Abstract
Infectious diseases drive countries to provide vaccines to individuals. Due to the limited supply of vaccines, individuals prioritize receiving vaccinations worldwide. Although, priority groups are formed based on age groupings due to the restricted decision-making time. Governments usually ordain different health protocols such as lockdown policy, mandatory use of face masks, and vaccination during the pandemics. Therefore, this study considers the case of COVID-19 with a SEQIR (susceptible–exposed–quarantined–infected–recovered) epidemic model and presents a novel prioritization technique to minimize the social and economic impacts of the lockdown policy. We use retail units as one of the affected parts to demonstrate how a vaccination plan may be more effective if individuals such as retailers were prioritized and age groups. In addition, we estimate the total required vaccine doses to control the epidemic disease and compute the number of vaccine doses supplied by various suppliers. The vaccine doses are determined using optimal control theory in the solution technique. In addition, we consider the effect of the mask using policy in the number of vaccine doses allocated to each priority group. The model’s performance is evaluated using an illustrative scenario based on a real case.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A report of COVID-19 cases was released in late 2019 in Wuhan, China. The first case of the disease was reported in Iran on February 20, 2020. COVID-19 had caused 5.34 million deaths worldwide as of December 2021, with 131,000 deaths in Iran. The world economy is expected to contract by 5.2% this year, according to World Bank estimates.Footnote 1 Thus, indirect effects such as business and shop closures should be considered in addition to the disease’s direct effects, such as morbidity and death, and its societal consequences. Ceylan and Ozkan [1] assess the majority of known epidemics and their effects on economics and socio-politics by examining scientific literature. They evaluate COVID-19’s potential effects, as well as approaches to mitigate them. The most urgent socio-economic actions required to battle the negative effects of a communicable disease are those relating to unemployment and its income effects, as well as the security of all sectors. They believe that to avoid long-term unemployment, the service, retail, and even industrial sectors must be supported.
Because of the epidemic’s prevalence, appropriate precautions and responses had to be considered. Vaccination, medication, education, lockdown, quarantine, using face masks, and home health care are just a few of the techniques available to combat epidemics [2,3,4]. One of the most promising treatments for dealing with epidemic diseases is vaccination [5, 6]. However, several elements of COVID-19 conditions, such as unclear identification, cause vaccine production to be delayed, with varying yields. On the other side, the worldwide demand for vaccines has resulted in a scarcity of COVID-19 effective vaccines [7]. The unavailability of medicines and vaccinations to cope with the infectious disease during the COVID-19 pandemic led to the use of various non-drug therapies, which came at a high financial cost to governments [8]. Therefore, developing an effective and responsive plan for individual priority would be unavoidable, given that the amount of vaccine doses available is insufficient to vaccinate all the persons at the same time.
In different pandemics, the World Health Organization (WHO) recognizes high-risk populations and underlines that they should be given more attention than other public health issues. The primary purposes of prioritizing vaccination for individuals are to preventing pandemic-related mortality, reducing social disruptions, limiting economic harm, and maintaining the infrastructure [9]. In different infectious disease outbreaks, various priority strategies are offered. For example, during the 2009 H1N1 influenza outbreak, Lee et al. [10] identified five priority categories based on computer modeling, including pregnant women, infants under 6 months, healthcare workers, adults aged 6 months to 24 years, and high-risk individuals aged 25–65 years.
When defining the priority groups, it is vital to remember that the epidemic is a dynamic system that evolves with each state. The immunization of distinct groups is done one after another, according to WHO’s priority groups under various vaccine supply scenarios. Thus, the time it takes for each priority group to obtain the vaccination is critical issue in managing the various aspects of an epidemic, such as social and economic costs. Other non-drug actions, such as locking down the people, result in business closures during pandemic peaks, resulting in a financial loss for shopkeepers and retailers until they are vaccinated. As a result, delaying vaccination of certain groups, such as business owners, will have a significant economic impact and a social cost.
Our primary aim for developing a novel mathematical model to evaluate different priority strategies was to address this challenge. We suggest a parallel vaccination technique that attempts to reduce the social and economic costs of store closure and the expense of vaccine procurement. Designing a new vaccination approach, for example, will assist policymakers in dealing with both the development of infectious diseases and the economic impacts of quarantine at the same time. In addition, we investigate the effect of mandatory use of face masks on the required number of vaccine doses.
The rest of the paper is laid out as follows. In the second section, we go over the relevant literature. The terminology, assumptions, and proposed model are described in “Problem description”. The solution approach offered to solve the model is described in “Solution approach”. In “Computational results”, various numerical examples are given which validate the created model through computation and simulation. Finally, “Conclusion” brings the paper to a conclusion.
Literature review
Infectious diseases are a leading cause of morbidity and mortality worldwide. An epidemic is defined as a disease over the typical life expectancy [11]. As a result of a new epidemic that began in 2019, the world is currently coping with the COVID-19 epidemic. The first stage in controlling an epidemic is to defining the disease’s epidemic model as a dynamic system and forecasting the number of infected people to aid decision-makers in controlling the outbreak using the appropriate measures [12, 13]. An epidemic model is a simplified method for understanding how infectious diseases spread from person to person. It is required to gather thorough knowledge about the disease from a group of experts, to model the dynamics of a disease [14].
For modeling the dynamics of COVID-19, several researchers provide an alternative epidemic model. Buckner and Chowell [15] adopt a compartmental model-to-model transmission dynamics, including pre-symptomatic, asymptomatic, and symptomatic people. They focus on mortality, specifically years of life lost (YLL) and deaths. Zou and Wang [16] present a new epidemic model for predicting COVID-19 transmission in the United States at the national and state levels. They suggest the SuEIR epidemic model, a variation of the SEIR (susceptible–exposed–infected–removed) epidemic model that considers untested/unreported COVID-19 cases. In addition to hospitalized patients, they consider pre-symptomatic, asymptomatic, and symptomatic infected individuals. Choi, Kim [17] offer an age-structured mathematical model to describe the transmission patterns of COVID-19 with immunization in eight different age groups.
