Abstract
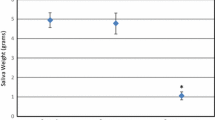
Tongue pressure is reportedly associated with dysphagia. This study investigated relationships among characteristics of head and neck cancer, tongue pressure and dysphagia screening tests performed in patients with head and neck cancer during the acute phase after surgical resection. Fifty-seven patients (36 men, 21 women; age range 26–95 years) underwent surgical resection and dysphagia screening tests (Repetitive Saliva Swallowing Test, Water Swallowing Test, Modified Water Swallowing Test and Food Test) and pre- and postoperative measurement of tongue pressure at 5 time points (preoperatively, and 1–2 weeks and 1, 2, and 3 months postoperatively). Progression of cancer (stage), tracheotomy, surgical reconstruction, chemotherapy, radiotherapy and neck dissection were factors associated with postoperative tongue pressure. Data were analyzed by linear mixed-effect model, Spearman correlation coefficient and receiver operating characteristic (ROC) curve. Tongue pressure was significantly reduced 1–2 weeks after surgery, and recovered over time. Changes in tongue pressure were significantly associated with stage, radiotherapy and reconstruction. All screening tests showed a significant relationship with tongue pressure. Analysis of ROC and area under the effect curve suggested that a tongue pressure of 15 kPa can be used as a cut-off value to detect dysphagia after surgery for head and neck cancer. Our results suggest that tongue pressure evaluation might offer a safe, useful and objective tool to assess dysphagia immediately postoperatively in patients with head and neck cancer.



Similar content being viewed by others
References
Pauloski BR, Logemann JA, Rademaker AW, McConnel FM, Stein D, Beery Q, et al. Speech and swallowing function after oral and oropharyngeal resections: one-year follow-up. Head Neck. 1994;16:313–22.
Morimoto N, Yamashita T, Sato K, Kurata T, Ikeda Y, Kusuhara T, Murata N, Abe K. Assessment of swallowing in motor neuron disease and Asidan/SCA36 patients with new methods. J Neurol Sci. 2013;324(1–2):149–55.
Suarez-Cunqueiro MM, Schramm A, Schoen R, Seoane-Leston J, Otero-Cepeda XL, Bormann KH, Kokemueller H, Metzger M, Diz-Dios P, Gellrich NC. Speech and swallowing impairment after treatment for oral and oropharyngeal cancer. Arch Otolaryngol Head Neck Surg. 2008;134:1299–304.
Matsui Y, Ohno K, Shirota T, Michiwaki Y, Takahashi K, Yamashita Y, Yoshimasu H, Amagasa M, Okabe S, Ono M, Tei K, Totsuka Y, Tomitsuka K, Fujibayashi K, Satomi T, Chiba H, Matsuura M, Seto K, Sato T, Asada K, Ishibashi K, Umino S, Fujita K, Kinoshita Y, Yamamoto T, Iida S, Ookura M, Kogo M, Hosoda M, Oobu K, Ozeki S. Subjective evaluation of postoperative function in patients who had undergone reconstruction after ablation of tongue/floor of the mouth cancer—a multicenter study through a questionnaire. J Jpn Soc Oral Tumor. 2007;19:7–18.
Hey C, Lange BP, Eberle S, Zaretsky Y, Sader R, Stover T, Wagenblast J. Water swallow screening test for patients after surgery for head and neck cancer: early identification of dysphagia, aspiration and limitations of oral intake. Anticancer Res. 2013;33:4017–21.
Yoshikawa M. Tongue pressure measurement for supporting the dental prosthetic treatment in super aging society. J Jpn Prosthodont Soc. 2013;5:145–8.
Umemoto J, Thuga K, Kitashima T, Tsuboi Y, Furuya H, Akagawa Y, Kikuta T. The relationship between findings in videofluorography and tongue pressure of patients with neuromuscular disease and cerebral infarction. Jpn J Gerodontol. 2008;23:354–9.
Konaka K, Kondo J, Hirota N, Tamine K, Hori K, Ono T, Maeda Y, Sakoda S, Naritomi H. Relationship between tongue pressure and dysphagia in stroke patients. Eur Neurol. 2010;64:101–7.
Hirota N, Konaka K, Ono T, Tamine K, Kondo J, Hori K, Yoshimuta Y, Maeda Y, Sakoda S, Naritomi H. Reduced tongue pressure against the hard palate on the paralyzed side during swallowing predicts dysphagia in patients with acute stroke. Stroke. 2010;41:2982–4.
Ono T, Hori K, Tamine K, Kondo J, Hamanaka S, Sakoda S. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88:150–8.
Ono T, Hori K, Tamine K, Kondo J, Hamanaka S, Sakoda S. Swallowing function quantitative evaluation by the tongue pressure sensor sheet of patients with Parkinson’s disease. J Soc Biomech. 2010;34:105–10.
Takeuchi K, Ozawa Y, Hasegawa J, Tsuda T, Karino T, Ueda A, Toyota K. Usability of maximum tongue pressure measurement in patients with dysphagia or dysarthria—using a newly developed measurement device—. Jpn J Dysphagia Rehabil. 2012;16:165–74.
Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53:1483–9.
Yoshikawa M, Yoshida M, Tsuga K, Akagawa Y, Groher ME. Comparison of three types of tongue pressure measurement devices. Dysphagia. 2011;26:232–7.
