Abstract
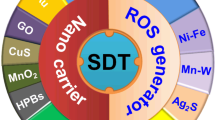
There is a tremendous need for prevention and effective treatment of cancer due to the associated morbidity and mortality. In this study, we introduce sonodynamic therapy (SDT), which is expected to be a new cancer treatment modality. SDT is a promising option for minimally invasive treatment of solid tumors and comprises three different components: sonosensitizers, ultrasound, and molecular oxygen. These components are harmless individually, but in combination they generate cytotoxic reactive oxygen species (ROS). We will explore the molecular mechanism by which SDT kills cancer cells, the class of sonosensitizers, drug delivery methods, and in vitro and in vivo studies. At the same time, we will highlight clinical applications for cancer treatment. The progress of SDT research suggests that it has the potential to become an advanced field of cancer treatment in clinical application. In this article, we will focus on the mechanism of action of SDT and its application to cancer treatment, and explain key factors to aid in developing strategies for future SDT development.




Similar content being viewed by others
Abbreviations
- SDT:
-
Sonodynamic therapy
- ROS:
-
Reactive oxygen species
- US:
-
Ultrasound
- PDT:
-
Photodynamic therapy
- HIFU:
-
High-intensity focused US
- SL:
-
Sonoluminescence
- O2 − :
-
Superoxides
- 1O2 :
-
Singlet oxygen
- ⋅OH:
-
Hydroxyl radicals:
- Hp:
-
Hematoporphyrin
- HMME:
-
Hematoporphyrin monomethyl ether
- PpIX:
-
Protoporphyrin IX
- Ce6:
-
Chlorine-e6
- 5-ALA:
-
5-Aminolevulinic acid
- EB:
-
Erythrosin B
- RB:
-
Rose bengal
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- TiO2 :
-
Titanium oxide
- SiO2 :
-
Silicon oxide
- EPR:
-
Enhanced permeation and retention
- DOX:
-
Doxorubicin
- CsA:
-
Cyclosporine A
- ADM:
-
Adriamycin
- SF1:
-
Sonoflora 1
- GcMAF:
-
Gc protein-derived macrophage-activating factor
References
Rosenthal I, Sostaric JZ, Riesz P. Sonodynamic therapy—a review of the synergistic effects of drugs and ultrasound. Ultrason Sonochem. 2004;11:349–63.
Kuroki M, Hachimine K, Abe H, et al. Sonodynamic therapy of cancer using novel sonosensitizers. Anticancer Res. 2007;27:3673–7.
Tachibana K, Feril LB Jr, Ikeda-Dantsuji Y. Sonodynamic therapy. Ultrasonics. 2008;48:253–9.
Trendowski M. The promise of sonodynamic therapy. Cancer Metastasis Rev. 2014;33:143–60.
Costley D, Mc Ewan C, Fowley C, et al. Treating cancer with sonodynamic therapy: a review. Int J Hyperth. 2015;31:107–17.
Liu XH, Li S, Wang M, et al. Current status and future perspectives of sonodynamic therapy and sonosensitiers. Asian Pac J Cancer Prev. 2015;16:4489–92.
McHale AP, Callan JF, Nomikou N, et al. Sonodynamic therapy: concept, mechanism and application to cancer treatment. Adv Exp Med Biol. 2016;880:429–50.
Zhang Q, Bao C, Cai X, et al. Sonodynamic therapy-assisted immunotherapy: a novel modality for cancer treatment. Cancer Sci. 2018;109:1330–45.
Lafond M, Yoshizawa S, Umemura S. Sonodynamic therapy: advances and challenges in clinical translation. J Ultrasound Med. 2019;38:567–80.
Liang S, Deng X, Ma P, et al. Recent advances in nanomaterial-assisted combinational sonodynamic cancer therapy. Adv Mater. 2020;32: e2003214.
Son S, Kim JH, Wang X, et al. Multifunctional sonosensitizers in sonodynamic cancer therapy. Chem Soc Rev. 2020;49:3244–61.
Choi V, Rajora MA, Zheng G. Activating drugs with sound: mechanisms behind sonodynamic therapy and the role of nanomedicine. Bioconjug Chem. 2020;31:967–89.