Pal, Ghosh [18] describe the COVID-19 outbreak using the SEQIR pandemic model, in which infected but undiagnosed individuals are quarantined for the duration of the incubation period. The basic reproduction number and the thorough stability analysis are used to show the dynamics of the SEQIR model. The estimated number of cases directly generated by one case in a population where all individuals are vulnerable to infection is the basic reproduction number. It is influenced by several factors, including the sick person’s duration of infection, the microorganism’s infectiousness, and the number of susceptible people in the population that the infected person contacts. Korolev [19] also investigates the SEIRD epidemic model for COVID-19, which is poorly detected using short-term data on death and reported cases. He argues that the evidence available is insufficient to identify which epidemic model is most appropriate for COVID-19.
Guerstein, Romeo-Aznar [20] propose a control model that combines social separation and immunization. They create a deterministic compartmental model to reflect the stages of COVID-19 progression and, as a result, to demonstrate the outcomes of deploying such technologies. Non-vaccinated people have become infected after the vaccination was implemented during the epidemic. As a result, social separation can aid in flattening the curve of infection.
In addition to the deterministic epidemic models, several scholars have presented stochastic epidemic models that are more complex but allow for the study of multiple aspects of epidemics [21,22,23].
The prioritization of people in the epidemic model is another concern of the researchers in the immunization programs. Individual prioritizing needs to be paid more attention to different conditions of epidemics and when the supply of effective vaccines is low. When an endemic disease strikes in the aftermath of an outbreak, Gamchi, Torabi [24] provide a mathematical model to prioritize the affected people for vaccination. They use an SIR epidemic model to determine how long each priority group will wait for vaccination. In light of the limited supply of vaccines in various countries, Hezam, Nayeem [25] provide 4 primary criteria and 15 sub-criteria based on age, health status, and job prioritizes persons. They use a neutrosophic AHP to analyze these parameters and identify which groups should first get immunized with the COVID-19 vaccine. In addition, Markovič, Šterk [26] investigate the impact of people’s health status on the vaccine distribution. Using an extended stochastic SEIR epidemic model, their results show that the rate of vaccination (i.e., the number of individuals vaccinated per day) and the availability of vaccine doses, as well as the health status of the vaccinated people, influence the chosen scenario of prioritization to cope with the COVID-19 epidemic. Foy, Wahl [27] provide a mathematical model for allocating vaccines based on restricted resources to reduce COVID-19-related morbidity and death and the effects of non-pharmaceutical therapies. Yang, Zheng [28] explore the primary framework to estimate the China’s critical target priority group and group size to reduce COVID-19-related mortality and break the disease’s transmission chain.
Chapman, Shukla [29] compare five alternative COVID-19 vaccine allocation strategies. Random allocation is one of these tactics, specific demographic targeting, age-based targeting, important worker targeting, and comorbidity targeting. To determine the appropriate immunization method, they look at one risk factor and two risk factors. Ferranna, Cadarette [30] use the age-stratified susceptible–exposed–infectious–recovered (SEIR) model to evaluate COVID-19 vaccination prioritization options and find that prioritizing essential workers reduces the number of mortalities in well-controlled pandemic scenarios. Notably, in determining the best strategy of prioritization, the vaccination uptake should be considered because, there are many factors and parameters that affect the decision by individuals to take the vaccine. Considering the limited source of COVID-19 vaccine, Piraveenan, Sawleshwarkar [31] explore the parameters that affect the decision-making process of individuals to receive the vaccine, and the decision-making process of government to choose the vaccines.
We also go at the literature on the mathematical models that have been proposed. Many studies have proposed a mathematical model to anticipate COVID-19 cases. They also look into the impact of non-pharmaceutical interventions (NPIs) such as lockdowns, social distancing, and other similar techniques [32,33,34]. It should be noted that removing the NPIs should be gradually. Czypionka and Iftekhar [35] investigate different strategies to remove the NPIs like lockdown policy and the case of Europe shows that low incidence strategy and high incidence strategy have different impacts on public health, society and economy. Kohli, Maschio [36] use a Markov cohort model to estimate direct medical expenses and deaths associated with COVID-19 in the United States, both with and without a 60% effective vaccination. They look at three different categories of people based on their age, risk and age, and occupation and age. They use cost-effectiveness analysis to compute the incremental cost per quality-adjusted life-year (QALY) and establish the optimum vaccination priority method.
Gap analysis
The use of the epidemic models to predict disease spread is one of its most critical applications. As a result, many academics concentrate on epidemic models that best fit many epidemics. The study employs several current criteria to rank persons and assesses them using various methods. In contrast, it is critical to predict a disease’s dynamic behavior, taking epidemic models into account when constructing a mathematical optimization model could aid policymakers in making essential judgments about disease behavior.
Although numerous forms of vaccine prioritizing study have been conducted, all the previous studies have shortcomings in examining the function of epidemic models in maximizing objectives such as social cost and economic impacts caused by COVID-19. In addition, the number of vaccination doses allocated to each priority group would be determined using a combination of epidemic models and mathematical optimization models, which is a flaw in earlier studies. As a result, this study aims to develop a new three-objective mathematical model for determining the optimal vaccination distribution among priority groups. We also investigate the mandatory use of face mask protocol in the number of vaccine doses allocated to different priority groups.
