Abstract
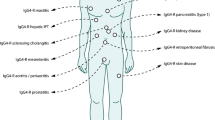
Autoimmune pancreatitis (AIP) is characterized by a tumefactive inflammatory lesion resembling pancreatic carcinoma. Type 1 AIP is a pancreatic manifestation of IgG4-related disease characterized by unique histological features that can be identified on imaging. The capsule-like rim, which is a collar of hypertrophic lesion surrounding the pancreas, consists of lymphoplasmacytic infiltration and fibrosis, and storiform fibrosis is often identified. Hypertrophic lesions of various microscopic architectures such as the ducts, veins (obliterative phlebitis), arteries (periarteritis), and nerves are observed without parenchymal damage. The pancreatic lobules keep their contours, but the acinar cells are diminished and replaced by numerous inflammatory cells. These features provide clues to arrive at a diagnosis of type 1 AIP and to distinguish it from pancreatic carcinoma on imaging. In contrast, type 2 AIP is an epithelium-centered inflammation involving the ducts and lobules. Neutrophilic infiltration in the epithelium and/or lumens (granulocytic epithelial lesion) is a characteristic finding. Lobular swelling due to inflammation is the cause of pancreatic enlargement. IgG4-related sclerosing cholangitis is histologically similar to the hypertrophic ductal lesion in type 1 AIP and characterized by wall thickening due to inflammation and luminal stenosis. The epithelium is intact, which is different from bile duct carcinomas and primary sclerosing cholangitis, the latter of which is characterized by inflammation targeting the epithelium. Although the histological features of type 1 AIP and IgG4-related sclerosing cholangitis are unique, the biopsy diagnosis of these diseases has limitations, which should be recognized by clinicians.





Similar content being viewed by others
References
Kawaguchi K, Koike M, Tsuruta K, Okamoto A, Tabata I, Fujita N. Lymphoplasmacytic sclerosing pancreatitis with cholangitis: a variant of primary sclerosing cholangitis extensively involving pancreas. Hum Pathol. 1991;22:387–95.
Yoshida K, Toki F, Takeuchi T, Watanabe S, Shiratori K, Hayashi N. Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci. 1995;40:1561–8.
Zamboni G, Luttges J, Capelli P, et al. Histopathological features of diagnostic and clinical relevance in autoimmune pancreatitis: a study on 53 resection specimens and 9 biopsy specimens. Virchows Arch. 2004;445:552–63.
Notohara K, Burgart LJ, Yadav D, Chari S, Smyrk TC. Idiopathic chronic pancreatitis with periductal lymphoplasmacytic infiltration: clinicopathologic features of 35 cases. Am J Surg Pathol. 2003;27:1119–27.
Deshpande V, Chicano S, Finkelberg D, et al. Autoimmune pancreatitis: a systemic immune complex mediated disease. Am J Surg Pathol. 2006;30:1537–45.
Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001;344:732–8.
Hamano H, Kawa S, Ochi Y, et al. Hydronephrosis associated with retroperitoneal fibrosis and sclerosing pancreatitis. Lancet. 2002;359:1403–4.
Zhang L, Notohara K, Levy MJ, Chari ST, Smyrk TC. IgG4-positive plasma cell infiltration in the diagnosis of autoimmune pancreatitis. Mod Pathol. 2007;20:23–8.
Sah RP, Chari ST, Pannala R, et al. Differences in clinical profile and relapse rate of type 1 versus type 2 autoimmune pancreatitis. Gastroenterology. 2010;139:140–8.
Kamisawa T, Chari ST, Giday SA, et al. Clinical profile of autoimmune pancreatitis and its histological subtypes: an international multicenter survey. Pancreas. 2011;40:809–14.
Deshpande V, Gupta R, Sainani N, et al. Subclassification of autoimmune pancreatitis: a histologic classification with clinical significance. Am J Surg Pathol. 2011;35:26–35.
Detlefsen S, Zamboni G, Frulloni L, et al. Clinical features and relapse rates after surgery in type 1 autoimmune pancreatitis differ from type 2: a study of 114 surgically treated European patients. Pancreatology. 2012;12:276–83.
