Abstract
Reducing patient wait times is a key operational goal and impacts patient outcomes. The purpose of this study is to explore the effects of different radiology scheduling strategies on exam wait times before and after holiday periods at an outpatient imaging facility using computer simulation. An idealized Monte Carlo simulation of exam scheduling at an outpatient imaging facility was developed based on the actual distribution of scheduled exams at outpatient radiology sites at a tertiary care medical center. Using this simulation, we examined three scheduling strategies: (1) no scheduling modifications, (2) increase imaging capacity before or after the holiday (i.e. increase facility hours), and (3) use a novel rolling release scheduling paradigm. In the third scenario, a fraction of exam slots are blocked to long-term follow-up exams and made available only closer to the exam date, thereby preventing long-term follow-up exams from filling the schedule and ensuring slots are available for non-follow-up exams. We examined the effect of these three scenarios on utilization and wait times, which we defined as the time from order placement to exam completion, during and after the holiday period. The baseline mean wait time for non-follow-up exams was 5.4 days in our simulation. When no scheduling modifications were made, there was a significant increase in wait times in the week preceding the holiday when compared to baseline (10.0 days vs 5.4 days, p < 0.01). Wait times remained elevated for 4 weeks following the holiday. Increasing imaging capacity during the holiday and post-holiday period by 20% reduced wait times by only 6.2% (9.38 days vs 10.0 days, p < 0.01). Increasing capacity by 50% resulted in a 7.1% reduction in wait times (9.28 days, p < 0.01), and increasing capacity by 100% resulted in a 13% reduction in wait times (8.75 days, p < 0.01). In comparison, using a rolling release model produced a reduction in peak wait times equivalent to doubling capacity (8.76 days, p < 0.01) when 45% of slots were reserved. Improvements in wait times persisted even when rolling release was limited to the 3 weeks preceding or 1 week following the holiday period. Releasing slots on a rolling basis did not significantly decrease utilization or increase wait times for long-term follow-up exams except in extreme scenarios where 80% or more of slots were reserved for non-follow-up exams. A rolling release scheduling paradigm can significantly reduce wait time fluctuations around holiday periods without requiring additional capacity or impacting utilization.
Similar content being viewed by others
Introduction
Radiology wait times impact both clinical outcomes [1] and the patient experience [2]. Patient wait times are second only to staff communication and behavior in radiation patient feedback reports [3], and a large portion of patient complaints at radiology centers focus on delays [4]. Moreover, long patient wait times for imaging are known to be associated with worse patient outcomes [1, 5]. As a result, wait times represent a key metric for operational improvement [6,7,8,9]. Facilities may respond to wait times exacerbations by increasing capacity through additional staff, hours, or equipment. Unfortunately, these traditional strategies to improve wait times can incur significant costs. As a result, there is a pressing need to identify additional strategies to minimize patient wait times, ideally without requiring increased imaging capacity.
Even at institutions where wait times are well controlled during normal operations, holiday periods may lead to significant exacerbations in wait times. In our experience at outpatient oncologic imaging facilities affiliated with a tertiary care center in an urban area of the northeastern United States, patients often prefer to avoid scheduling long-term follow-up exams during holiday periods, such as the last week of December. If a patient’s 3-, 6-, or 9-month follow-up imaging date falls during a holiday period, the patient may decline to be scheduled into the holiday period and instead request a slot in the following week. This process, we suspect, fills up the scheduling slots in the post-holiday period, reducing the number of slots available to patients who need short-term, non-follow-up exams during the post-holiday period.
It remains unknown whether alternative scheduling practices can reduce acute exacerbations in wait times without affecting capacity utilization or requiring increased staffing. Unfortunately, experimentally altering scheduling practices at real-world radiology sites may be disruptive and impractical. Computer simulations are frequently used in other contexts to study operational improvements without disrupting real-world operations [6]. However, simulations have not previously been used to understand how scheduling practices can improve outpatient radiology wait times. To this end, we developed a simulation of patient scheduling at an outpatient radiology practice. We then use this simulation to examine the specific case of a week-long holiday period. The purpose of this study is to explore the impact of different scheduling practices on exam wait times around a week-long holiday using a Monte Carlo simulation.
Methods
Monte Carlo Simulation
We developed an idealized Monte Carlo simulation of exam scheduling at a single-modality outpatient imaging facility using the R programming language. This computer simulation sequentially schedules radiology patients into future appointment slots. Each patient is randomly assigned a desired order-to-exam time. For example, if a patient required a 30-day follow-up CT, this would correspond to a desired order-to-exam time of 30 days. As the actual distribution of real order-to-exam wait times at outpatient imaging sites affiliated with a tertiary care center drops off rapidly, we used an exponential distribution to model the desired order-to-exam times.
