Abstract
Purpose
To investigate the incidence rate and side effects of topical atropine sulfate and cyclopentolate hydrochloride for cycloplegia in children aged 15 years or under.
Methods
This prospective study had been conducted at 9 institutions between April 1, 2016 and March 31, 2017 in patients 15 years old or younger who received either atropine or cyclopentolate for refraction assessment. The investigation included patient’s age, symptoms, and whether patients with side effects had any systemic diseases.
Results
A total of 811 patients (mean age ± SD, 4.6 ± 2.2 years) received atropine and 71 (8.8%) patients had side effects. Except in patients under two years old, 1% eye drops showed higher incidence rate of side effects than 0.5% and 0.25% eye drops. Side effects most frequently occurred following the initiation of the instillation on the first day. The symptoms included flush (29/71, 40.8%), fever (21/71, 30.0%), and both (11/71, 15.5%). A total of 2238 patients (5.7 ± 3.0 years) used cyclopentolate and 27 (1.2%) (4.0 ± 2.2 years) patients had side effects. The symptoms included drowsiness (10/27, 37.0%), red eye (4/27, 14.8%), fever (3/27, 11.1%), and flush (3/27, 11.1%).
Conclusions
Atropine has a side effect incidence rate 7 times higher than the incidence rate of cyclopentolate. Flush and fever are the most common side effects of atropine and drowsiness is the main side effect of cyclopentolate. These findings should be noted when examining cycloplegic refraction to manage amblyopia and strabismus in children.
Similar content being viewed by others
Introduction
Cycloplegic refraction is indispensable for managing amblyopia and strabismus in children. In Japan, the main cycloplegic agents used are topical atropine and cyclopentolate eye drops. Choice of cycloplegic agent, level of concentration, and frequency of instillation can all vary among institutions and yet, no nationwide investigation on the side effects and incidence of the side effects of accommodative cycloplegic eye drops has been conducted.
In a previous study, we have used a questionnaire to conduct a nationwide survey of the current situation of cycloplegic eye drops use and the side effects in children aged 15 years or younger. The questionnaire was sent to 178 institutions with which the directors of the Japanese Association for Strabismus and Amblyopia (JASA) and JASA-listed ophthalmologists with subspecialties of strabismus and amblyopia are affiliated [1]. The questionnaire results showed that most institutions use atropine of concentrations of 0.5% or 1.00% twice a day for 7 days. Cyclopentolate is instilled twice with a 5-minute interval and refraction examination is performed 60 minutes after the instillation. Many of the ophthalmologists had patients showing side effects of accommodative cycloplegic eye drops. In 84.5% of the institutions patients had fever and flush, following instillation of atropine, and in 55.2% of the institutions patients felt drowsiness and hallucinations after receiving cyclopentolate. The risk of side effects appears to be the main concern for ophthalmologists when using accommodative cycloplegic eye drops.
Studies on the side effects of atropine and cyclopentolate have been carried out by individual facilities [2,3,4,5,6,7,8,9]. To our knowledge, no multi-center investigation has been conducted. For safer clinical use of accommodative cycloplegic eye drops, this study aimed to investigate the side effects of atropine and cyclopentolate and the incidence rates of the side effects in children 15 years old or younger on a national wide level.
Patients and methods
Approved by the Ethics Committee of each institution and adhered to the tenets of the Declaration of Helsinki, this prospective study was conducted by 9 institutions between April 1, 2016 and March 31, 2017. Subjects were children 15 years old or younger who received atropine or cyclopentolate for refraction assessment. The investigation included gender and age at the time of use for all the patients; and age, gender, symptoms, with or without systemic diseases for those with side effects. In the patients receiving atropine, the concentration of the eye drops, the interval between the initiation of the eye drops, and the occurrence of side effects were also investigated. Every month, the participating institutions sent the results of the investigation to Kindai University Faculty of Medicine.