Song TJ, Kim JH, Kim MH, et al. Comparison of clinical findings between histologically confirmed type 1 and type 2 autoimmune pancreatitis. J Gastroenterol Hepatol. 2012;27:700–8.
Kamisawa T, Chari ST, Lerch MM, Kim MH, Gress TM, Shimosegawa T. Recent advances in autoimmune pancreatitis: type 1 and type 2. Gut. 2013;62:1373–80.
Hart PA, Kamisawa T, Brugge WR, et al. Long-term outcomes of autoimmune pancreatitis: a multicentre, international analysis. Gut. 2013;62:1771–6.
Hart PA, Zen Y, Chari ST. Recent advances in autoimmune pancreatitis. Gastroenterology. 2015;149:39–51.
Notohara K, Nishimori I, Mizuno N, et al. Clinicopathological features of type 2 autoimmune pancreatitis in Japan: results of a multicenter survey. Pancreas. 2015;44:1072–7.
Hart PA, Levy MJ, Smyrk TC, et al. Clinical profiles and outcomes in idiopathic duct-centric chronic pancreatitis (type 2 autoimmune pancreatitis): the Mayo Clinic experience. Gut. 2016;65:1702–9.
Chari ST, Kloeppel G, Zhang L, Notohara K, Lerch MM, Shimosegawa T. Histopathologic and clinical subtypes of autoimmune pancreatitis: the Honolulu consensus document. Pancreas. 2010;39:549–54.
Shimosegawa T, Chari ST, Frulloni L, et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas. 2011;40:352–8.
Kitagawa S, Zen Y, Harada K, et al. Abundant IgG4-positive plasma cell infiltration characterizes chronic sclerosing sialadenitis (Kuttner’s tumor). Am J Surg Pathol. 2005;29:783–91.
Kasashima S, Zen Y, Kawashima A, et al. Inflammatory abdominal aortic aneurysm: close relationship to IgG4-related periaortitis. Am J Surg Pathol. 2008;32:197–204.
Zen Y, Onodera M, Inoue D, et al. Retroperitoneal fibrosis: a clinicopathologic study with respect to immunoglobulin G4. Am J Surg Pathol. 2009;33:1833–9.
Zen Y, Harada K, Sasaki M, et al. IgG4-related sclerosing cholangitis with and without hepatic inflammatory pseudotumor, and sclerosing pancreatitis-associated sclerosing cholangitis: do they belong to a spectrum of sclerosing pancreatitis? Am J Surg Pathol. 2004;28:1193–203.
Bartholomew LG, Cain JC, Woolner LB, Utz DC, Ferris DO. Sclerosing cholangitis: its possible association with Riedel’s struma and fibrous retroperitonitis. Report of two cases. N Engl J Med. 1963;269:8–12.
Comings DE, Skubi KB, Van Eyes J, Motulsky AG. Familial multifocal fibrosclerosis. Findings suggesting that retroperitoneal fibrosis, mediastinal fibrosis, sclerosing cholangitis, Riedel’s thyroiditis, and pseudotumor of the orbit may be different manifestations of a single disease. Ann Intern Med. 1967;66:884–92.
Laitt RD, Hubscher SG, Buckels JA, Darby S, Elias E. Sclerosing cholangitis associated with multifocal fibrosis: a case report. Gut. 1992;33:1430–2.
Kamisawa T, Funata N, Hayashi Y, et al. Close relationship between autoimmune pancreatitis and multifocal fibrosclerosis. Gut. 2003;52:683–7.
Stone JH, Khosroshahi A, Deshpande V, et al. Recommendations for the nomenclature of IgG4-related disease and its individual organ system manifestations. Arthritis Rheum. 2012;64:3061–7.
Uchida K, Okazaki K. Clinical and pathophysiological aspects of type 1 autoimmune pancreatitis. J Gastroenterol. 2018;53:475–83.
Hart PA, Topazian MD, Witzig TE, et al. Treatment of relapsing autoimmune pancreatitis with immunomodulators and rituximab: the Mayo Clinic experience. Gut. 2013;62:1607–15.