Utanohara Y, Hayashi R, Yoshikawa M, Yoshida M, Tsuga K, Akagawa Y. Standard values of maximum tongue pressure taken using newly developed disposable tongue pressure measurement device. Dysphagia. 2008;23:286–90.
Adams V, Mathisen B, Baines S, Lazarus C, Callister R. A systematic review and meta-analysis of measurements of tongue and hand strength and endurance using the Iowa Oral Performance Instrument (IOPI). Dysphagia. 2013;28:350–69.
Kato S, Shimogaki M, Onodera A, Ueda H, Oikawa K, Ikeda K, Kosaka A, Imai M, Hasegawa K. Creating a revised Hasegawa Dementia Scale (HDS-R). Jpn J Geriatr Psychiatry. 1991;2:1339–47.
Leslie Sobin MG, Wittekind C. TNM classification of malignant tumours. 7th ed. Hoboken: Union for International Cancer Control International Union Against Cancer; 2010.
Tsuga K, Yoshikawa M, Oue H, Okazaki Y, Tsuchioka H, Maruyama M, Yoshida M, Akagawa M. Maximal voluntary tongue pressure is decreased in Japanese frail elderly persons. Gerodontology. 2012;29:e1078–85.
Baba M, Saitoh E, Okada S. Dysphagia rehabilitation in Japan. Phys Med Rehabil Clin North Am. 2008;19:929–38.
Sakayori T, Maki Y, Hirata S, Okada M, Ishii T. Evaluation of a Japanese “Prevention of long-term care” project for the improvement in oral function in the high-risk elderly. Geriatr Gerontol Int. 2013;13:451–7.
Satoshi Horiguchi YS. Screening tests in evaluating swallowing function. Jpn Med Assoc J. 2011;54:31–4.
Kubota T. Paralytic dysphagia in the brain vascular disorders—for screening test and the clinical application. Sogo Rehabilitation. 1982;10:271–6.
Osawa A, Maeshima S, Tanahashi N. Water-swallowing test: screening for aspiration in stroke patients. Cerebrovasc Dis (Basel, Switzerland). 2013;35:276–81.
Tohara H, Saitoh E, Mays KA, Kuhlemeier K, Palmer JB. Three tests for predicting aspiration without videofluorography. Dysphagia. 2003;18:126–34.
Tohara H, Saitoh E, Baba M, Onogi K, Uematsu H. Swallowing characteristics and tongue surface movements of persons with regard to pasty foods -a dysphagia evaluation system without videofluorographic study. Jpn J Dysphagia Rehabil. 2002;6:196–206.
Matsuda AMT, Shibata A, Katanoda K, Sobue T, Nishimoto H. The Japan Cancer Surveillance Research Group. National estimates of cancer incidence based on cancer registries in Japan (1975–2010). Jpn J Clin Oncol. 2013;44:388–96.
Matsuda T, Ajiki W, Marugame T, Ioka A, Tsukuma H, Sobue T, Research group of population-based cancer registries of Japan. Population-based survival of cancer patients diagnosed between 1993 and 1999 in Japan: a chronological and international comparative study. Jpn J Clin Oncol. 2011;41:40–51.
Matsuda T, Ajiki W, Marugame T, Ioka A, Tsukuma H, Sobue T. Research Group of Population-Based Cancer Registries of Japan. Jpn J Clin Oncol. 2011;41:40–51.
Thomas L, Moore EJ, Olsen KD, Kasperbauer JL. Long-term quality of life in young adults treated for oral cavity squamous cell cancer. Ann Otol Rhinol Laryngol. 2012;121:395–401.
Payakachat N, Ounpraseuth S, Suen JY. Late complications and long-term quality of life for survivors (>5 years) with history of head and neck cancer. Head Neck. 2013;35:819–25.
Lin BM, Starmer HM, Gourin CG. The relationship between depressive symptoms, quality of life, and swallowing function in head and neck cancer patients 1 year after definitive therapy. Laryngoscope. 2012;122:1518–25.
Hamahata A, Beppu T, Shirakura S, Hatanaka A, Yamaki T, Saitou T, Sakurai H. Tongue pressure in patients with tongue cancer resection and reconstruction. Auris Nasus Larynx. 2014;41:563–7.
Palmer PM, Jaffe DM, McCulloch TM, Finnegan EM, Van Daele DJ, Luschei ES. Quantitative contributions of the muscles of the tongue, floor-of-mouth, jaw, and velum to tongue-to-palate pressure generation. J Speech Lang Hear Res. 2008;51:828–35.
Lazarus C, Logemann JA, Pauloski BR, Rademaker AW, Helenowski IB, Vonesh EF, Mac CE, Mittal BB, Vokes EE, Haraf DJ. Effects of radiotherapy with or without chemotherapy on tongue strength and swallowing in patients with oral cancer. Head Neck. 2007;29:632–7.
Acknowledgements
This study was supported by a grant from the Ministry of Education, Science and Culture of Japan (No. 25463043). The authors declare no conflicts of interest with any financial organization regarding the manuscript. The funder played no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors would like to express their sincere appreciation to K. Yoshikiyo and M. Shiramizu for their tremendous support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Kazuma Sugahara: Co-first author.
Rights and permissions
About this article
Cite this article
Hasegawa, Y., Sugahara, K., Fukuoka, T. et al. Change in tongue pressure in patients with head and neck cancer after surgical resection. Odontology 105, 494–503 (2017). https://doi.org/10.1007/s10266-016-0291-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-016-0291-0