Xu M, Zhou L, Zheng L, et al. Sonodynamic therapy-derived multimodal synergistic cancer therapy. Cancer Lett. 2021;497:229–42.
Meng Q, Chen B, Wu W, et al. Enhanced antitumor effects of low-frequency ultrasound combined with adriamycin on human leukemia multidrug resistance cell line K562/A02. Chin J Cancer. 2008;27:436–9.
Miller MW, Luque AE, Battaglia LF, et al. Biological and environmental factors affecting ultrasound-induced hemolysis in vitro: 1. HIV macROSytosis. Ultrasound Med Biol. 2003;29:77–91.
Zhao Y, Lu C, Zhou Z, et al. Enhancing chemotherapeutic drug inhibition on tumor growth by ultrasound: an in vivo experiment. J Drug Target. 2011;19:154–60.
Bai W, Shen E, Hu B. Induction of the apoptosis of cancer cell by sonodynamic therapy: a review. Chin J Cancer Res. 2012;24:368–73.
Masui T, Ota I, Kanno M. Low-intensity ultrasound enhances the anticancer activity of cetuximab in human head and neck cancer cells. Exp Ther Med. 2013;5:11–6.
Wang P, Wang X, Liu Q. Cell damage of hepatoma-22 cells exposed to continuous wave ultrasound. Tumori. 2012;98:523–31.
Wang X, Liu Q, Wang Z. Bioeffects of low-energy continuous ultrasound on isolated sarcoma 180 cells. Chemotherapy. 2009;55:253–61.
Endo S, Kudo N, Yamaguchi S, et al. Porphyrin derivatives-mediated sonodynamic therapy for malignant gliomas in vitro. Ultrasound Med Biol. 2015;41:2458–65.
Jeong EJ, Seo SJ, Ahn YJ, et al. Sonodynamically induced antitumor effects of 5-aminolevulinic acid and fractionated ultrasound irradiation in all orthotopic rat glioma model. Ultrasound Med Biol. 2012;38:2143–50.
Yumita N, Nishigaki R, Umemura K, et al. Hematoporpbyrin as a sensitizer of cell-damaging effect of’ ultrasound. Jpn J Cancer Res. 1989;80:219–22.
Chen H, Zhou X, Gao Y, et al. Recent progress in development of new sonosensitizers for sonodynamic cancer therapy. Drug Discov Today. 2014;19:502–9.
Kessel D, Jeffers R, Fowlkes JB, et al. Porphyrin-induced enhancement of ultrasound cytotoxicity. Int J Radiat Biol. 1994;66:221–8.
Yumita N, Nishigaki R, Umemura K, et al. Synergistic effect of ultrasound and hematoporphyrin on sarcoma. Jpn J Cancer Res. 1990;81:304–8.
Umemura S, Yumita N, Nishigaki R, et al. Mechanism of cell damage by ultrasound in combination with hematoporphyrin. Jpn J Cancer Res. 1990;81:962–6.
Dubinsky TJ, Cuevas C, Dighe MK, et al. High-intensity focused ultrasound: current potential and oncologic applications. AJR Am J Roentgenol. 2008;190:191–9.
Hwang JH, Wang YN, Warren C, et al. Preclinical in vivo evaluation of an extracorporeal HIFU device for ablation of pancreatic tumors. Ultrasound Med Biol. 2009;35:967–75.
Sofuni A, Moriyasu F, Sano T, et al. The current potential of high-intensity focused ultrasound for pancreatic carcinoma. J Hepatobil Pancreat Sci. 2011;18:295–303.
Sofuni A, Moriyasu F, Sano T, et al. Safety trial of high-intensity focused ultrasound therapy for pancreatic cancer. World J Gastroenterol. 2014;20:9570–7.
Sofuni A, Asai Y, Tsuchiya T, et al. Novel therapeutic method for unresectable pancreatic cancer—the impact of the long-term research in therapeutic effect of high-intensity focused ultrasound (HIFU) therapy. Curr Oncol. 2021;28:4845–61.