Mattoo H, Mahajan VS, Della-Torre E, et al. De novo oligoclonal expansions of circulating plasmablasts in active and relapsing IgG4-related disease. J Allergy Clin Immunol. 2014;134:679–87.
Kino-Ohsaki J, Nishimori I, Morita M, et al. Serum antibodies to carbonic anhydrase I and II in patients with idiopathic chronic pancreatitis and Sjogren’s syndrome. Gastroenterology. 1996;110:1579–86.
Nishimori I, Miyaji E, Morimoto K, Nagao K, Kamada M, Onishi S. Serum antibodies to carbonic anhydrase IV in patients with autoimmune pancreatitis. Gut. 2005;54:274–81.
Uchida K, Okazaki K, Konishi Y, et al. Clinical analysis of autoimmune-related pancreatitis. Am J Gastroenterol. 2000;95:2788–94.
Asada M, Nishio A, Uchida K, et al. Identification of a novel autoantibody against pancreatic secretory trypsin inhibitor in patients with autoimmune pancreatitis. Pancreas. 2006;33:20–6.
Lohr JM, Faissner R, Koczan D, et al. Autoantibodies against the exocrine pancreas in autoimmune pancreatitis: gene and protein expression profiling and immunoassays identify pancreatic enzymes as a major target of the inflammatory process. Am J Gastroenterol. 2010;105:2060–71.
Endo T, Takizawa S, Tanaka S, et al. Amylase alpha-2A autoantibodies: novel marker of autoimmune pancreatitis and fulminant type 1 diabetes. Diabetes. 2009;58:732–7.
Takizawa S, Endo T, Wanjia X, Tanaka S, Takahashi M, Kobayashi T. HSP 10 is a new autoantigen in both autoimmune pancreatitis and fulminant type 1 diabetes. Biochem Biophys Res Commun. 2009;386:192–6.
Frulloni L, Lunardi C, Simone R, et al. Identification of a novel antibody associated with autoimmune pancreatitis. N Engl J Med. 2009;361:2135–42.
Culver EL, Smit WL, Evans C, et al. No evidence to support a role for Helicobacter pylori infection and plasminogen binding protein in autoimmune pancreatitis and IgG4-related disease in a UK cohort. Pancreatology. 2017;17:395–402.
Hubers LM, Vos H, Schuurman AR, et al. Annexin A11 is targeted by IgG4 and IgG1 autoantibodies in IgG4-related disease. Gut. 2018;67:728–35.
Perugino CA, AlSalem SB, Mattoo H, et al. Identification of galectin-3 as an autoantigen in patients with IgG4-related disease. J Allergy Clin Immunol. 2019;143:736–45.
Shiokawa M, Kodama Y, Kuriyama K, et al. Pathogenicity of IgG in patients with IgG4-related disease. Gut. 2016;65:1322–32.
Shiokawa M, Kodama Y, Sekiguchi K, et al. Laminin 511 is a target antigen in autoimmune pancreatitis. Sci Transl Med. 2018;10:eaaq0997.
Zhang L, Chari S, Smyrk TC, et al. Autoimmune pancreatitis (AIP) type 1 and type 2: an international consensus study on histopathologic diagnostic criteria. Pancreas. 2011;40:1172–9.
Deshpande V, Zen Y, Chan JK, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25:1181–92.
Kawa S, Kamisawa T, Notohara K, et al. Japanese clinical diagnostic criteria for autoimmune pancreatitis, 2018: revision of Japanese clinical diagnostic criteria for autoimmune pancreatitis, 2011. Pancreas. 2020;49:e13–4.
Suda K, Takase M, Fukumura Y, Kashiwagi S. Pathology of autoimmune pancreatitis and tumor-forming pancreatitis. J Gastroenterol. 2007;42:22–7.
Dhall D, Suriawinata AA, Tang LH, Shia J, Klimstra DS. Use of immunohistochemistry for IgG4 in the distinction of autoimmune pancreatitis from peritumoral pancreatitis. Hum Pathol. 2010;41:643–52.