We believe that, in addition to the disease’s social cost, the economic impacts of business closures should be substantial for countries. As a result, the planners must devise a vaccine distribution strategy to deal with the disease’s many effects while working with a limited quantity of effective vaccine doses. The suggested three-objective model attempts to reduce the cost of vaccine procurement from various providers, the social cost incurred by infected individuals before and after vaccination, and the economic costs associated with store closures during the lockdown policy execution. To sum up, the main gaps in the engaged literature are as follows which, to the best of our knowledge, are not considered in previous research works:
-
Considering the economic impact of prioritizing the individuals to receive the COVID-19 vaccine, besides the social cost;
-
Investigating the effect of mandatory use of face masks on the epidemic’s control;
-
Developing a mathematical model to the optimal distribution of COVID-19’s vaccine among the priority groups.
Contribution
The immunization programs show that defining different groups with the same priority is necessary to cope with the pandemics like COVID-19, especially in the first stages, because the willingness of several age groups to receive the vaccine is different [37]. Therefore, this paper’s main contribution is to consider the parallel vaccination, which makes it different with other research papers in this context. On the other hand, many vaccine doses were wasted individually due to the vaccination process and declining of the individuals’ willingness to get vaccinated. For instance, according to ABC News, “millions of unused COVID-19 doses in the United States are set to go wasted as the country’s vaccination rates continued to decline amid an uptick of new infections.”Footnote 2 Thus, if the other priority group had the opportunity to receive the vaccine, the waste of vaccine doses would be reduced. As we investigate the effect of parallel prioritization of the individuals based not only on age but also on other factors like the economic effect of receiving COVID-19 vaccine.
Problem description
Infectious diseases transmission has various effects on social life, the economy, government costs, and small and medium-sized businesses. To deal with such issues, most governments have begun immunization programs. All countries’ priority plans are based on WHO recommendations. When all people of the first group have been vaccinated, the immunization of the second group begins and continues until all people have been immunized. As a result, those in various priority groups should wait to get vaccinated, as it may take too long to become immune to the disease.
On the other hand, numerous enterprises, malls, and retail stores must close due to government lockdown policies. In addition, among the retailers and shopkeepers that are not prioritized and lose the majority of their market during the pandemic, the ages of 30–49 years are the most common. As a result, a parallel vaccination approach to deal with business owners’ economic problems is required.
In this paper, we investigate how parallel vaccination among different priority groups and implementing the policy of using face masks affect the social cost of infected individuals from different priority groups and the economic cost imposed on business owners, shopkeepers, and retail stores during the implementation of lockdown policies and vaccine procurement costs. As a result, we offer a mathematical methodology for determining the best vaccine allocation to the priority groups, as well as putting the lockdown policy and other health regulations in place, like using face masks. The proposed model excludes health workers at a high or extremely high risk of acquiring and transmitting infection. This group needs to be vaccinated as soon as possible, and we provide a strategy for assigning the remaining vaccines. Adults over the age of 65, people between the ages of 50 and 64, and retailers are the key groups (the ages between 30 and 49 years have the most frequency among the retailers and shopkeepers). Even during the implementation of the lockdown policy, retailers might resume their activities following immunization. As a result, the COVID-19 pandemic’s economic impact would be reduced. In other words, removing non-pharmaceutical interventions like lockdown policy steadily is more achievable and advantageous for public health, society and economy [35]. The herd effect refers to the indirect protection of unvaccinated people, in which a rise in the prevalence of immunity caused by vaccination may result in a reduction in the vulnerable population surrounding infectious people [38]. Susceptible, exposed, quarantined, infected, and recovered are included in the considered epidemic model (Figs. 1 and 2) [18]. It should be considered that there are different epidemic models simulating the dynamicity of COVID-19. Since the main contribution of the paper is to investigate the effect of the parallel prioritization of individuals by considering the economic impact of lockdown policy, we use the SEQIR epidemic model for the sake of simplicity. Notably, while various priority groups share the same epidemic model, the rates in each group vary. In order to measure the social cost of infected people, the disability-adjusted life years (DALY) index is used. The cost of spreading a disease epidemic in unaffected areas by an infected individual as the host is included in the DALY [5, 39, 40].