Krasovitski B, Frenkel V, Shoham S, et al. Intramembrane cavitation as a unifying mechanism for ultrasound-induced bioeffects. Proc Natl Acad Sci USA. 2011;108:3258–63.
Riesz P, Berdahl D, Christman CL. Free radical generation by ultrasound in aqueous and nonaqueous solutions. Environ Health Perspect. 1985;64:233–52.
Umemura S, Kawabata K, Sasaki K. In vitro and in vivo enhancement of sonodynamically active cavitation by second-harmonic superimposition. J Acoust Soc Am. 1997;101:569–77.
Kessel D, Lo J, Jeffers R, et al. Modes of photodynamic vs sonodynamic cytotoxicity. J Photochem Photobiol B. 1995;28:219–21.
Pickworth M, Dendy P, Leighton T, et al. Studies of the cavitational effects of clinical ultrasound by sonoluminescence: 2. Thresholds for sonoluminescence from a therapeutic ultrasound beam and the effect of temperature and duty cycle. Phys Med Biol. 1988;33:1249–60.
Byun K, Kim KY, Kwak H. Sonoluminescence characteristics from micron and submicron bubbles. J Korean Phys Soc. 2005;47:1010–22.
Saksena T, Nyborg W. Sonoluminescence from stable cavitation. J Chem Phys. 1970;53:1722–34.
Hachiminc K, Shibaguchi H, Kuroki M, et al. Sonodynamic therapy of cancer using a novel porphyrin derivative. DCPH–P–Na(l), which is devoid of photosensitivity. Cancer Sci. 2007;98:916–20.
Lv Y, Fang M, Zheng J, et al. Low-intensity ultrasound combined with 5-aminolcvulinic acid administration in the treatment of human tongue squamous carcinoma. Cell Physiol Biochem. 2012;30:321–33.
Song W, Cui H, Zhang R, et al. Apoptosis of SAS cells induced by sonodynamic therapy using 5-aminolevulinic acid sonosensitizer. Anticancer Res. 2011;31:39–45.
Bhatia RP, Dhawan S, Khanna HD, et al. Indirect evaluation of corneal apoptosis in contact lens wearers by estimation of nitric oxide and antioxidant enzymes in tears. Oman J Ophthalmol. 2010;3:66–9.
Dai S, Xu C, Tian Y, et al. In vitro stimulation of calcium overload and apoptosis by sonodynamic therapy combined with hematoporphyrin monomethyl ether in C6 glioma cells. Oncol Lett. 2014;8:1675–81.
Su X, Wang P, Wang X, et al. Involvement of MAPK activation and ROS generation in human leukemia U937 cells undergoing apoptosis in response to sonodynamic therapy. Int J Radiat Bio. 2013;89:915–7.
Su XM, Wang P, Yang S, et al. Sonodynamic therapy induces the interplay between apoptosis and autophagy in K562 cells through ROS. Int J Biochem Cell Biol. 2015;60:82–92.
Zhao P, Liu Q, Wang P, et al. Autophagic and apoptotic response to sonodynamic therapy induced cell damage in leukemia I1210 cells in vitro. Cancer Biother Radiopharm. 2011;26:209–18.
Wang X, Liu Q, Wang Z, et al. Role of autophagy in sonodynamic therapy-induced cytotoxicity in S180 cells. Ultrasound Med Biol. 2010;36:1933–6.
Wang X, Xiong D, Wang J, et al. Investigation on damage of DNA molecules under irradiation of low frequency ultrasound in the presence of hematoporphyrin-gallium (HP-Ga) complex. Ultrason Sonochem. 2008;15:761–7.
Su X, Wang X, et al. ERK inhibitor U0126 enhanced SDT- induced cytotoxicity of human leukemia U937 cells. Gen Phys Biophys. 2014;33:295–9.
Dellinger M. Apoptosis or necrosis following Photofrin photosensitization: influence of the incubation protocol. Photochem Photobiol. 1996;64:182–7.
Oleinick NL, Morris RL, Belichenko I. The role of apoptosis in response to photodynamic therapy: what, where, why, and how. Photochem Photobiol Sci. 2002;1:1–21.