The simulation attempts to schedule a patient into the date corresponding to the desired order-to-exam time. We assume patients would prefer to schedule a later slot rather than seek a different imaging facility. Consequently, if the target date has no remaining exam slots, the simulation schedules the patient into the next available date. For each patient, the desired number of days from order placement to exam completion and the actual number days from order to exam were recorded. We defined total wait time as the number of days from order placement to exam completion.
The capacity of the simulated site was fixed arbitrarily at 40 exams per day, which is similar to the actual capacity at imaging sites affiliated with our institution. The number of patients per day was allowed to vary according to a truncated normal distribution centered at 90% of daily imaging capacity. The simulation was then run out to 120 weeks and then iterated through 1,000 runs. The first 40 and last 10 weeks of each simulation were discarded to remove edge effects. We computed the median wait time per week across all simulations. For the purposes of this simulation, we defined “non-follow-up exams” as those exams that the ordering physician intends to be completed within 30 days. We also refer to these as “short-term exams.” Wait times were also computed separately for short-term exams versus longer-term exams.
In our clinical experience, patients frequently request to have their imaging appointments scheduled outside of major holiday periods. In this simulation, we assume that 90% of patients whose initial appointment dates fall in the holiday period will request to be rescheduled into later dates in the post-holiday period. For example, suppose an order for a 30-day follow-up imaging study is placed by a physician. If an exam slot is available 30 days from the date of order placement, the patient will first be offered this slot. However, if this date lies in the holiday period, we assume there is a 90% probability that the patient will decline this appointment and request to be rescheduled to the first available slot after the holiday period. We selected a 90% probability to accentuate model dynamics around the holiday period and to better differentiate between alternative scheduling scenarios. We simulated the holiday at week 100 to allow the model to achieve a steady state prior to the holiday. The model was implemented in the R programming language using the tidyverse collection of packages [10, 11].
Scenarios
Using this model, we studied the impact of a week-long holiday on wait times and utilization. We examined three scenarios.
Baseline
In the first scenario, scheduling and staffing were unchanged throughout the holiday period. This scenario explored the impact of the simulated holiday in the absence of scheduling or staffing changes.
Increased Capacity
In the second scenario, additional imaging capacity was added in the 4 weeks after the holiday period in an attempt to address post-holiday exacerbations in wait times. This is typically accomplished by increasing staffing or facility hours.
Rolling Release
In the third scenario, a novel scheduling strategy that we term “Rolling Release” was implemented in an attempt to reduce wait times.
As discussed previously, in our clinical experience, patients are often reluctant to be scheduled for imaging in a holiday period, and patients whose long-term follow-up exam date should fall within the holiday period frequently request to be rescheduled into later exam dates in the post-holiday period. As a result, we suspect that reserving a fraction of post-holiday slots for non-follow-up exams, defined here as exams ordered for completion within the next 30 days, might reduce the exacerbation in post-holiday wait times. In this scheduling strategy, a portion of exam slots only become available within 30 days of the exam date. Patients can only be scheduled into these slots within 30 days of the slot, ensuring that a certain number of exam slots will not be filled by long-term follow-up exams scheduled far in advance. In effect, these slots are reserved for non-follow-up exams. We chose to release slots on a 30 day basis, as opposed to an earlier or later release, to balance the needs for 60-, 90-, and 180-day follow-up exams against exams with shorter turnaround times. We explored multiple rolling release models in which a varying percentage of exam slots were reserved for rolling release. In each scenario, utilization and wait times were calculated before, during, and after the holiday period. Peak wait times and utilization rates were compared against baseline wait times and baseline utilization rates using t-tests. Lastly, we simulated the effect of limiting the rolling release period to a shorter period before or after the holiday.
Results
The baseline mean wait time for short-term (< 30 day) exams was 5.4 days in our simulation (Fig. 1). Wait times ranged from 3.2 days to 8.0 days, with a standard deviation of 0.58 days. The median wait time was 5.8 days.
Wait times were significantly increased before, during, and following a week-long holiday. A week-long holiday was simulated at week 100 (gray vertical line). When no scheduling adjustments were made, wait times in weeks 99 through 104 were significantly worse than the baseline mean wait times without a holiday (green horizontal line). Large increases in capacity by 20% or more were needed to produce meaningful reductions in peak wait times
Scenario 1: No Scheduling Modifications
When no scheduling adjustments were made, a week-long holiday resulted in a significant increase in wait times starting in the week prior to the holiday. Wait times peaked in the week preceding the holiday (10.0 days vs 5.4 days, p < 0.01). Wait times remained elevated for the holiday and four subsequent weeks (8.80, 7.75, 6.90, 6.20, and 5.75 days, respectively, all p < 0.01). Wait times returned to baseline levels in the following weeks.
