Abstract
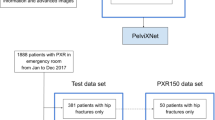
Admission trauma whole-body CT is routinely employed as a first-line diagnostic tool for characterizing pelvic fracture severity. Tile AO/OTA grade based on the presence or absence of rotational and translational instability corresponds with need for interventions including massive transfusion and angioembolization. An automated method could be highly beneficial for point of care triage in this critical time-sensitive setting. A dataset of 373 trauma whole-body CTs collected from two busy level 1 trauma centers with consensus Tile AO/OTA grading by three trauma radiologists was used to train and test a triplanar parallel concatenated network incorporating orthogonal full-thickness multiplanar reformat (MPR) views as input with a ResNeXt-50 backbone. Input pelvic images were first derived using an automated registration and cropping technique. Performance of the network for classification of rotational and translational instability was compared with that of (1) an analogous triplanar architecture incorporating an LSTM RNN network, (2) a previously described 3D autoencoder-based method, and (3) grading by a fourth independent blinded radiologist with trauma expertise. Confusion matrix results were derived, anchored to peak Matthews correlation coefficient (MCC). Associations with clinical outcomes were determined using Fisher’s exact test. The triplanar parallel concatenated method had the highest accuracies for discriminating translational and rotational instability (85% and 74%, respectively), with specificity, recall, and F1 score of 93.4%, 56.5%, and 0.63 for translational instability and 71.7%, 75.7%, and 0.77 for rotational instability. Accuracy of this method was equivalent to the single radiologist read for rotational instability (74.0% versus 76.7%, p = 0.40), but significantly higher for translational instability (85.0% versus 75.1, p = 0.0007). Mean inference time was < 0.1 s per test image. Translational instability determined with this method was associated with need for angioembolization and massive transfusion (p = 0.002–0.008). Saliency maps demonstrated that the network focused on the sacroiliac complex and pubic symphysis, in keeping with the AO/OTA grading paradigm. A multiview concatenated deep network leveraging 3D information from orthogonal thick-MPR images predicted rotationally and translationally unstable pelvic fractures with accuracy comparable to an independent reader with trauma radiology expertise. Model output demonstrated significant association with key clinical outcomes.





Similar content being viewed by others
Abbreviations
- LSTM RNN:
-
Long short-term memory recurrent neural network
- TP:
-
True positive
- TN:
-
True negative
- FP:
-
False positive
- FN:
-
False negative
- TPR:
-
True positive rate
- TNR:
-
True negative rate
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- FNR:
-
False negative rate
- FPR:
-
False positive rate
- FDR:
-
False discovery rate
- FOR:
-
False omission rate
- DOR:
-
Diagnostic odds ratio
References
Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, Kluger Y, Moore EE, Peitzman AB, Ivatury R. Pelvic trauma: WSES classification and guidelines. World J of Emerg Surg 12(1):15,2017
Garlapati AK, Ashwood N. An overview of pelvic ring disruption. Trauma 14(2):169-178,2012
Dreizin D. Commentary on “Multidetector CT in Vascular Injuries Resulting from Pelvic Fractures”. RadioGraphics 39(7):2130-2133,2019
Raniga SB, Mittal AK, Bernstein M, Skalski MR, Al-Hadidi AM. Multidetector CT in Vascular Injuries Resulting from Pelvic Fractures: A Primer for Diagnostic Radiologists. RadioGraphics 39(7):2111-2129,2019