Castano AP, Mroz P, Hamblin MR. Photodynamic therapy and antitumour immunity. Nature Rev Cancer. 2006;6:535–45.
Kessel D, Vicente MGH, Reiners JJ. Initiation of apoptosis and autophagy by photodynamic therapy. Lasers Surg Med. 2006;38:482–8.
Kondo Y, Kanzawa T, Sawaya R, Kondo S. The role of autophagy in cancer development and response to therapy. Nature Rev Cancer. 2005;5:726–34.
Muragaki Y, Akimoto J, Maruyama T, et al. Phase II clinical study on intraoperative photodynamic therapy with talaporfin sodium and semiconductor laser in patients with malignant brain tumors. J Neurosurg. 2013;119:845–52.
Song D, Yue W, Li Z, et al. Study of the mechanism of sonodynamic therapy in a rat glioma model. Onco Targets Ther. 2014;7:1801–10.
Li L, Chen Y, Wang X, et al. Comparison of protoporphyrin IX produced cell proliferation inhibition between human breast cancer MCF-7 and MDA-MB-231 cells. Pharmazie. 2014;69:621–8.
Li Y, Wang P, Wang X, et al. Involvement of mitochondrial and reactive oxygen species in the sonodynamic toxicity of chlorin e6 in human leukumia K562 cells. Ultrasound Med Biol. 2014;40:990–1000.
Suzuki N, Okada K, Chida S, et al. Antitumor effect of acridine orange under ultrasonic irradiation in vitro. Anticancer Res. 2007;27:4179–84.
Komori C, Okada K, Kawamura K, et al. The sonodynamic antitumor effect of methylene blue on sarcoma180 cells in vitro. Anticancer Res. 2009;29:2411–5.
Urbanska K, Romanowska-Dixon B, Matuszak Z, et al. Indocyanine green as a prospective sensitizer for photodynamic therapy of melanomas. Acta Biochim Pol. 2002;49:387–91.
Nomikou N, Sterrett C, Arthur C, et al. The effects of ultrasound and light on indocyanine- green-treated tumour cells and tissues. Chem Med Chem. 2012;7:1465–71.
Ji C, Si J, Xu Y, et al. Mitochondria-targeted and ultrasound-responsive nanoparticles for oxygen and nitric oxide codelivery to reverse immunosuppression and enhance sonodynamic therapy for immune activation. Theranostics. 2021;11:8587–604.
Wu P, Dong W, Guo X, et al. ROS-responsive blended nanoparticles: cascade-amplifying synergistic effects of sonochemotherapy with on-demand boosted drug release during SDT PROSess. Adv Healthc Mater. 2019;8: e1900720.
Haibo C, Ye T. GW24-e0411 The sonodynamic effect of curcumin on THP-1 cell-derived macrophages. Heart. 2013;99:A22–3.
Zheng L, Sun X, Zhu X, et al. Apoptosis of THP–1 derived macrophages induced by sonodynamic therapy using a new sonosensitizer hydroxyl acetylated curcumin. PLoS One. 2014;9: e93133.
Liu JF. Non-steroidal anti-inflammatory drugs and cancer, with an especial focus on esophageal cancer. Asian Pac J Cancer Prev. 2011;12:3159–68.
Sakusabe N, Okada K, Sato K, et al. Enhanced sonodynamic antitumor effect of ultrasound in the presence of nonsteroidal anti-inflammatory drugs. Jpn J Cancer Res. 1999;90:1146–51.
Okada K, Itoi E, Nakajima M, et al. Enhance antitumor effect of ultrasound in the presence of piroxicam in a mouse air pouch model. Jpn J Cancer Res. 2002;93:216–22.
Daniele RG, Rolim CMB, Farooqi AA. Nanoparticle induced oxidative stress in cancer cells: adding new pieces to an incomplete jigsaw puzzle. Asian Pac J Cancer Prev. 2014;12:4739–43.
Ogi H, Hirao M, Shimoyama M. Activation of TiO2 photocatalyst by single–bubble sonoluminescence for water treatment. Ultrasonics. 2002;40:649–50.