Scenario 2: Increasing Capacity After the Holiday
Increasing capacity in the 4 weeks after the holiday resulted in reductions in wait times (Table 1 and Fig. 1). In Table 1, each row corresponds to the scheduling scenario listed in the first column. The first row corresponds to a holiday without any scheduling changes, as in the first scenario above. The subsequent rows correspond to simulations in which additional capacity is added in the 4 weeks following the holiday period. Increasing capacity by 20% reduced wait times by 6.2% (9.38 days vs 10.0 days, p < 0.01). A 50% increase in capacity resulted in a 7.1% reduction in wait times (9.28 days, p < 0.01). Doubling capacity resulted in a 13% reduction in wait times (8.75 days vs 10.0 days, p < 0.01). Increased capacity did not significantly impact utilization. We additionally considered the case of increasing capacity in the pre-holiday period (data not shown). Increased capacity in the week prior to the holiday did not result in any improvement in peak wait times.
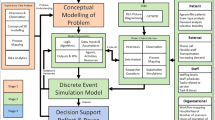
Scenario 3: Rolling Release
Reserving exam slots on a rolling basis by reserving 15 to 75% of exam slots for short-term exams produced significant (p < 0.01) reductions in wait times (Table 2 and Fig. 2). In Table 2, the first row corresponds to a holiday with ordinary scheduling, as described in scenario one above, while each subsequent row has a certain fraction of slots reserved for exams that need to be completed within the next thirty days. Peak wait times ranged from 9.50 to 8.05 days (5.0 to 19.5%), with greater reductions when a larger fraction of exam slots is reserved. Reserving 45% of exam slots on a rolling basis resulted in a 13% reduction in wait times (8.76 days vs 10.0 days, p < 0.01), equivalent to doubling capacity. Moreover, releasing slots on a rolling basis did not significantly increase wait times for long-term follow-up exams except when 80% or more of slots were reserved for short-term exams (Fig. 3).
Releasing slots on a rolling basis improved wait times. A week-long holiday was simulated at week 100 (gray vertical line). When no scheduling changes were made, wait times were significantly worse than the baseline mean wait times without a holiday (green horizontal line). Releasing slots on a rolling basis produced improvements in wait times. Specifically, reserving 45% of slots produces an improvement equivalent to doubling capacity
Rolling release reduced peak wait times without impacting utilization before or after the holiday, except when 80% or more of slots were reserved for short-term exams. Panel A: Each point corresponds to a scenario with the labeled percentage of slots reserved for short-term exams. Peak wait times in days are plotted against the mean utilization in the pre-holiday period. Reserving different fractions of available exam slots for short-term exams did not produce a significant difference in mean utilization, except when a very large proportion (80% or greater) of slots were reserved for short-term exams. Panel B: The same plot is repeated but with mean utilization during the holiday week and four subsequent weeks
As releasing 45% of slots on a 30-day rolling basis was equivalent to doubling capacity, we used 45% reserved capacity as our benchmark for further evaluation. Our initial rolling release model simulated an imaging facility in which rolling release is implemented on an ongoing basis throughout the year. Since rolling release may be difficult to maintain for long periods of time, we then evaluated the impact of restricting rolling release to the period surrounding the holiday. First, we simulated reserving 45% of slots in the weeks preceding the holiday for rolling release and allowing all earlier weeks to be scheduled in the usual first-come, first-served manner without rolling release. Implementing rolling release starting just 3 weeks preceding the holiday produced a significant reduction in peak wait times (9.56 days vs 10.0 days, p < 0.01). Greater improvements in wait times were seen when rolling release was started earlier. No changes in wait times were seen when rolling release was implemented less than 3 weeks prior to the start of the holiday.
Subsequently, we simulated truncating early release after the holiday period. Specifically, we simulated a rolling release of 45% of slots throughout the pre-holiday period and the holiday week followed by a switch to ordinary scheduling at some point during the subsequent post-holiday period. We found that pre-holiday rolling release scheduling produced significant reductions in wait times even when conventional, non-rolling scheduling was re-instituted in the post-holiday period. Indeed, terminating the rolling release scheduling even 1 week after the holiday still produced significant, albeit smaller, reductions in wait times compared to baseline (8.92 days vs 10.0 days, p < 0.01).