Vaidya R, Scott AN, Tonnos F, Hudson I, Martin AJ, Sethi A. Patients with pelvic fractures from blunt trauma. What is the cause of mortality and when? Am J Surg 211(3):495–500,2016
Costantini TW, Coimbra R, Holcomb JB, Podbielski JM, Catalano R, Blackburn A, Scalea TM, Stein DM, Williams L, Conflitti J. Current management of hemorrhage from severe pelvic fractures: results of an American Association for the Surgery of Trauma multi-institutional trial. J Trauma Acute Care 80(5):717-725,2016
Yoshihara H, Yoneoka D. Demographic epidemiology of unstable pelvic fracture in the United States from 2000 to 2009: trends and in-hospital mortality. J Trauma Acute Care Surg 76(2):380-385,2014
Dreizin D, Nascone J, Davis DL, Mascarenhas D, Tirada N, Chen H, Bodanapally UK. Can MDCT unmask instability in binder-stabilized pelvic ring disruptions? Am J Roentgenol 2016;207(6):1244-1251,2016
Tile M. Acute pelvic fractures: I. Causation and classification. JAAOS-J Am Acad Orthop Surg 4(3):143–151,1996
Hanson PB, Milne JC, Chapman MW. Open fractures of the pelvis. Review of 43 cases. J Bone Surg Brit 73(2):325–329,1991
Slater S, Barron D. Pelvic fractures—A guide to classification and management. Eur J Radiol 74(1):16-23,2010
Cooper J. Pelvic ring injuries. Trauma 8(2):95-110,2006
Van Vugt A, Van Kampen A. An unstable pelvic ring: the killing fracture. J Bone Joint Surg Brit 88(4):427-433,2006
Osterhoff G, Scheyerer MJ, Fritz Y, Bouaicha S, Wanner GA, Simmen H-P, Werner CM. Comparing the predictive value of the pelvic ring injury classification systems by Tile and by Young and Burgess. Injury 45(4):742-747,2014
Berger-Groch J, Thiesen DM, Grossterlinden LG, Schaewel J, Fensky F, Hartel MJ. The intra-and interobserver reliability of the Tile AO, the Young and Burgess, and FFP classifications in pelvic trauma. Arch Orthop Trauma Surg 139(5):645-650,2019
Alton TB, Gee AO. Classifications in brief: Young and Burgess classification of pelvic ring injuries. Springer, 2014
Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surgery Brit 70(1):1-12,1988
Zingg T, Uldry E, Omoumi P, Clerc D, Monier A, Pache B, Moshebah M, Butti F, Becce F. Interobserver reliability of the Tile classification system for pelvic fractures among radiologists and surgeons. Eur Radiol 2020, pp 1–9
Koo H, Leveridge M, Thompson C, Zdero R, Bhandari M, Kreder HJ, Stephen D, McKee MD, Schemitsch EH. Interobserver reliability of the young-burgess and tile classification systems for fractures of the pelvic ring. J Orthop Trauma 22(6):379-384,2008
Bucholz R. The pathological anatomy of Malgaigne fracture-dislocations of the pelvis. J Bone Joint Surg Am 63(3):400-404,1981
Dreizin D, Bodanapally U, Mascarenhas D, O’Toole RV, Tirada N, Issa G, Nascone J. Quantitative MDCT assessment of binder effects after pelvic ring disruptions using segmented pelvic haematoma volumes and multiplanar caliper measurements. Eur Radiol 28(9):3953-3962,2018
Gabbe BJ, Esser M, Bucknill A, Russ MK, Hofstee D-J, Cameron P, Handley C, deSteiger RN. The imaging and classification of severe pelvic ring fractures: experiences from two level 1 trauma centres. Bone Joint J 95(10):1396-1401,2013
Dreizin D, Bodanapally U, Boscak A, Tirada N, Issa G, Nascone JW, Bivona L, Mascarenhas D, O’Toole RV, Nixon E. CT prediction model for major arterial injury after blunt pelvic ring disruption. Radiology 287(3):1061-1069,2018
Gänsslen A, Pohlemann T, Paul C, Lobenhoffer P, Tscherne H. Epidemiology of pelvic ring injuries. Injury 27:13-20,1996
Hussami M, Grabherr S, Meuli RA, Schmidt S. Severe pelvic injury: vascular lesions detected by ante-and post-mortem contrast medium-enhanced CT and associations with pelvic fractures. Int J Legal Med 131(3):731-738,2017