Results
Atropine
Patient’s gender and concentration levels of eye drops
A total of 811 patients (age range, 2 months to 14.1 years; mean age ± SD, 4.6 ± 2.2 years) used atropine. Of 811, 387 (47.7%) were boys and 424 (52.3%) were girls. Table 1 shows the concentration levels and patient’s age at the time of atropine use. Eye drops of higher concentrations tended to be used for elder patients. Of 9, ophthalmologists at 6 institutions instilled atropine twice a day for 7 days and at 3 institutions instilled twice a day for 5 days. The lacrimal sac was pressed in all the patients following atropine instillation. Atropine eye ointment was used in 3 of the 9 institutions.
Incidence rate of side effects
Of 811, 71 (8.8%; mean age, 4.3 ± 2.2 years) patients including 30 (42.3%) boys and 41 (57.7%) girls had side effects. During the year, the period of May through September had a higher incidence rate than the overall rate of 8.8%. Within that period, July, September, and June had the top highest incidence rates (Fig. 1). The period between the initiation of the instillation and the time when the side effect occurred was: 1 day (37/69, 53.6%), 2-3 days (19/69, 27.5%), and 4 days or longer (13/69, 18.9%). Of 71 patients, 2 were not clear about the time when the side effect had occurred.
Association of side effect incidence rate with concentration level and age
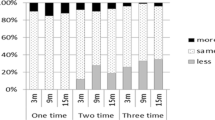
Among the 3 concentration levels, 1% eye drops had the highest incidence rate of side effects (49/391, 12.5%), followed by 0.25% eye drops (6/80, 7.5%) and 0.5% eye drops (16/329, 4.9%). No patients using 1.0% eye ointment had any side effects. Table 2 shows the age-specific incidence rates of side effects. Patients under one-year old had the highest incidence rate (5/26, 19.2%) and patients between 2-3 years old had the lowest incidence rate (6/93, 6.5%). In all the patients except those under two years of age, 1% eye drops showed a higher incidence rate of side effects than 0.5% and 0.25% eye drops (Fig. 2).
Association of side effect incidence rate with concentration level and age (n = 811). a < 1 year old (n = 26). b 1-2 years old (n = 67). c 2-3 years old (n = 93). d 3-4 years old (n = 142). e 4-5 years old (n = 156). f 5-6 years old (n = 118). g 6-15 years old (n = 209). Eye drops of 1% showed a higher incidence rate of side effects than 0.5% and 0.25% eye drops in all the patients. □ rate of patients using atropine at the concentration level. ■ side effect rate
Side effects and systemic diseases
The side effects of atropine included flush (29/71, 40.8%), fever (21/71, 30.0%), and both (11/71, 15.5%), (Fig. 3). The eye drops with the highest concentration (1%) showed side effects including fever (20/49, 40.8%), flush (17/49, 34.7%), and both (8/49, 16.3%). In the patients with side effects, 5 (7.0%) patients had systemic diseases including Down’s syndrome (2 patients), mild cerebral palsy (1), congenital hydrocephalus (1), and atrial septal defect (1). All symptoms were transient and there were no serious side effects.
Cyclopentolate
Patient’s gender
A total of 2238 patients (age range, 2 months to 14.9 years; mean age ± SD, 5.7 ± 3.0 years) used cyclopentolate. Of these, 1,129 (50.4%) were boys and 1,109 (49.6%) were girls. In 8 of the 9 institutions, cyclopentolate was instilled twice with an interval of 5-15 minutes. The remaining institution used only one instillation. Refraction was examined 40-90 minutes after the instillation.
Incidence rate of side effects
Of 2,238, 27 (1.2%) patients (mean age ± SD, 4.0 ± 2.2 years) including 12 (44.4%) boys and 15 (55.5%) girls had side effects. The side effect incidence rates of June (1.5%), July (2.7%), September (2.8%), October (2.0%), and January (1.6%) were higher than the overall rate of 1.2% but no distinct difference was found.
The difference of side effect incidence rate between atropine (8.8%) and cyclopentolate (1.2%) was 7.5% (95% confidence interval: 5.6%, 9.5%; P < 0.01; Fisher’s exact test).
Association between the incidence rate of side effects and age
Table 3 shows the age-specific incidence rate of side effects. The patients under one-year old had the highest rate (4/74, 5.4%) and the patients between 3-4 years old had the lowest rate (2/328, 0.6%) (Table 3).