Kubota Y, Shuin T, Kawasaki C, et al. Photokilling of T-24 human bladder cancer cells with titanium dioxide. Br J Cancer. 1994;70:1107–11.
You DG, Deepagan VG, Um W, et al. ROS-generating TiO2 nanoparticles for non-invasive sonodynamic therapy of cancer. Sci Rep. 2016;6:23200.
Ninomiya K, Noda K, Ogino C, et al. Enhanced OH radical generation by dual-frequency, ultrasound with TiO2 nanoparticles: its application to targeted sonodynamic therapy. Ultrason Sonochem. 2014;21:289–94.
Harada Y, Ogawa K, Irie Y, et al. Ultrasound activation of TiO2 in melanoma tumors. J Control Release. 2011;49:190–5.
Osmiiikina LA, Sivakov VA, Mysov GA, et al. Nanoparticles prepared from porous silicon nanowires for bio-imaging and sonodynamic therapy. Nanoscale Res Lett. 2014;9:463.
Shanei A, Sazgarnia A, Meibodi NT, et al. Sonodynamic therapy using protoporphyrin IX conjugated to gold nanoparticles: an in vivo study on a colon tumor model. Iran J Basic Med Sci. 2012;15:759–67.
Narang AS, Varia S. Role of tumor vascular architecture in drug delivery. Adv Drug Deliv Rev. 2011;63:640–58.
Torchilin V. Tumor delivery of macromolecular drugs based on the EPR effect. Adv Drug Deliv Rev. 2011;63:131–5.
Liang L, Xie S, Jiang L, et al. The combined effects of hematoporphyrin monomethyl ether-SDT and doxorubicin on the proliferation of QBC939 cell lines. Ultrasound Med Biol. 2013;39:146–60.
Yoshida T, Kondo T, Ogawa R, et al. Combination of doxorubicin and low–intensity ultrasound causes a synergistic enhancement in cell killing and all additive enhancement in apoptosis induction in human lymphoma U937 cells. Cancer Chemother Pharmacol. 2008;61:559–67.
Ren Y, Wang R, Liu Y, et al. A hematoporphyrin-based delivery system for drug resistance reversal and tumor ablation. Biomaterials. 2014;35:2462–70.
Yang H, Liu YH, Xu L, et al. Efficacy of permanent iodine-125 seed implants and gemcitabine chemotherapy in patients with platinum-resistant recurrent ovarian carcinoma. Asian Pac J Cancer Prev. 2014;20:9009–13.
Yu T, Yang Y, Liu S, et al. Ultrasound increases DNA damage attributable to cisplatin in cisplatin-resistant human ovarian cancer cells. Ultrasound Obstet Gynecol. 2009;33:355–9.
Gao HJ, Zhang WM, Wang XH, et al. Adriamycin enhances the sonodynamic effect of chlorin e6 against the proliferation of human breast cancer MDA-MB-231 cells in vitro. J Southern Med Uni. 2010;30:2291–4.
Yue W, Chen L, Yu L, et al. Checkpoint blockade and nanosonosensitizer-augmented noninvasive sonodynamic therapy combination reduces tumour growth and metastases in mice. Nat Commun. 2019;10:2025.
Horise Y, Maeda M, Konishi Y, et al. Sonodynamic therapy with anticancer micelles and high-intensity focused ultrasound in treatment of canine cancer. Front Pharmacol. 2019;21:545.
Yumita N, Sasaki K, Umemura S, et al. Sonodynamically induced antitumor effect of a gallium–porphyrin complex, ATX-70. Jpn J Cancer Res. 1996;87:310–6.
Yumita N, Okuyama N, Sasaki K, et al. Sonodynamic therapy on chemically induced mammary tumor: pharmacokinetics, tissue distribution and sonodynamically induced antitumor effect of gallium–porphyrin complex ATX–70. Cancer Chemother Pharmacol. 2007;60:891–7.
Yumita N, Okuyama N, Sasaki K, et al. Sonodynamic therapy on chemically induced mammary tumor: pharmacokinetics, tissue distribution and sonodynamically induced antitumor effect of porfimer sodium. Cancer Sci. 2004;95:765–9.