SEQIR epidemic model of COVID-19 without control [18]. Given the transmission rates in the epidemic model, individuals’ states change when there are contacts among susceptible individuals and quarantined or exposed ones. Moreover, based on the severity of the disease, their states switch to infected or recovered. In addition, the natural death rate or death rate of infected individuals affects the number of individuals in each state. Different compartments, including susceptible, exposed, quarantined, infected, and recovered, are shown in the figure. The transmission rates between the compartments, the natural death rate, and the death rate due to the COVID-19 are presented. Notably, this figure shows the dynamic of the disease before using the control tools
SEQIR epidemic model of COVID-19 considering control variables. Compared to Fig. 1, when there is a control tool such as vaccination, some susceptible individuals get immune to the disease. They move to the recovered individuals decreasing the number of exposed, quarantined, or infected ones. In addition, using a face mask protects the susceptible individuals against the disease, reducing their number. This figure is the same as the previous one, and the difference is that the effect of using the control tools is considered
Notations
Indices
\(i\) | Index of suppliers (\(i=1,\dots ,n)\) |
\(j\) | Index of priority groups (\(j=1,\dots ,m)\) |
\(l\) | Index of businesses that affected by lockdown policy (\(l=1, ..., P)\) |
Parameters
\({p}_{i}\) | Price of each vaccine dose from supplier \(i\) |
\({K}_{i}\) | Capacity of supplier \(i\) |
\({C}_{l}^{ld}\) | Cost of locking down business \(l\) |
\({SC}_{j}\) | Social cost caused by infected individuals of the group \(j\) |
\({S}_{1,j}(t)\)(\({S}_{2,j}(t)\)) | Number of susceptible individuals of the group \(j\) before vaccination (after vaccination) at time \(t\) |
\({E}_{1,j}(t)\)(\({E}_{2,j}(t)\)) | Number of exposed individuals of the group \(j\) before vaccination (after vaccination) at time \(t\) |
\({Q}_{1,j}(t)\)(\({Q}_{2,j}(t)\)) | Number of quarantined individuals of the group \(j\) before vaccination (after vaccination) at time \(t\) |
\({I}_{1,j}(t)\)(\({I}_{2,j}(t)\)) | Number of infected individuals of the group \(j\) before vaccination (after vaccination) at time \(t\) |
\({R}_{1,j}\left(t\right)\left({R}_{2,j}\left(t\right)\right)\) | Number of recovered individuals of the group \(j\) before vaccination (after vaccination) at time \(t\) |
\(\mu_{j}\) | The recruitment rate of priority group j |
\(\alpha_{j}\) | The transmission rate from susceptible population to infected of priority group \(j\) but not detected by testing population |
\(\beta_{j}\) | The transmission rate from susceptible population to quarantine population of priority group \(j\) |
\(\beta ^{\prime}_{j}\) | The transmission rate from infected but not detected by testing population to quarantine population of priority group \(j\) |
\(\sigma_{j}\) | The transmission rate from infected but not detected by testing population to secured zone population of the priority group \(j\) |
\(\sigma ^{\prime}_{j}\) | The transmission rate from quarantine population to secured zone population of priority group \(j\) |
\(r_{j}\) | The transmission rate from infected but not detected by testing population to infected population of priority group \(j\) for treatment |
\(r^{\prime}_{j}\) | The transmission rate from quarantine population to infected population of priority group \(j\) for treatment |
\(d_{j}\) | The natural death rate of all sub-populations in priority group \(j\) |
\(d^{\prime}_{j}\) | The death rate of infected population due to COVID-19 in priority group \(j\) |
\({\mathcal{R}}_{0,j}\) | Basic reproduction number of the priority group \(j\) |
\(T_{j}^{end}\) | The time at which the epidemic in the priority group \(j\) ends |
\(C^{v}\) | Fixed cost of the vaccination program |
\(C^{F}\) | Fixed cost of implementing the policy of using a face mask |
\(\tau_{j}\) | Start time of the priority group \(j\)’s vaccination |
Decision variables
\({V}_{i}\) | Number of vaccine doses supplied by the supplier \(i\) |
\({u}_{1,j}\) | The proportion of susceptible individuals of the priority group \(j\) that are vaccinated per unit time |
\({u}_{2,j}\) | The proportion of susceptible individuals of the priority group \(j\) that are required to use face mask |
\({D}_{j}\) | Number of vaccine doses required to immunize the priority group \(j\) |
The developed decision models
The proposed three-objective model attempts to reduce vaccine procurement costs, total social costs incurred by infected individuals from various priority groups before and after vaccination, and the economic cost of shop closures simultaneously. As a result, determining the best time to immunize each priority group and the number of vaccine doses allotted to each group is essential. We consider the vaccination and using the face mask as the control tool.
The first objective’s main goal is to keep the cost of reducing or increasing vaccination intensity as low as possible:
Equation (1) represents the total cost of procuring vaccines from various vendors. We evaluate different pricing for the supplied vaccines because vaccine prices vary depending on the vaccine type and brand. The cost of vaccine doses should impact on the number of doses delivered by the supplier. The role of this objective function is to consider the limited resource of vaccines with different prices, which affects the total amount of vaccine doses assigned to different priority groups.
The second goal is to reduce the social cost of infected people before and after vaccination, considering different priority groups:
The first term in Eq. (2) reflects the social cost of priority group members infected prior to immunization. The second term is the cost after immunization, as previously stated. The third term is the vaccination cost when considering the optimal variable, and the last one is the cost of implementing the use of face masks as a health protocol. The third and fourth terms, in particular, try to maximize the number of recovered people while employing the minor possible control variable. The square of the control variables measures the severity of vaccination and face mask using side effects [2]. Because of \(0 \le u(t) \le 1\), we use the squared value of the control variables to lessen the effect of vaccine cost and cost of implementing the using face mask policy in the overall social cost. In addition, each immunization program’s fixed cost of vaccination comprises the cost of healthcare team members, vaccine maintenance costs in the central depot, and cold chain equipment costs [24].