Ruatti S, Guillot S, Brun J, Thony F, Bouzat P, Payen J, Tonetti J. Which pelvic ring fractures are potentially lethal? Injury 46(6):1059-1063,2015
Agri F, Bourgeat M, Becce F, Moerenhout K, Pasquier M, Borens O, Yersin B, Demartines N, Zingg T. Association of pelvic fracture patterns, pelvic binder use and arterial angio-embolization with transfusion requirements and mortality rates; a 7-year retrospective cohort study. BMC Surg 17(1):104,2017
Dreizin D, Zhou Y, Chen T, Li G, Yuille AL, McLenithan A, Morrison JJ. Deep learning-based quantitative visualization and measurement of extraperitoneal hematoma volumes in patients with pelvic fractures: potential role in personalized forecasting and decision support. J Trauma Acute Care Surg, 2019
Dreizin D, Munera F. Blunt polytrauma: evaluation with 64-section whole-body CT angiography. Radiographics 32(3):609-631,2012
Battey TW, Dreizin D, Bodanapally UK, Wnorowski A, Issa G, Iacco A, Chiu W. A comparison of segmented abdominopelvic fluid volumes with conventional CT signs of abdominal compartment syndrome in a trauma population. Abdominal Radiol, 2019, pp 1–8
Dreizin D, Bodanapally UK, Munera F. MDCT of complications and common postoperative findings following penetrating torso trauma. Emerg Radiol 22(5):553-563,2015
Dreizin D, Menaker J, Scalea TM. Extracorporeal membranous oxygenation (ECMO) in polytrauma: what the radiologist needs to know. Emerg Radiol 22(5):565-576,2015
Dreizin D, LeBedis CA, Nascone JW. Imaging Acetabular Fractures. Radiologic Clinics 57(4):823-841,2019
Gan K, Xu D, Lin Y, Shen Y, Zhang T, Hu K, Zhou K, Bi M, Pan L, Wu W. Artificial intelligence detection of distal radius fractures: a comparison between the convolutional neural network and professional assessments. Acta Orthop, 2019, pp 1–12
Olczak J, Fahlberg N, Maki A, Razavian AS, Jilert A, Stark A, Sköldenberg O, Gordon M. Artificial intelligence for analyzing orthopedic trauma radiographs: deep learning algorithms—are they on par with humans for diagnosing fractures? Acta Orthop 88(6):581-586,2017
Kim D, MacKinnon T. Artificial intelligence in fracture detection: transfer learning from deep convolutional neural networks. Clin Radiol 73(5):439-445,2018
Urakawa T, Tanaka Y, Goto S, Matsuzawa H, Watanabe K, Endo N. Detecting intertrochanteric hip fractures with orthopedist-level accuracy using a deep convolutional neural network. Skeletal Radiol 48(2):239-244,2019
Thian YL, Li Y, Jagmohan P, Sia D, Chan VEY, Tan RT. Convolutional neural networks for automated fracture detection and localization on wrist radiographs. Radiol Artif Intell1(1):e180001,2019
Wang Y, Lu L, Cheng C-T, Jin D, Harrison AP, Xiao J, Liao C-H, Miao S. Weakly Supervised Universal Fracture Detection in Pelvic X-Rays. International Conference on Medical Image Computing and Computer-Assisted Intervention: Springer, 2019, pp 459–467
Kitamura G, Chung CY, Moore BE. Ankle fracture detection utilizing a convolutional neural network ensemble implemented with a small sample, de novo training, and multiview incorporation. J Digit Imaging, 2019, pp 1–6
Rayan JC, Reddy N, Kan JH, Zhang W, Annapragada A. Binomial classification of pediatric elbow fractures using a deep learning multiview approach emulating radiologist decision making. Radiol Artif Intell 1(1):e180015,2019
Chung SW, Han SS, Lee JW, Oh K-S, Kim NR, Yoon JP, Kim JY, Moon SH, Kwon J, Lee H-J. Automated detection and classification of the proximal humerus fracture by using deep learning algorithm. Acta Orthop 89(4):468-473,2018
Dreizin D, Goldmann F, Chen T, M U. Automated CT pelvic fracture severity grading with deep learning: association with clinical outcomes. Conference on Machine Intelligence in Medical Imaging (C-MIMI). Austin, TX: SIIM, 2019