Side effects and systemic diseases
Among the side effects, drowsiness (10/27, 37.0%), red eye (4/27, 14.8%), flush (3/27, 11.1%), and redness (3/27, 11.1%) had the top three incidence rates (Figure 4). Other side effects included hyperactivity, bad mood, skin sores and conjunctivitis. Of the 27 patients showing side effects, 7 (25.9%) patients had systemic diseases including Down’s syndrome (2 patients), craniosynostosis syndrome (1), Cornelia de Lange syndrome (1), agenesis of the corpus callosum (1), periventricular leukomalacia (1), and complications of respiratory distress syndrome, patent ductus arteriosus, and hypokalemia (1). All the symptoms were transient and no serious side effects were observed.
Discussion
This multicenter study showed that in children aged 15 years or younger, atropine had a side effect incidence rate (8.8%) 7 times higher than the rate of cyclopentolate (1.2%). Flush and fever accounted for 86.2% of the side effects caused by atropine. The main side effect caused by cyclopentolate was drowsiness (37.0%).
Reports claim that the accommodative cycloplegic effects of atropine and cyclopentolate do not differ significantly [10,11,12]. On the other hand, some studies show that atropine can produce larger cycloplegia than cyclopentolate for 0.3 D to 1.0 D [4, 13,14,15,16]. Particularly in cases of esotropia, atropine is often used to evaluate the accommodative factors and to avoid under-correction of hyperopia [1]. However, the risk of side effects is the biggest concern for atropine [1]. In this study, all the participating institutions had ophthalmologists specializing in strabismus and amblyopia. The directions for eye drops use were fully explained to the patients orally or in writing; nevertheless the side effect incidence rate of atropine (8.8%) was higher than the rates previously reported (1.7% to 5.5%) [2,3,4,5]. Compared to the previous studies which were conducted retrospectively, the occurrence of side effects could have been closely observed in this 1-year prospective study and resulted in a higher incidence rate. Of 811, only 11(1.4%) patients used 1% atropine eye ointment and none of them had side effects. Eye ointment might possibly cause fewer side effects than eye drops. Choice of either eye ointment or eye drops could be a factor in the occurrence of side effects.
The main side effects of atropine were flush and fever and they occurred in 81.1% of the patients showing side effects within 3 days from the initiation of the eye drops. These results were consistent with previous results [4, 17]. In a 3-year retrospective study, Toyama et al. report that flush and fever often occur when the average temperature is over 30 °C [5]. This can be attributed to the anticholinergic action that suppresses sweating in a high temperature environment. We also obtained a similar result showing July as the month with the highest side effect incidence rate. On the other hand, the side effect incidence rate for August (9.5%) was higher than the overall rate (8.8%) but lower than the rates for other months during the hot season. Although a clear explanation could not be made, we suspect that the frequent use of air conditioning in August might be the reason for the low rate. Therefore, when using atropine during the hot season it is important to pay attention to both the side effects and eye drops concentration.
Drowsiness, ataxia, and visual hallucinations are side effects of cyclopentolate reported in several case studies [6,7,8,9]. A recent prospective observational cohort study also reports drowsiness as the main side effect of cyclopentolate and a side effect incidence rate of 10.3% [18], much higher than the incidence rate in this study (1.2%). Since drowsiness is a side effect which can either be subjectively self-reported or objectively observed, the difference in determining the status of drowsiness might have caused the difference in the incidence rate between the current and previous studies.
In the patients with side effects, more patients using cyclopentolate had systemic diseases than those using atropine. Atropine is often avoided in patients with systemic diseases. This might have caused a bias subject inclusion and affected the side effects’ incidence rate of atropine. This is in fact the limitation of this study. Therefore, the connection between systemic diseases and the occurrence of side effects will need further investigation.