The last objective function aims to reduce the economic impact of shop closures. Closing a store during the implementation of a lockdown policy puts a cost of closure on the retailer based on the type of business. As a result, the third objective, in conjunction with the other purposes, assists policymakers in determining when such a priority group should be vaccinated. In the other words, we consider the economic impact of lockdown policy besides the social cost (in the \(Z2\)) for the priority group of shopkeepers who encounter the cost of shop closure. Considering such an objective function leads to assigning some vaccine doses to the shopkeepers as a priority group and, consequently, removing different restrictions such as a lockdown policy:
As a result of the lockdown prior to the vaccination, the cost imposed on businesses is denoted by the first term in Eq. (3). It should be noted that the number of susceptible, exposed, quarantined and infected individuals in the priority group of shopkeepers and business owners affect the lockdown cost and consequently the economic impact of that policy. The second term is the cost imposed on the firm due to retailer infection. The length of the lockdown policy determines the cost imposed on the business. For simplicity, we use the following linear function for the mentioned cost:
There is an epidemic model without a control tool before each priority group is vaccinated, and the infected individuals recover naturally. The epidemic model’s differential equations would be as follows: Eqs. (5–9). The rates of being susceptible, exposed, quarantined, infected, and recovered are all represented by such equations:
When each priority group receives the needed dosage of vaccine and the immunization program begins, the epidemic model shifts in viewing vaccination as a control strategy. As a result, we would have Eqs. (10–14). It is notable that, in Eqs. (11) and (12), since the individuals of different priority groups are not isolated, there is contact between susceptible individuals in priority group j and exposed ones in all the priority groups we use the summation of \({E}_{2,j}(t)\) (i.e., \({\alpha }_{j}{S}_{2,j}\left(t\right){\sum }_{j=1}^{m}{E}_{2,j}(t)\)):
Constraint Eq. (16) states that we must provide enough vaccine doses for all priority groups to control an infectious disease outbreak. Notably, a group’s demand for a vaccine depends on the optimal control tool’s value, the number of susceptible individuals in the group, and the vaccination time:
Finally, (17) denotes that provider i's capacity equals to the maximum number of vaccine doses it can supply:
Solution approach
The developed approach intends to reduce the socio-economic cost of infected people while also considering the costs imposed on retailers due to the countries’ lockdown policies. We also examine vendors with varied prices due to the limitations on procuring vaccinations from suppliers. As a result, another goal of this problem is to reduce vaccine supply procurement costs. Shamsi G, Ali Torabi [5] and Gamchi, Torabi [24] present some solutions for such multi-objective issues.
We use the most recent solution approach to solve the proposed model. To tackle the problem, we consider two different phases. We run the dynamics of the epidemic model in the first phase to determine the total number of vaccine doses required to control the epidemic disease. As a result, the following procedures are followed:
Step 1. Determine the basic reproduction number, \({\mathcal{R}}_{0,j}\), for each priority group, considering the disease type and transmission rate. We use the generation matrix to determine the value of the basic reproduction number:
We define two matrices of gain terms (F) and loss terms (V) according to Eqs. (5–9). Moreover, \({\mathcal{R}}_{0}\) is the dominant eigenvalue of \(G=F.{V}^{-1}\) as follows [18]:
Step 2. If \({\mathcal{R}}_{0,j}<1\) is true, no vaccine is required, and the group \(j\) is removed from the list of immunization programs. If not, proceed to Step 3.
Step 3. Run the epidemic model for the remaining priority groups in each region to see how many people are in each compartment of the epidemic model at any given time.
Step 4. Using the optimal control theory, determine the number of susceptible individuals in each priority group who may be eligible for vaccination, and the vaccine doses required to control the epidemic disease. In addition, at various time intervals, calculate the social cost of infected persons:
Notably, we apply Pontryagin’s maximum principle [41] to solve the optimal control problem by optimizing the Hamiltonian function. In addition, the considered objective function is as follows:
where \({wt}_{1}\) and \({wt}_{2}\) are the weight of objective functions 2 and 3, respectively, and \({wt}_{1}+{wt}_{2}=1\).
Theorem
If \({u}_{j}^{*}(t)\) is an optimal control variable corresponding to the optimal states of the priority group j, which minimize the single weighted-sum objective function (20), then there exist co-state variables \({\omega }_{1}(t)\) to \({\omega }_{5}(t)\) which satisfy
with the following transversality conditions:
Furthermore, the optimal control variables are:
where \({u}_{max}\) and \(u^{\prime}_{max}\) depends on the number of resources available to implement the control measure.
Proof
We form the Hamiltonian HAM as follows:
where \({\omega }_{1}(t)\) to \({\omega }_{5}(t)\) are the adjoint functions to be determined suitably. Using Pontryagin’s maximum principle, we would have:
Using the optimality conditions, we find
which results in
We obtain Eqs. (23) and (24) using the control space \(U = \{ u_{i} \left( t \right)|0 \le u_{i} \left( t \right) \le u_{{{\text{max}}}} \le 1, t \in \left[ {\tau_{{{\text{start}}}} , T_{{{\text{end}}}} } \right]\}\).
Step 5. By determining the required doses of vaccine for each priority group, we would have linear mathematical modeling to determine the number of vaccine doses ordered to each supplier. In addition, by determining the second control tool, we determine the period of using face masks to overcome the epidemic.
Computational results
This section uses a real-world scenario to assess the model’s and solution approach’s effectiveness. We also go over the numerical results to provide some managerial insights.
The case description
The COVID-19 outbreak in 2019 impacted people worldwide, and due to the virus’s rapid spread, no government was able to respond adequately. As a result, strategies such as lockdown must be introduced to limit the infectious disease’s morbidity and death. Even after the COVID-19 vaccine was discovered, governments were forced to impose a lockdown policy due to a limited vaccine supply and a prioritization system based on the age groups. They began a vaccination program with those over the age of 65 and continued with the other age groups until all people had been immunized. We propose a mechanism in this research to vaccinate individuals in parallel while dealing with the economic impacts of lockdown policies and disease transmission. Such programs might assist policymakers in similar situations in making informed decisions about parallel vaccination. In addition, we consider implementing a suing face mask policy to reduce disease transmission.
The proposed vaccination method for an infectious disease like COVID-19 is examined in this subsection. Tehran, Iran’s capital, serves as our example. Different age groups are investigated in the case study, including 50–65 years old (G1) and over 65 years old (G2). In addition, according to market statistics, Iran has 5 million retail units, with around 7% of them in Tehran. Each retail unit has an average of three people working in it. As a result, the group of shops and retailers would consist of 1,050,000 people with regard to Fig. 3.
In our case study, we have three different priority groups, including the two age groups described above, as well as a group of shopkeepers and retailers (G3).