Fukui Y, Uchida K, Sumimoto K, et al. The similarity of Type 1 autoimmune pancreatitis to pancreatic ductal adenocarcinoma with significant IgG4-positive plasma cell infiltration. J Gastroenterol. 2013;48:751–61.
Ikeura T, Miyoshi H, Uchida K, et al. Relationship between autoimmune pancreatitis and pancreatic cancer: a single-center experience. Pancreatology. 2014;14:373–9.
Resheq YJ, Quaas A, von Renteln D, Schramm C, Lohse AW, Lüth S. Infiltration of peritumoural but tumour-free parenchyma with IgG4-positive plasma cells in hilar cholangiocarcinoma and pancreatic adenocarcinoma. Dig Liver Dis. 2013;45:859–65.
Uehara T, Hamano H, Kawa S, et al. Comparison of histopathological features of pancreatic carcinoma and type 1 autoimmune pancreatitis. Pathol Int. 2014;64:51–7.
Notohara K, Kamisawa T, Fukushima N, et al. Guidance for diagnosing autoimmune pancreatitis with biopsy tissues. Pathol Int. 2020;70:699–711.
Chan SK, Cheuk W, Chan KT, Chan JK. IgG4-related sclerosing pachymeningitis: a previously unrecognized form of central nervous system involvement in IgG4-related sclerosing disease. Am J Surg Pathol. 2009;33:1249–52.
Watanabe T, Fujinaga Y, Kawakami S, et al. Infraorbital nerve swelling associated with autoimmune pancreatitis. Jpn J Radiol. 2011;29:194–201.
Sogabe Y, Miyatani K, Goto R, Ishii G, Ohshima K, Sato Y. Pathological findings of infraorbital nerve enlargement in IgG4-related ophthalmic disease. Jpn J Ophthalmol. 2012;56:511–4.
Goto H, Takahira M, Azumi A. Diagnostic criteria for IgG4-related ophthalmic disease. Jpn J Ophthalmol. 2015;59:1–7.
Inoue D, Zen Y, Abo H, et al. Immunoglobulin G4-related periaortitis and periarteritis: CT findings in 17 patients. Radiology. 2011;261:625–33.
Irie H, Honda H, Baba S, et al. Autoimmune pancreatitis: CT and MR characteristics. AJR Am J Roentgenol. 1998;170:1323–7.
Takahashi M, Fujinaga Y, Notohara K, et al. Diagnostic imaging guide for autoimmune pancreatitis. Jpn J Radiol. 2020;38:591–612.
Miyabe K, Notohara K, Nakazawa T, et al. Histological evaluation of obliterative phlebitis for the diagnosis of autoimmune pancreatitis. J Gastroenterol. 2014;49:715–26.
Basturk O, Hong SM, Wood LD, et al. A Revised classification system and recommendations from the Baltimore consensus meeting for neoplastic precursor lesions in the pancreas. Am J Surg Pathol. 2015;39:1730–41.
Song JE, Han J, Kim HG, Kim MH, Hong SM. Type 1 autoimmune pancreatitis with histologically proven granulocytic epithelial lesions. Pancreatology. 2015;15:305–7.
Deshpande V, Mino-Kenudson M, Brugge WR, et al. Endoscopic ultrasound guided fine needle aspiration biopsy of autoimmune pancreatitis: diagnostic criteria and pitfalls. Am J Surg Pathol. 2005;29:1464–71.
Holmes BJ, Hruban RH, Wolfgang CL, Ali SZ. Fine needle aspirate of autoimmune pancreatitis (lymphoplasmacytic sclerosing pancreatitis): cytomorphologic characteristics and clinical correlates. Acta Cytol. 2012;56:228–32.
Cai G, Bernstein J, Aslanian HR, Hui P, Chhieng D. Endoscopic ultrasound-guided fine-needle aspiration biopsy of autoimmune pancreatitis: diagnostic clues and pitfalls. J Am Soc Cytopathol. 2015;4:211–7.
Maruyama M, Arakura N, Ozaki Y, et al. Type 1 autoimmune pancreatitis can transform into chronic pancreatitis: a long-term follow-up study of 73 Japanese patients. Int J Rheumatol. 2013;2013:272595.