Discussion
Our results suggest that wait times exacerbations around a week-long holiday can be managed effectively through a rolling release scheduling system in which a portion of exam slots are reserved for non-follow-up exams. Rolling release produced statistically and operationally significant reductions in peak wait times around a simulated week-long holiday. Specifically, reserving 45% of slots for such exams was equivalent to doubling capacity in the 4 weeks following the holiday. Moreover, reductions in peak wait times occurred even when rolling release was only implemented in the 3 weeks preceding and 1 week following the holiday period.
This improvement in simulated wait times was achieved without requiring additional staffing or increased capacity. In contrast, traditional strategies for reducing patient wait times incorporating increased capacity through greater staffing or increased work hours (as in [1]) can incur significant costs and may be infeasible at many institutions. Rolling block scheduling did not significantly impact wait times for long-term follow-up exams or reduce capacity utilization. In contrast, under a typical scheduling system, resource utilization and wait times are inversely correlated [6], and as a result, reducing wait times through increased capacity may incur additional indirect costs in the form of poor resource utilization, though this was not seen in the present model.
Prior studies have used computer simulations to explore the dynamics of patient wait times [12]. However, most studies of medical wait times have focused on short-term delays in service delivery, such as hours waited beyond a scheduled appointment time, or hours waited for unscheduled services in emergency departments [13], urgent cares, or walk-in radiology facilities [14, 15]. While it is clear that delays of this kind in the context of outpatient imaging can impact patient satisfaction [3, 4], it is unclear the extent to which such imaging delays of this type impact patients’ health outcomes.
In the present study, we considered a related, but distinct, definition of wait times. Specifically, we considered how long patients are made to wait between the placement of an order for an outpatient imaging study and the date on which the exam can actually be completed. Wait times of this kind have not been widely studied, but are known to impact patient outcomes in some contexts. For example, in the context of oncologic imaging, wait times for confirmatory imaging and image-guided biopsies in patients with suspicious lung nodules are correlated with tumor size and stage [1]. In a retrospective study of non-small cell lung cancer patients in Newfoundland, Canada, Byrne and colleagues showed that wait times from an initial abnormal plain film XR to confirmatory CT and wait times from confirmatory CT to CT-guided biopsy were correlated with larger lung tumor size and stage and worse patient prognosis [1]. Moreover, Byrne et al. showed that after imaging wait times at these same institutions were significantly improved by increasing staffing levels, these order-to-exam wait times were no longer correlated with tumor size or stage. Thus, improving wait times for non-acute imaging could potentially have significant impacts on patient outcomes.
In the case discussed by Byrne and colleagues, improvements in wait times and patient outcomes were achieved by hiring additional CT technologists. However, hiring additional staff may be cost prohibitive at some institutions. Our results suggest that a rolling release scheduling model may be useful in managing patient wait times for outpatient imaging. While we considered the specific case of a week-long holiday, our model and analysis are also extensible to a range of scenarios in which patient preferences or facility capacity produce wait time exacerbations. Such scenarios include equipment maintenance periods, staffing shortages, weather events, or other crises in which imaging capacity is limited. This is particularly salient during the COVID-19 pandemic period, in which wait times and patient access are critically important. More broadly, the Monte Carlo approach described here is a flexible tool for evaluating other proposed approaches to scheduling or capacity changes. This model provides a rapid method for evaluating the impact of potentially disruptive changes to radiology department workflows prior to implementation.
This study has several limitations. First, we considered the specific case of a radiology site in which the distribution of order-to-exam times is exponential, with most exams completed within 2 weeks of the order date. This exponential distribution was based on scheduling data from outpatient imaging sites affiliated with a tertiary care center focused on oncology. As a result, the simulation models far fewer long-term follow-up exams than short-notice exams, which is consistent with the realities of a very high mortality patient population. In our simulation, rolling block scheduling ensures that these short-notice exams are scheduled quickly by distributing longer-term exams across a broader range of dates. However, other radiology sites with different patient populations may have different distributions of desired order-to-exam times. In our simulation, rolling release did not result in a statistically significant increase in wait times for longer-term exams. However, in real-world applications with different patient populations, these delays may be significant, particularly at imaging sites with a greater proportion of long-term exams, and further work will be needed to model patients’ choices to select alternate imaging facilities. Additionally, this model does not incorporate variations in exam length or type, which have been shown to impact patient throughput and wait times in other contexts [16,17,18].
In conclusion, rolling release of exam slots can significantly reduce wait time fluctuations around holiday periods without impacting utilization or requiring additional facility hours. Our model suggests that reserving 45% of slots for non-follow-up exams produces an improvement in wait times equivalent to doubling capacity during the post-holiday period. Outpatient radiology facilities should consider implementing a rolling release model to manage wait times around holiday periods, particularly if facility hours or staffing are fixed.