Dreizin D, Bodanapally UK, Neerchal N, Tirada N, Patlas M, Herskovits E. Volumetric analysis of pelvic hematomas after blunt trauma using semi-automated seeded region growing segmentation: a method validation study. Abdominal Radiol 41(11):2203-2208,2016
Ligisha P BS. A survey on pelvic bone fracture detection. Int J Adv Res Sci Eng Technol 5(22):19-22,2016
Najarian K, Wu J, Davuluri P, Ward K, Hargraves RH. Automated computer-aided decision support for traumatic pelvic and abdominal injuries
Smith R, Najarian K, Ward K. A hierarchical method based on active shape models and directed Hough transform for segmentation of noisy biomedical images; application in segmentation of pelvic X-ray images. BMC Med Inform Decis Mak 9(1):S2,2009
Chowdhury AS, Burns JE, Mukherjee A, Sen B, Yao J, Summers RM. Automated detection of pelvic fractures from volumetric CT images. 2012 9th IEEE International Symposium on Biomedical Imaging (ISBI): IEEE, 2012, pp 1687–1690
Wu J, Davuluri P, Ward KR, Cockrell C, Hobson R, Najarian K. Fracture detection in traumatic pelvic CT images. J Med Imaging 2012:1,2012
Su H, Maji S, Kalogerakis E, Learned-Miller E. Multi-view convolutional neural networks for 3d shape recognition. Proceedings of the IEEE international conference on computer vision, 2015, pp 945–953
Ritter D, Orman J, Schmidgunst C, Graumann R. 3D soft tissue imaging with a mobile C-arm. Comput Med Imaging Graph 31(2):91-102,2007
Rao YR, Prathapani N, Nagabhooshanam E. Application of normalized cross correlation to image registration.Int J Adv Res Sci Eng Technol 3(5):12-16,2014
Sullivan J, Blake A, Isard M, MacCormick J. Bayesian object localisation in images. Int J Comp Vis 44(2):111–135,2001 https://doi.org/10.1023/A:1011818912717
Xie S, Girshick R, Dollár P, Tu Z, He K. Aggregated residual transformations for deep neural networks. Proceedings of the IEEE conference on computer vision and pattern recognition, 2017, pp 1492–1500
Boughorbel S, Jarray F, El-Anbari M. Optimal classifier for imbalanced data using Matthews Correlation Coefficient metric. PloS one 12(6),2017
Matthews BW. Comparison of the predicted and observed secondary structure of T4 phage lysozyme. Biochimica et Biophysica Acta (BBA)-Protein Structure 405(2):442–451,1975
Deng J, Dong W, Socher R, Li L-J, Li K, Fei-Fei L. ImageNet: A large-scale hierarchical image database. Computer Vision and Pattern Recognition, 2009, pp 248-255
Springenberg JT, Dosovitskiy A, Brox T, Riedmiller MA. Striving for Simplicity: The All Convolutional Net. International Conference on Learning Representations, 2015
Sekuboyina A, Rempfler M, Valentinitsch A, Loeffler M, Kirschke JS, Menze BH. Probabilistic point cloud reconstructions for vertebral shape analysis. Medical Image Computing and Computer-Assisted Intervention, 2019, pp 375–383
Yu L, Yang X, Chen H, Qin J, Heng PA. Volumetric ConvNets with mixed residual connections for automated prostate segmentation from 3D MR images. Thirty-first AAAI conference on artificial intelligence, 2017
Anderson SW, Soto JA, Lucey BC, Burke PA, Hirsch EF, Rhea JT. Blunt trauma: feasibility and clinical utility of pelvic CT angiography performed with 64–detector row CT. Radiol 246(2):410-419,2008
Funding
1. NIH K08 EB027141-01A1 (PI: David Dreizin, MD). 2. RSNA Research Scholar Grant (#RSCH1605) (PI: David Dreizin, MD). 3. Accelerated Translational Incubator Pilot (ATIP) award, University of Maryland (PI: David Dreizin, MD).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dreizin, D., Goldmann, F., LeBedis, C. et al. An Automated Deep Learning Method for Tile AO/OTA Pelvic Fracture Severity Grading from Trauma whole-Body CT. J Digit Imaging 34, 53–65 (2021). https://doi.org/10.1007/s10278-020-00399-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10278-020-00399-x