Kuraishi Y, Uehara T, Watanabe T, et al. Corticosteroids prevent the progression of autoimmune pancreatitis to chronic pancreatitis. Pancreatology. 2020;20:1062–8.
Mizuno N, Bhatia V, Hosoda W, et al. Histological diagnosis of autoimmune pancreatitis using EUS-guided trucut biopsy: a comparison study with EUS-FNA. J Gastroenterol. 2009;44:742–50.
Imai K, Matsubayashi H, Fukutomi A, Uesaka K, Sasaki K, Ono H. Endoscopic ultrasonography-guided fine needle aspiration biopsy using 22-gauge needle in diagnosis of autoimmune pancreatitis. Dig Liver Dis. 2011;43:869–74.
Levy MJ, Reddy RP, Wiersema MJ, et al. EUS-guided trucut biopsy in establishing autoimmune pancreatitis as the cause of obstructive jaundice. Gastrointest Endosc. 2005;61:467–72.
Iwashita T, Yasuda I, Doi S, et al. Use of samples from endoscopic ultrasound-guided 19-gauge fine-needle aspiration in diagnosis of autoimmune pancreatitis. Clin Gastroenterol Hepatol. 2012;10:316–22.
Kanno A, Ishida K, Hamada S, et al. Diagnosis of autoimmune pancreatitis by EUS-FNA by using a 22-gauge needle based on the International Consensus Diagnostic Criteria. Gastrointest Endosc. 2012;76:594–602.
Ishikawa T, Itoh A, Kawashima H, et al. Endoscopic ultrasound-guided fine needle aspiration in the differentiation of type 1 and type 2 autoimmune pancreatitis. World J Gastroenterol. 2012;18:3883–8.
Yamashita H, Naitoh I, Nakazawa T, et al. A comparison of the diagnostic efficacy in type 1 autoimmune pancreatitis based on biopsy specimens from various organs. Pancreatology. 2014;14:186–92.
Morishima T, Kawashima H, Ohno E, et al. Prospective multicenter study on the usefulness of EUS-guided FNA biopsy for the diagnosis of autoimmune pancreatitis. Gastrointest Endosc. 2016;84:241–8.
Kanno A, Masamune A, Fujishima F, et al. Diagnosis of autoimmune pancreatitis by EUS-guided FNA using a 22-gauge needle: a prospective multicenter study. Gastrointest Endosc. 2016;84:797–804.
Notohara K, Kamisawa T, Kanno A, et al. Efficacy and limitations of the histological diagnosis of type 1 autoimmune pancreatitis with endoscopic ultrasound-guided fine needle biopsy with large tissue amounts. Pancreatology. 2020;20:834–43.
Detlefsen S, Joergensen MT, Mortensen MB. Microscopic findings in EUS-guided fine needle (SharkCore) biopsies with type 1 and type 2 autoimmune pancreatitis. Pathol Int. 2017;67:514–20.
Kurita A, Yasukawa S, Zen Y, et al. Comparison of a 22-gauge Franseen-tip needle with a 20-gauge forward-bevel needle for the diagnosis of type 1 autoimmune pancreatitis: a prospective, randomized, controlled, multicenter study (COMPAS study). Gastrointest Endosc. 2020;91:373–81.
Ishikawa T, Kawashima H, Ohno E, et al. Usefulness of endoscopic ultrasound-guided fine-needle biopsy for the diagnosis of autoimmune pancreatitis using a 22-gauge Franseen needle: a prospective multicenter study. Endoscopy. 2020;52:978–85.
Fukui T, Mitsuyama T, Takaoka M, Uchida K, Matsushita M, Okazaki K. Pancreatic cancer associated with autoimmune pancreatitis in remission. Intern Med. 2008;47:151–5.
Witkiewicz AK, Kennedy EP, Kennyon L, Yeo CJ, Hruban RH. Synchronous autoimmune pancreatitis and infiltrating pancreatic ductal adenocarcinoma: case report and review of the literature. Hum Pathol. 2008;39:1548–51.