References
Byrne SC, Barrett B, Bhatia R. The Impact of Diagnostic Imaging Wait Times on the Prognosis of Lung Cancer. Can Assoc Radiol J 2015;66:53–57.
Holbrook A, Glenn H, Mahmood R, Cai Q, Kang J, Duszak R. Shorter Perceived Outpatient MRI Wait Times Associated With Higher Patient Satisfaction. Journal of the American College of Radiology 2016;13:505–509.
Rosenkrantz AB, Pysarenko K. The Patient Experience in Radiology: Observations From Over 3,500 Patient Feedback Reports in a Single Institution. Journal of the American College of Radiology 2016;13:1371–1377.
Salazar G, Quencer K, Aran S, Abujudeh H. Patient Satisfaction in Radiology: Qualitative Analysis of Written Complaints Generated Over a 10-Year Period in an Academic Medical Center. Journal of the American College of Radiology 2013;10:513–517.
Lo DS, Zeldin RA, Skrastins R, et al. Time to Treat: A System Redesign Focusing on Decreasing the Time from Suspicion of Lung Cancer to Diagnosis. Journal of Thoracic Oncology 2007;2:1001–1006.
Loving VA, Ellis RL, Rippee R, Steele JR, Schomer DF, Shoemaker S. Time Is Not on Our Side: How Radiology Practices Should Manage Customer Queues. Journal of the American College of Radiology 2017;14:1481–1488.
Camacho F, Anderson R, Safrit A, Jones AS, Hoffmann P. The Relationship between Patient’s Perceived Waiting Time and Office-Based Practice Satisfaction. North Carolina Medical Journal 2006;67:409–413.
Bleustein C, Rothschild DB, Valen A, Valaitis E, Schweitzer L, Jones R. Wait Times, Patient Satisfaction Scores, and the Perception of Care. The American Journal of Managed Care 2014;20:8.
Swan JS, Fryback DG, Lawrence WF, Sainfort F, Hagenauer ME, Heisey DM. A Time-tradeoff Method for Cost—Effectiveness Models Applied to Radiology. Med Decis Making 2000;20:79–88.
R Core Team R. A language and environment for statistical computing; R Foundation for Statistical Computing: Vienna, Austria, 2019
Wickham et al., (2019). Welcome to the tidyverse. Journal of Open Source Software, 4(43), 1686. https://doi.org/10.21105/joss.01686
Cayirli T, Veral E. Outpatient Scheduling in Health Care: A Review of Literature. Production and Operations Management 2009;12:519–549.
Strobel S, Ren KY, Dragoman A, et al. Do Patients Respond to Posted Emergency Department Wait Times: Time-Series Evidence From the Implementation of a Wait Time Publication System in Hamilton, Canada. Annals of Emergency Medicine 2021;78:465–473.
Luo L, Zhang Y, Qing F, Ding H, Shi Y, Guo H. A discrete event simulation approach for reserving capacity for emergency patients in the radiology department. BMC Health Serv Res 2018;18:452.
Curtis C, Liu C, Bollerman TJ, Pianykh OS. Machine Learning for Predicting Patient Wait Times and Appointment Delays. Journal of the American College of Radiology 2018;15:1310–1316.
Godley M, Jenkins JB. Decreasing Wait Times and Increasing Patient Satisfaction: A Lean Six Sigma Approach. Journal of Nursing Care Quality 2019;34:61–65.
McDevitt JL, Quadri RS, Sutphin PD, et al. Capacity Prioritization Initiative Reduced the Wait Time for Port Placement and Facilitated Increased Volume of Port Placements at a Large County Health System. Current Problems in Diagnostic Radiology 2021;50:288–292.
van Lent WAM, Deetman JW, Teertstra HJ, Muller SH, Hans EW, van Harten WH. Reducing the throughput time of the diagnostic track involving CT scanning with computer simulation. European Journal of Radiology 2012;81:3131–3140.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Model design, simulation implementation, and data analysis were performed by Vivek Pisharody and Joseph Erinjeri. The first draft of the manuscript was written by Vivek Pisharody. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study did not involve human or animal subjects or protected health information.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pisharody, V.A., Yarmohammadi, H., Ziv, E. et al. Reducing Wait Times for Radiology Exams Around Holiday Periods: A Monte Carlo Simulation. J Digit Imaging 36, 29–37 (2023). https://doi.org/10.1007/s10278-022-00728-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10278-022-00728-2