Wang X, Lewis TJ, Mitchell D. The tumoricidal effect of sonodynamic therapy (SDT) on S-180 sarcoma in mice. Integr Cancer Ther. 2008;7:96–102.
Xiong W, Wang P, Hu J, et al. A new sensitizer DVDMS combined with multiple focused ultrasound treatments: an effective antitumor strategy. Sci Rep. 2015;5:17485.
Wang H, Wang P, Li L, et al. Microbubbles enhance the antitumor effects of sinoporphyrin sodium mediated sonodynamic therapy both in vitro and in vivo. Int J Biol Sci. 2015;11:1401–9.
Liu Y, Wang P, Liu Q, et al. Sinoporphyrin sodium triggered sonophotodynamic effects on breast cancer both in vitro and in vivo. Ultrason Sonochem. 2016;31:437–48.
Hu Z, Fan H, Lv G, et al. 5-Aminolevulinic acid–mediated sonodynamic therapy induces anti-tumor effects in malignant melanoma via p53-miR-34a-Sirt1 axis. J Dermatol Sci. 2015;79:155–62.
Li Y, Zhou Q, Hu Z, et al. 5-Aminolevulinic acid-based sonodynamic therapy induces the apoptosis of osteosarcoma in mice. PLoS One. 2015;10: e0132074.
Shimamura Y, Tamatani D, Kuniyasu S, et al. 5-Aminolevulinic acid enhances ultrasound-mediated antitumor activity via mitochondrial oxidative damage in breast cancer. Anticancer Res. 2016;36:3607–12.
Osaki T, Yokoe I, Uto Y, et al. Bleomycin enhances the efficacy of sonodynamic therapy using aluminum phthalocyanine disulfonate. Ultrason Sonochem. 2016;28:161–8.
Osaki T, Ono M, Uto Y, et al. Sonodynamic therapy using 5-aminolevulinic acid enhances the efficacy of bleomycin. Ultrasonics. 2016;67:76–84.
Ju D, Yamaguchi F, Zhan G, et al. Hyperthermotherapy enhances antitumor effect of 5-aminolevulinic acid-mediated sonodynamic therapy with activation of caspase-dependent apoptotic pathway in human glioma. Tumour Biol. 2016;37:10415–26.
Wang X, Zhang W, Xu Z, et al. Sonodynamic and photodynamic therapy in advanced breast carcinoma: a report of 3 cases. Integr Cancer Ther. 2009;8:283–7.
Kenyon JN, Fulle RJ, Lewis TJ. Activated cancer therapy using light and ultrasound: a case series of sonodynamic photodynamic therapy in 115 patients over a 4-year period. Curr Drug Therapy. 2009;4:179–93.
Inui T, Makita K, Miura H, et al. Case report: a breast cancer patient treated with GcMAF, sonodynamic therapy and hormone therapy. Anticancer Res. 2014;34:4589–93.
Kisker O, Onizuka S, Becker CM, et al. Vitamin D binding protein–macrophage activating factor (DBP–MAF) inhibits angiogenesis and tumor growth in mice. Neoplasia. 2003;5:32–40.
Tachibana K. Molecular diagnosis and treatment using a new ultrasound contrast agent. Gan To Kagaku Ryoho. 2013;40:291.
Acknowledgements
We would like to thank Prof. Yoshihiro Muragaki at Tokyo Woman Medical University, Faculty of Advanced Techno-Surgery, and Prof. Shin Yoshizawa and Prof. Shinichiro Umemura at Tohoku University, Graduate School of Biomedical Engineering. We would like to also thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
Conceptualization, A.S.; data curation, A.S.; investigation, A.S.; supervision, T.I.; validation, A.T. and T.I.; writing—original draft, A.S.; writing—review and editing, A.S. All the authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Atsushi Sofuni and Takao Itoi declare that they have no conflicts of interest.
Ethical statements
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent was obtained from all the patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Sofuni, A., Itoi, T. Current status and future perspective of sonodynamic therapy for cancer. J Med Ultrasonics (2022). https://doi.org/10.1007/s10396-022-01263-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10396-022-01263-x