Motosugi U, Ichikawa T, Yamaguchi H, et al. Small invasive ductal adenocarcinoma of the pancreas associated with lymphoplasmacytic sclerosing pancreatitis. Pathol Int. 2009;59:744–7.
Zhang X, Liu X, Joseph L, Zhao L, Hart J, Xiao SY. Pancreatic ductal adenocarcinoma with autoimmune pancreatitis-like histologic and immunohistochemical features. Hum Pathol. 2014;45:621–7.
Takano Y, Nagahama M, Yamamura E, et al. A case of concurrent pancreatic intraepithelial neoplasia and type 1 autoimmune pancreatitis with marked pancreatic duct dilatation. Clin J Gastroenterol. 2016;9:266–71.
Sugiyama T, Tajiri T, Hiraiwa S, et al. A case of high-grade pancreatic intraepithelial neoplasia concomitant with type 1 autoimmune pancreatitis: the process underlying both conditions. Pathol Int. 2019;69:165–71.
Naitoh I, Nakazawa T, Notohara K, et al. Intraductal papillary mucinous neoplasm associated with autoimmune pancreatitis. Pancreas. 2013;42:552–4.
Urata T, Naito Y, Izumi Y, et al. Localized type 1 autoimmune pancreatitis superimposed upon preexisting intraductal papillary mucinous neoplasms. World J Gastroenterol. 2013;19:9127–32.
Bateman AC, Culver EL, Sommerlad M, Chetty R. Intraduct papillary mucinous neoplasm of the pancreas: a tumour linked with IgG4-related disease? J Clin Pathol. 2013;66:671–5.
Tabata T, Kamisawa T, Hara S, et al. Intraductal papillary mucinous neoplasm of the pancreas and IgG4-related disease: a coincidental association. Pancreatology. 2013;13:379–83.
Vaquero EC, Salcedo MT, Cuatrecasas M, et al. Autoimmune pancreatitis type-1 associated with intraduct papillary mucinous neoplasm: report of two cases. Pancreatology. 2014;14:316–8.
Hedayat AA, Lisovsky M, Suriawinata AA, Longnecker DS. Association of IgG4 response and autoimmune pancreatitis with intraductal papillary-mucinous neoplasms. Pancreatology. 2017;17:263–6.
Koshita S, Noda Y, Ito K, et al. Branch duct intraductal papillary mucinous neoplasms of the pancreas involving type 1 localized autoimmune pancreatitis with normal serum IgG4 levels successfully diagnosed by endoscopic ultrasound-guided fine-needle aspiration and treated without pancreatic surgery. Intern Med. 2017;56:1163–7.
Suzuki R, Okada R, Muto M, et al. Rare coincidence of intraductal papillary mucinous neoplasm and type 1 autoimmune pancreatitis. Clin J Gastroenterol. 2020;13:1315–21.
Yakirevich E, Henriksen KJ, Miner T, Resnick MB. Mucinous cystic neoplasm of the pancreas with increased IgG4+ plasma cells and histopathologic features of autoimmune pancreatitis/IgG4-related disease. Pancreas. 2015;44:674–6.
Kim MJ, Song TJ, Kim HJ, Kim SC, Kim MH, Hong SM. Coexisting mucinous cystic neoplasm of the pancreas and type 1 autoimmune pancreatitis. J Pathol Transl Med. 2019;53:125–8.
Hatano Y, Kawashima K, Iwashita T, Kimura M, Shimizu M, Hara A. A Solid pseudopapillary neoplasm of the pancreas associated with IgG4-related pancreatitis: a case report. Int J Surg Pathol. 2017;25:271–5.
Matsumori T, Shiokawa M, Kodama Y. Pancreatic mass in a patient with an increased serum level of IgG4. Gastroenterology. 2018;155:269–70.
Shiokawa M, Kodama Y, Yoshimura K, et al. Risk of cancer in patients with autoimmune pancreatitis. Am J Gastroenterol. 2013;108:610–7.
Kloppel G, Detlefsen S, Chari ST, Longnecker DS, Zamboni G. Autoimmune pancreatitis: the clinicopathological characteristics of the subtype with granulocytic epithelial lesions. J Gastroenterol. 2010;45:787–93.