Age group-based population of Tehran. The most populated age group in Tehran is the range of 25 to 39, which affects the immunization program’s efficiency if it is based on the age groups. A graph with vertical bars depicts the distribution of age groups in Tehran. The Y-axis is labeled as “No. of individuals,” and the X-axis is labeled as “Age groups,” ranging from 0–4 to 100+
It is worth noting that including shopkeepers and merchants as one of the priority groups could aid authorities in reducing the economic consequences of the lockdown strategy. As a result, the proposed model provides a basic framework for vaccine distribution that may be used for various priority groups and different types of epidemic diseases that affect people all over the country or the world. COVID-19 is used as a numerical example in this section. As a result, prior research is used to estimate various rates of the linked epidemic model, such as recruitment rate, transmission rate, recovery rate, etc. It should also be remembered that priority groups may have varying rates. Individuals over the age of 65, for example, are more likely to become infected and die than other adults. The parameters used in this paper are presented in Table 1. In addition, the government bears additional social costs for several priority groups. \(SC1=1200\$/\mathrm{individual}\), \(SC 2=1000\mathrm{\$}/\mathrm{individual}\), and \(SC 3=1300\$/\mathrm{individual}\) were chosen as the societal costs of infected people. It should be noted that different factors are considered when estimating the social cost of different priority groups, such as the cost of non-working people, the cost of healthcare services, and intervention implementation costs such as personnel salaries, infrastructure costs, and administrative costs [24, 40].
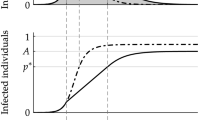
We also suppose a linear function of vaccination time for the cost of business lockdown (i.e., \({C}^{ld}\left({\tau }_{J}\right)=A{\tau }_{J}+B\)). In this case, we consider \(A=20\) and \(B=0\). Since, in Iran, vaccination started about 1 year after the disease outbreak. Therefore, the dynamic of the epidemic would be as Fig. 4.
Dynamics of the COVID-19 epidemic disease before using control tools. In the first weeks of infectious disease spread out, the number of susceptible individuals decreases because there are no health protocols like face masks. Consequently, the infection rate is high. During this time, the number of susceptible ones increase, and because of the death that occurred by the disease, the number of infected, recovered and exposed decrease. The status of each compartment over the 40 weeks before using the control tools is shown in the figure. There are five different graphs that each one is related to a compartment in the dynamic system
As shown in Fig. 4, the number of susceptible individuals increases because the number of people who can be infected increases. In addition, the number of quarantined individuals, at first, increases but then decreases. Notably, system’s dynamic at the first weeks differs a lot compared to the rest of the time.
When the vaccination is started and the policy of using face masks implemented strictly, the number of recovered individuals increases while the number of exposed and infected individuals decreases. As shown in Fig. 5, it should be noted that by implementing the control tools, including vaccinating the individuals and mandatory use of face masks, the number of exposed and infected individuals goes down.
Dynamics of the COVID-19 epidemic disease after vaccination and mandatory use of face mask as control tools. Using the face mask and vaccination of individuals, the number of susceptible individuals and, consequently, the number of exposed and infected ones decreases. In addition, the number of recovered individuals increases. The status of each compartment over the 50 weeks after using the control tools is shown in the figure. There are five different graphs that each one is related to a compartment in the dynamic system
The results show that the parallel vaccination of individuals helps policymakers decrease the social and business costs of the lockdown policy. We determine the total doses of vaccine to control the epidemic disease based on different priority groups.
Figure 6 shows that the mandatory use of face masks should last for about 49 weeks after vaccination to improve the effectiveness of the immunization program.
Control function of using face mask (priority group G1). This curve shows that mandatory use of the face mask long-term impacts on epidemic control. The graph shows the value of the second control tool, i.e., mandatory use of face mask, over time. The Y-axis is labeled as “using face mask as a control tool” and the X-axis is labeled as “Time (weeks),” which indicates the time of controlling the epidemic using this control variable
The disease among priority group G1 would be controlled 25 weeks after vaccination (Fig. 7). Moreover, the total required number of vaccine doses for immunization of this group is 3,295,617 doses. For the other priority groups, we would have the results as given in Table 2.
Control function of vaccinating (priority group G1). This figure shows the effect of vaccination, which controls the epidemic disease 25 weeks after starting the immunization program. Notably, mandatory use of face masks also influences the time of epidemic control. The graph shows the value of the first control tool, i.e., vaccination, over time. The Y-axis is labeled as “vaccination as a control tool,” and the X-axis is labeled as “Time (weeks),” which indicates the time of controlling the epidemic using this control variable
Therefore, the total number of vaccine doses and mandatory face masks will help the government control the epidemic without implementing a lockdown policy for retailers.
Now, based on the vaccine price and the production capacity of each supplier, the government can place an order for the required vaccine doses to minimize the procurement cost. Here, we suppose two different suppliers with different capacities and prices as follows:
Supplier 1: 3.7$ per dose with the capacity of 4 million doses;
Supplier 2: 2.15 $ per dose with the capacity of 3 million doses.
Here, we have a linear mathematical model to determine the best policy to place the order. We solve the problem using GAMs software, and the result is as follows: the minimum cost is achieved by 3 million doses from supplier 2 and 3,736,028 doses from supplier 1.
Sensitivity analysis and managerial insight
The need for parallel vaccination is discussed here, with shopkeepers and retailers being a priority group. The economic impact of the lockdown strategy in the COVID-19 epidemic is tremendous, and many retailers have lost revenue due to it. In other cases, the policy has harmed mental health [44]. As a result, when deciding on vaccine allocation, we should evaluate the social and economic implications of the lockdown policy.
We are now looking into the impact of parallel prioritization and comparing it to present policies (i.e., vaccination based on the age groups).
