndrome. Gut 1999; 45: 406–8.
Coburn MC, Pricolo VE, DeLuca FG, Bland KI. Malignant potential in intestinal juvenile polyposis syndromes. Ann Surg Oncol 1995; 2: 386–91.
Howe JR, Ringold JC, Hughes JH, Summers RW. Direct genetic testing for SMAD4 mutations in patients at risk for juvenile polyposis. Surgery 1999; 126: 162–70.
Peutz JLA. Very remarkable case of familial polyposis of mucous membrane of intestinal tract and nasopharynx accompanied by peculiar pigmentations of skin and mucous membrane. Nederl maandschr v geneesk 1921; 10: 134–46.
Jeghers H, McKusick VA, Katz KH. Generalized intestinal polyposis and melanin spots of the oral mucosa, lips and digits. N Engl J Med 1949; 241: 993–1005.
Guillem JG, Smith AJ, Puig-La Calle J, Ruo L. Hamartomatous polyposis. In: Wells SA, Creswell LL, eds. Gastrointestinal Polyposis Syndromes. St Louis: Mosby Inc, 1999: 286–99.
Hemminki A, Tomlinson I, Markie D, et al. Localization of a susceptibility locus for Peutz-Jegher’s syndrome to 19p using comparative genomic hybridization and targeted linkage analysis. Nat Genet 1997; 15: 87–90.
Wang ZJ, Ellis I, Zauber P. Allelic imbalance at the LKB1 (STK11) locus on 19p13.3 in hamartomas, adenomas and carcinomas from patients with Peutz-Jegher’s syndrome provides evidence for a hamartoma-(adenoma)-carcinoma sequence. J Pathol 1999; 188: 613–17.
Esteller M, Avizienyte E, Corn PG, et al. Epigenetic inactivation of LKB1 in primary tumors associated with the Peutz-Jeghers syndrome. Oncogene 2000; 19: 164–8.
Giardiello FM, Welsh SW, Hamilton SR, et al. Increased risk of cancer in the Peutz-Jeghers syndrome. N Engl J Med 1987; 316: 1511–14.
Spigelman AD, Murday V, Phillips RKS. Cancer and the Peutz-Jeghers syndrome. Gut 1989; 30: 1588–90.
Hizawa K, Iida M, Matsumoto T, et al. Cancer in Peutz-Jeghers syndrome. Cancer 1993; 72: 2777–81.
Reid JD. Intestinal carcinoma in the Peutz-Jeghers syndrome. JAMA 1974; 229: 833–4.
Spigelman AD, Arese P, Phillips RKS. Polyposis: the Peutz-Jeghers syndrome. Br J Surg 1995; 82: 1311–14.
Hoskins KF, Stopfer JE, Calzone KA, et al. Assessment and counseling for familial breast cancer risk: A guide for clinicians. JAMA 1995; 273: 577–85.
Lloyd KM II, Dennis M. Cowden’s disease: A possible new symptom complex with multiple system involvement. Ann Intern Med 1963; 58: 136–42.
Thyresson HN, Doyle JA. Cowden’s disease (multiple hamartoma syndrome). Mayo Clin Proc 1981; 56: 179–84.
Eng C. Cowden syndrome. J Genet Counseling 1997; 6: 181–91.
Marsh DJ, Kum JB, Lunetta KL, Bennett, et al. PTEN mutation spectrum and genotype-phenotype correlations in Bannayan-Riley-Ruvalcaba syndrome suggest a single entity with Cowden syndrome. Hum Mol Genet 1999; 8: 1461–72.
Nelen MR, Padberg GW, Peeters EAJ, et al. Localization of the gen for Cowden disease to chromosome 10q22–23. Nat Genet 1996; 13: 114–16.
Marsh DJ, Zheng Z, Zedenius J, et al. Differential loss of heterozygosity in the region of the Cowden locus within 10q22–23 in follicular thyroid adenomas and carcinomas. Cancer Res 1997; 57: 500–3.
Steck P, Perhouse M, Jasser SA, et al. Identification of a candidate suppressor gene MMAC1 at chromosome 10q22–23.3 that is mutated in multiple advanced cancers. Nat Genet 1997; 15: 356–62.
LiJ, Yen C, Liaw D, et al. PTEN, a putative protein tyrosine phosphatase gene mutated in human brain, breast and prostate cancer. Science 1997; 275: 1943–6.
Guldberg P, thor Straten P, Birck A, Ahrenkiel V, Kirkin AF, Zeuthen J. Disruption of the MMAC1/PTEN gene by deletion or mutation is a frequent event in malignant melanoma. Cancer Res 1997; 57: 3660–3.
Hanssen AMN, Fryns JP. Cowden syndrome. J Med Genet 1995; 32: 117–9.
Starink TM, van der Veen JPW, Arwert F de Waal LP, et al. The Cowden syndrome. A clinical and genetic study in 21 patients. Clin Genet 1986; 29: 222–33.
Longy M, Lacombe D. Cowden disease. Report of a family and review. Ann Genet 1996; 39: 35–42.
Ruvalcaba RH, Myhre S, Smith DW. Sotos syndrome with intestinal polyposis and pigmentary changes of the genitalia. Clin Genet 1980; 18: 413–6.
Gorlin RJ, Cohen MM Jr, Condon LM, Burke BA. Bannayan-Riley-Ruvalcaba syndrome. Am J Med Genet 1992; 44: 307–14.
Zigman AF, Lavine JE, Jones MC, Boland CR, Carethers JM. Localization of the Bannayan-Riley-Ruvalcaba syndrome gene to chromosome 10q23. Gastroenterology 1997; 113: 1433–7.
Carethers JM, Furnari FB, Zigman AF, et al. Absence of PTEN/MMAC1 germline mutations in sporadic Bannayan-Riley-Ruvalcaba syndrome. Cancer Res 1998; 58: 2724–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wirtzfeld, D.A., Petrelli, N.J. & Rodriguez-Bigas, M.A. Hamartomatous Polyposis Syndromes: Molecular Genetics, Neoplastic Risk, and Surveillance Recommendations. Ann Surg Oncol 8, 319–327 (2001). https://doi.org/10.1007/s10434-001-0319-7
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10434-001-0319-7