Ku Y, Hong SM, Fujikura K, et al. IL-8 expression in granulocytic epithelial lesions of idiopathic duct-centric pancreatitis (type 2 autoimmune pancreatitis). Am J Surg Pathol. 2017;41:1129–38.
Gupta R, Neyaz A, Chougule A, et al. Autoimmune pancreatitis type 2: diagnostic utility of PD-L1 immunohistochemistry. Am J Surg Pathol. 2019;43:898–906.
Nakazawa T, Ohara H, Yamada T, et al. Atypical primary sclerosing cholangitis cases associated with unusual pancreatitis. Hepatogastroenterology. 2001;48:625–30.
Uehara T, Hamano H, Kawa S, Sano K, Honda T, Ota H. Distinct clinicopathological entity ‘autoimmune pancreatitis-associated sclerosing cholangitis.’ Pathol Int. 2005;55:405–11.
Graham RP, Smyrk TC, Chari ST, Takahashi N, Zhang L. Isolated IgG4-related sclerosing cholangitis: a report of 9 cases. Hum Pathol. 2014;45:1722–9.
Nakazawa T, Ohara H, Sano H, Ando T, Joh T. Schematic classification of sclerosing cholangitis with autoimmune pancreatitis by cholangiography. Pancreas. 2006;32:229.
Kamisawa T, Nakazawa T, Tazuma S, et al. Clinical practice guidelines for IgG4-related sclerosing cholangitis. J Hepatobiliary Pancreat Sci. 2019;26:9-42.
Nakazawa T, Kamisawa T, Okazaki K, et al. Clinical diagnostic criteria for IgG4-related sclerosing cholangitis 2020: (Revision of the clinical diagnostic criteria for IgG4-related sclerosing cholangitis 2012). J Hepatobiliary Pancreat Sci. 2021;28:235–42.
Naitoh I, Zen Y, Nakazawa T, et al. Small bile duct involvement in IgG4-related sclerosing cholangitis: liver biopsy and cholangiography correlation. J Gastroenterol. 2011;46:269–76.
Ishigami K, Shitani M, Kimura Y, et al. Ectopic relapse of IgG4-related disease presenting as IgG4-related sclerosing cholecystitis: a case report and review of literature. Medicine. 2018;97:e13868.
Hong SA, Sung YN, Kim HJ, et al. Xanthogranulomatous cholecystitis shows overlapping histological features with IgG4-related cholecystitis. Histopathology. 2018;72:569–79.
Gupta RK, Patton KT. Hyalinizing cholecystitis with features of immunoglobulin G4-related disease-coincidence or an unrecognized association? A case report. Hum Pathol. 2015;46:625–8.
Zhang L, Lewis JT, Abraham SC, et al. IgG4+ plasma cell infiltrates in liver explants with primary sclerosing cholangitis. Am J Surg Pathol. 2010;34:88–94.
Zen Y, Quaglia A, Portmann B. Immunoglobulin G4-positive plasma cell infiltration in explanted livers for primary sclerosing cholangitis. Histopathology. 2011;58:414–22.
Nishino T, Oyama H, Hashimoto E, et al. Clinicopathological differentiation between sclerosing cholangitis with autoimmune pancreatitis and primary sclerosing cholangitis. J Gastroenterol. 2007;42:550–9.
Deshpande V, Sainani NI, Chung RT, et al. IgG4-associated cholangitis: a comparative histological and immunophenotypic study with primary sclerosing cholangitis on liver biopsy material. Mod Pathol. 2009;22:1287–95.
Acknowledgements
I thank Dr. Etsuji Ishida, Department of Gastroenterology and Hepatology, Kurashiki Central Hospital, for offering the figures of imaging tests. This work was supported by MHLW Research Program on Rare and Intractable Diseases Grant Number JPMH20FC1040.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author has no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
This is a review article, and approval by the ethical review board is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Notohara, K. Histological features of autoimmune pancreatitis and IgG4-related sclerosing cholangitis with a correlation with imaging findings. J Med Ultrasonics 48, 581–594 (2021). https://doi.org/10.1007/s10396-021-01148-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-021-01148-5