Since the cost of vaccination for shopkeepers and retailers is a linear function of the vaccination start time, the longer the vaccination start time, the higher the cost. As a result, the decision-maker should develop an acceptable plan for the timely vaccination of shopkeepers and merchants, as outlined in this paper. In addition, we investigate the effect of implementing the mandatory mask using policy on the number of susceptible individuals. As shown in Fig. 8, the mask using policy implementing has a significant role in decreasing the number of susceptible individuals leading to the sooner control of the epidemic.
Total social cost and economic cost without considering the parallel prioritization. The area under the curves shows the total social and economic costs in different situations. The total cost in the case of parallel vaccination is lower than the other situation. Two different graphs in the figure compare the number of susceptible individuals in two cases of using face masks and not using them, which affect the number of vaccines allocated to each group
Several factors can affect the decisions about implementing the health protocols such as vaccination and mask use. Here, we discuss the economic impact and the social cost of infected individuals to determine the best approach to assign the limited number of vaccine doses to the individuals and the duration of the mandatory use of face masks. The results show that the proposed ways of control would positively affect the costs imposed on the nations.
Conclusion
COVID-19 has spread worldwide, and all countries have implemented a lockdown policy as a swift response to stem the development of the epidemic. Many merchants will encounter financial difficulties due to this policy, and the GDP is expected to fall by 5.2% this year. As a result of this outbreak, lessons should be learned, leading to an acceptable pre-disaster plan for timely provision of essential vaccination doses post-disaster to control the spread of potentially l infectious illnesses. In determining the optimal values of the required vaccine doses for each priority group and the best way to assign vaccine doses to them, the paper contributes to the related literature in several ways, including considering the mandatory use of face masks and the impacts of vaccination as control tools and accounting for the burden of disease as the social cost. Another priority group, as well as age groupings, are presented in order to reduce the economic, social, and procurement costs of the lockdown policy. To accomplish so, we use a SEQIR epidemic model with varied rates for each priority category to predict the number of vaccine doses needed in the event of a resource shortage. To address the epidemic model problem, we utilize the optimal control strategy, and based on the required number of vaccine doses; we decide the number of doses ordered from each supplier. Finally, we solve the linear mathematical model using GAMs software to reduce purchase costs.
According to our numerical illustrations, policymakers’ actions can be changed by considering different priority groups. Because, in addition to the social cost of infected individuals, lockdown policy has a significant impact on the lives of many shopkeepers and retailers, and the nation’s economy, prioritizing groups other than age groups is critical in determining how vaccines are distributed. As a result, policymakers will be better able to deal with the epidemic and its consequences if they explore a parallel prioritizing strategy to reduce social, economic and procurement costs.
There are various ways to expand on the current work. We investigate a SEQIR epidemic model in this study without sacrificing generality. Other epidemic models based on various diseases can, however, be considered. Other control techniques, such as social distance and education, can also be modeled to determine the dynamicity of the epidemic. We use the vaccination price as a criterion for ordering from multiple vendors in our problem scenario, although other factors such as reliability might also be evaluated.
References
Ceylan, R.F., Ozkan, B., Mulazimogullari, E.: Historical evidence for economic effects of COVID-19, pp. 817–823. Springer (2020)
Laarabi, H., et al.: Optimal vaccination strategies of an sir epidemic model with a saturated treatment. Univ J Appl Math 1(3), 185–191 (2013)
Tognotti, E.: Lessons from the history of quarantine, from plague to influenza A. Emerg. Infect. Dis. 19(2), 254 (2013)
Khodabandeh, P., et al.: A bi-objective home health care routing and scheduling model with considering nurse downgrading costs. Int. J. Environ. Res. Public Health 18(3), 900 (2021)
Shamsi, G.N., Ali Torabi, S., Shakouri, H.G.: An option contract for vaccine procurement using the SIR epidemic model. Eur. J. Oper. Res. 267(3), 1122–1140 (2018)
Waring, S.C., Brown, B.J.: The threat of communicable diseases following natural disasters: a public health response. Disaster Manag. Response 3(2), 41–47 (2005)
Gashaw, T., Bisrat Hagos, M.S.: Expected impacts of COVID-19: considering resource-limited countries and vulnerable population. Front Public Health (2021). https://doi.org/10.3389/fpubh.2021.614789
Li, Z., et al.: Active case finding with case management: the key to tackling the COVID-19 pandemic. Lancet 396(10243), 63–70 (2020)
Straetemans, M., et al.: Prioritization strategies for pandemic influenza vaccine in 27 countries of the European Union and the Global Health Security Action Group: a review. BMC Public Health 7(1), 236 (2007)
Lee, B.Y., et al.: A computer simulation of vaccine prioritization, allocation, and rationing during the 2009 H1N1 influenza pandemic. Vaccine 28(31), 4875–4879 (2010)
Imane, E., Jamal, B., Abdelouahed, N.: Dissemination of epidemic for SIR model. J Math Sci 7(136), 6793–6800 (2013)
Abbasimehr, H., Paki, R., Bahrini, A.: A novel approach based on combining deep learning models with statistical methods for COVID-19 time series forecasting. Neural Comput Applic (2021). https://doi.org/10.1007/s00521-021-06548-9
Wang, M., Flessa, S.: Modelling Covid-19 under uncertainty: what can we expect?, pp. 665–668. Springer (2020)
Malmir, B., Amini, M., Chang, S.I.: A medical decision support system for disease diagnosis under uncertainty. Expert Syst. Appl. 88, 95–108 (2017)
Buckner, J.H., Chowell, G., Springborn, M.R.: Optimal dynamic prioritization of scarce COVID-19 vaccines (2020). https://doi.org/10.1101/2020.09.22.20199174
Zou, D., et al.: Epidemic model guided machine learning for COVID-19 forecasts in the United States (2020). https://doi.org/10.1101/2020.05.24.20111989
Choi, Y., et al.: Vaccination prioritization strategies for COVID-19 in Korea: a mathematical modeling approach. Int. J. Environ. Res. Public Health 18(8), 4240 (2021)
Pal, D., et al.: Mathematical analysis of a COVID-19 epidemic model by using data driven epidemiological parameters of diseases spread in India (2020). https://doi.org/10.1101/2020.04.25.20079111
Korolev, I.: Identification and estimation of the SEIRD epidemic model for COVID-19. J Econom 220(1), 63–85 (2021)
Guerstein, S., et al.: Optimal strategies for combining vaccine prioritization and social distancing to reduce hospitalizations and mitigate COVID19 progression (2020). https://doi.org/10.1101/2020.12.22.20248622
Bardina X, Ferrante M, Rovira C (2020) A stochastic epidemic model of COVID-19 disease. arXiv preprint arXiv:2005.02859.