In conclusion, as cycloplegic agents, both atropine and cyclopentolate should be used judiciously. Regarding the occurrence of side effects, atropine requires even greater care than cyclopentolate particularly in children under one-year old. When using atropine in children of young age, eye drops of low concentration may be more appropriate as they cause fewer side effects. The results of this multicenter prospective study with a large number of subjects can contribute to the safety of using accommodative cycloplegic eye drops and provide the basic data to make guidelines for use of cycloplegic agents.
References
Wakayama A, Nishina S, Miki A, Utsumi T, Sugasawa J, Hayashi T, et al. Institutional standards for accommodative cycloplegic eye drops and their side effects in Japanese children: a multicenter study. Nippon Ganka Gakkai Zasshi. 2017;121:529–34 (in Japanese).
Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs. patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120:268–78.
Repka MX, Cotter SA, Beck RW, Kraker RT, Birch EE, Everett DF, et al. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111:2076–85.
Mori T, Yago K, Iida T, Hashimoto T. Refraction of children after cycloplegia with 1% atropine. Folia Jpn Ophtholmol Clin. 2008;1:157–60 (in Japanese).
Toyama E, Seki Y, Takahashi R, Umebara I, Wakayama A, Tanabe F, et al. Incidence and symptoms of atropine side effect in children. Jpn Orthopt J. 2014;43:213–8.
Beswick JA. Psychosis from cyclopentolate. Am J Ophthalmol. 1962;53:879–80.
Mark HH. Psychotogenic properties of cyclopentolate. JAMA. 1963;26:430–1.
Bhatia SS, Vidyashankar C, Sharma RK, Dubey AK. Systemic toxicity with cyclopentolate eye drops. Indian Pediatr. 2000;37:329–31.
Pooniya V, Pandey N. Systemic toxicity of topical cyclopentolate eye drops in a child. Eye. 2012;26:1391–2.
Celebi S, Aykan Ü. The comparison of cyclopentolate and atropine in patients with refractive accommodative esotropia by means of retinoscopy, autorefractometry and biometric lens thickness. Acta Ophthalmol Scand. 1999;77:426–9.
Sani RY, Hassan S, Habib SG, Ifeanyichukwu EP. Cycloplegic effect of atropine compared with cyclopentolate–tropicamide combination in children with hypermetropia. Niger Med J. 2016;57:173–7.
Farthood QK. Cycloplegic refraction in children with cyclopentolate versus atropine. J Clin Exp. 2012;3:239. https://doi.org/10.4172/2155-9570.1000239.
Robb RM, Peterson RA. Cycloplegic refraction in children. J Pediatr Ophthalmol. 1968;5:110–4.
Rosenbaum AL, Bateman JB. Cycloplegic refraction in esotropic children cyclopentolate versus atropine. Ophthalmology. 1981;88:1031–4.
Stolovitch C, Loewenstein A. The use of cyclopentolate versus atropine cycloplegia in esotropic caucasian children. Binocul Vis Q. 1992;7:93–6.
Kawamoto K, Hayasaka S. Cycloplegic refractions in Japanese children: a comparison of atropine and cyclopentolate. Ophthalmologica. 1997;211:57–60.
Piano M, O’Connor AR, Newsham D. Use of atropine penalization to treat amblyopia in Uk orthoptic practice. J Pediatr Ophthalmol. 2014;51:363–9.
Van Miderhout HM, Joosse MV, Grootendorst DC, Schlij-Delfos NE. Adverse reactions following routine anticholinergic eye drops in a pediatric population: an observational cohort study. BMJ Open. 2015;5:e008798.
Acknowledgments
The authors thank Reiyo Tahara for editorial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
A. Wakayama, None; S. Nishina, None; A. Miki, None; T. Utsumi, None; J. Sugasawa, None; T. Hayashi, None; M. Sato, None; A. Kimura, None; T. Fujikado, None.
Additional information
Corresponding author: Akemi Wakayama
About this article
Cite this article
Wakayama, A., Nishina, S., Miki, A. et al. Incidence of side effects of topical atropine sulfate and cyclopentolate hydrochloride for cycloplegia in Japanese children: a multicenter study. Jpn J Ophthalmol 62, 531–536 (2018). https://doi.org/10.1007/s10384-018-0612-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-018-0612-7