Hussain, G., et al.: Modeling the dynamics of novel coronavirus (COVID-19) via stochastic epidemic model. Alex. Eng. J. 60(4), 4121–4130 (2021)
Rihan, F.A., Alsakaji, H.J., Rajivganthi, C.: Stochastic SIRC epidemic model with time-delay for COVID-19. Adv. Difference Equ. 2020(1), 1–20 (2020)
Shamsi Gamchi, N., Torabi, S.A., Jolai, F.: A novel vehicle routing problem for vaccine distribution using SIR epidemic model, pp. 1–34. OR Spectrum (2020)
Hezam, I.M., et al.: COVID-19 Vaccine: A neutrosophic MCDM approach for determining the priority groups. Results in Physics 20, 103654 (2021)
Markovič, R., et al.: Socio-demographic and health factors drive the epidemic progression and should guide vaccination strategies for best COVID-19 containment. Results Phys 26, 104433 (2021)
Foy, B.H., et al.: Comparing COVID-19 vaccine allocation strategies in India: a mathematical modelling study. Int. J. Infect. Dis. 103, 431–438 (2021)
Yang, J., et al.: Who should be prioritized for COVID-19 vaccination in China? A descriptive study. BMC Med. 19(1), 45 (2021)
Chapman, L.A.C., et al.: Risk factor targeting for vaccine prioritization during the COVID-19 pandemic. Sci. Rep. 12, 3055 (2022). https://doi.org/10.1038/s41598-022-06971-5
Ferranna, M., Cadarette, D., Bloom, D.E.: COVID-19 vaccine allocation: modeling health outcomes and equity implications of alternative strategies. Engineering (2021). https://doi.org/10.1016/j.eng.2021.03.014
Piraveenan, M., et al.: Optimal governance and implementation of vaccination programmes to contain the COVID-19 pandemic. R Soc Open Sci 8(6), 210429 (2021)
Jewell, N.P., Lewnard, J.A., Jewell, B.L.: Predictive mathematical models of the COVID-19 pandemic: underlying principles and value of projections. JAMA 323(19), 1893–1894 (2020)
Ndaïrou, F., et al.: Mathematical modeling of COVID-19 transmission dynamics with a case study of Wuhan. Chaos Solitons Fractals 135, 109846 (2020)
Sardar, T., et al.: Assessment of lockdown effect in some states and overall India: a predictive mathematical study on COVID-19 outbreak. Chaos Solitons Fractals 139, 110078 (2020)
Czypionka, T., et al.: The benefits, costs and feasibility of a low incidence COVID-19 strategy. Lancet Reg Health Eur 13, 100294 (2022)
Kohli, M., et al.: The potential public health and economic value of a hypothetical COVID-19 vaccine in the United States: use of cost-effectiveness modeling to inform vaccination prioritization. Vaccine 39(7), 1157–1164 (2021)
Afifi, T.O., et al.: Older adolescents and young adults willingness to receive the COVID-19 vaccine: implications for informing public health strategies. Vaccine 39(26), 3473–3479 (2021)
Kim, T.H., Johnstone, J., Loeb, M.: Vaccine herd effect. Scand. J. Infect. Dis. 43(9), 683–689 (2011)
Brent, R.J.: An implicit price of a DALY for use in a cost-benefit analysis of ARVs. Appl. Econ. 43(11), 1413–1421 (2011)
Neumann, P.J., et al.: A systematic review of cost-effectiveness studies reporting Cost-per-DALY averted. PLoS ONE. 11(12), e0168512 (2016). https://doi.org/10.1371/journal.pone.0168512
Pontryagin, L.S.: Mathematical theory of optimal processes. CRC Press (1987)
Shah, N.H., et al.: Fractional SIR-model for estimating transmission dynamics of COVID-19 in India. Journal 4(2), 86–100 (2021)
Semenova, Y., et al.: Epidemiological characteristics and forecast of COVID-19 outbreak in the Republic of Kazakhstan. J. Korean Med. Sci. 35(24), e227 (2020). https://doi.org/10.3346/jkms.2020.35.e227
Droit-Volet, S., et al.: Time and Covid-19 stress in the lockdown situation: time free,«Dying» of boredom and sadness. PLoS One 15(8), e0236465 (2020)
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shamsi Gamchi, N., Esmaeili, M. A novel mathematical model for prioritization of individuals to receive vaccine considering governmental health protocols. Eur J Health Econ 24, 633–646 (2023). https://doi.org/10.1007/s10198-022-01491-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-022-01491-5
Keywords
- Infectious disease
- SEQIR epidemic model
- Vaccine allocation
- Parallel prioritization
- Mandatory use of face mask
- Optimal control