Abstract
Background
Potential benefits of single-port laparoscopic surgery may include improved cosmetic results, less postoperative pain, surgical trauma and faster recovery. Results of randomized prospective studies with a focus on single-port rectal surgery have not yet been presented. The aim of the present study was to compare single-port and conventional laparoscopic surgery for rectal cancer in terms of short-term outcomes including postoperative pain and trauma-induced changes in certain bioactive substances.
Methods
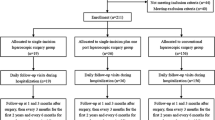
Patients with non-metastasized rectal cancer were prospectively randomized to single-port (n = 20) or conventional laparoscopic rectal surgery (n = 20). Postoperative pain was assessed at rest, at coughing and during mobilization, with a numeric pain ranking score and was recorded at 6 h after the operation and subsequently every morning daily for 4 days. Levels of C-reactive protein (CRP), interleukin-6 (IL-6) and tissue inhibitor of metalloproteinases-1 (TIMP-1) were determined. Blood samples were collected preoperatively (baseline), and 6, 24, 48, 72 and 96 h after skin incision.
Results
Pain scores were significantly reduced in the single-port group on postoperative days 2, 3 and 4 during coughing and mobilization. In addition, the patients in the single-port group suffered significantly less pain at rest at 6 h after surgery and on postoperative days 1, 3 and 4. The levels of the three markers increased significantly after surgery. The increase was similar between groups for plasma IL-6 and TIMP-1 at all time points, while the CRP levels were significantly lower in the single-port group at 6 (p < 0.001) and 24 h (p < 0.05) after skin incision. Abdominal incisions lengths were significantly shorter in the single-port group (p = 0.001). There was no significant difference between groups in operating time and blood loss, morbidity or mortality rate. The short-term oncological outcome in the two groups was similar.
Conclusions
Single-port rectal surgery may reduce postoperative pain. Although CRP levels were lower at some time points, results of the present randomized, pilot study suggest that the trauma-induced inflammatory response of single-port operations may be similar to the trauma-induced inflammatory response of conventional laparoscopic surgery.



Similar content being viewed by others
References
Waters JA, Rap BM, Guzman MJ et al (2012) Single-port laparoscopic right hemicolectomy: the first 100 resections. Dis Colon Rectum 55:134–139
Ramos-Valadez DI, Ragupathi M, Nieto J et al (2012) Single-incision versus conventional laparoscopic sigmoid colectomy: a case-matched series. Surg Endosc 26:96–102
Champagne BJ, Lee EC, Leblanc F, Stein SL, Delaney CP (2011) Single-incision vs straight laparoscopic segmental colectomy: a case-controlled study. Dis Colon Rectum 54:183–186
Vestweber B, Galetin T, Lammerting K et al (2013) Single-incision laparoscopic surgery: outcomes from 224 colonic resections performed at a single center using SILS. Surg Endosc 27:434–442
Kehlet H (1999) Surgical stress response: does endoscopic surgery confer an advantage? World J Surg 23:801–807
Allendorf JD, Bessler M, Horvath KD et al (1999) Increased tumor establishment and growth after open vs laparoscopic surgery in mice may be related to differences in postoperative T-cell function. Surg Endosc 13:233–235
Nielsen HJ (1995) The effect of histamine type-2 receptor antagonists on posttraumatic immune competence. Dan Med Bull 42:162–174
Van der Bij GJ, Oosterling SJ, Beelen RH, Meijer S, Coffey JC, van Egmond M (2009) The perioperative period is an underutilized window of therapeutic opportunity in patients with colorectal cancer. Ann Surg 249:727–734
Mynster T, Christensen IJ, Moesgaard F, Nielsen HJ (2000) Effects of the combination of blood transfusion and postoperative infectious complications on prognosis after surgery for colorectal cancer. Danish RANX05 Colorectal Cancer Study Group. Br J Surg 87:1553–1562
Lin E, Calvano SE, Lowry SF (2000) Inflammatory cytokines and cell response in surgery. Surgery 127:117–126
Paterson-Brown S, Garden OJ, Carter DC (1991) Laparoscopic cholecystectomy. Br J Surg 78:131–132
Bruce DM, Smith M, Walker CB et al (1999) Minimal access surgery for cholelithiasis induces an attenuated acute phase response. Am J Surg 178:232–234
Ohzato H, Yoshizaki K, Nishimoto N et al (1992) Interleukin-6 as a new indicator of inflammatory status: detection of serum levels of interleukin-6 and C-reactiv protein after surgery. Surgery 111:201–209
Soda K, Kano Y, Kawakami M et al (2003) Excessive increase of serum interleukin-6 jeopardizes host defence against multibacterial infection. Cytokine 21:295–302
Frederiksen C, Lomholt AF, Davis GJ et al (2009) Changes in plasma TIMP-1 levels after resection for primary colorectal cancer. Anticancer Res 29:75–82
Targarone EM, Pons MJ, Balague C et al (1996) Acute phase is the only significantly reduced component of the injury response after laparoscopic cholecytectomy. World J Surg 20:528–534
Sietses C, Wiezer MJ, Eijsbouts QAJ et al (1999) A prospective randomised study of systemic immune response after laparoscopic and conventional Nissen fundoplication. Surgery 126:5–9
Liu C, Liu J, Zhang S (2011) Laparoscopic versus conventional open surgery for immune function in patients with colorectal cancer. Int J Colorectal Dis 26:1375–1385
Maggiori L, Gaujoux S, Tribillon T et al (2012) Single-incision laparoscopy for colorectal resection: a systematic review and meta-analysis of more than a thousand procedures. Colorectal Dis 14:e643–e654
Huscher CG, Mingoli A, Sgarzini G et al (2012) Standard laparoscopic versus single-incision laparoscopic colectomy for cancer: early results of a randomized prospective study. Am J Surg 204:115–120
Poon JT, Cheung CW, Fan JK, Lo OS, Law WL (2012) Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc 26:2729–2734
DCCG Guidelines 4th edition (2009) http://www.dccg.dk/10_English/0010_English.html
Basse L, Jakobsen DH, Billesbølle P et al (2000) A clinical pathway to accelerate recovery after colonic resection. Ann Surg 232:51–57
Aslak KA, Bulut O (2012) The implementation of a standardized approach to laparoscopic rectal surgery. JLSL 16:264–270
Bulut O, Aslak KA, Rosenstock S (2013) Technique and short-term outcomes of single-port surgery for rectal cancer: a feasibility study of 25 patients. Scand J Surg 103:26–33
Sørensen NM, Sørensen IV, Würtz SØ et al (2008) Biology and potential clinical implications of tissue inhibitor of metalloproteinases-1 in colorectal cancer treatment. Scand J Gastroenterol 43:774–786
Lu CC, Lin SE, Chung KC, Rau KM (2012) Comparison of clinical outcome of single-incision laparoscopic surgery using simplified access system with conventional laparoscopic surgery for malignant colorectal disease. Colorectal Dis 14:e171–e176
Kim S-J, Ryu G-O, Kim J-G, Lee K-J, Lee S-C, Oh S-K (2011) The short term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg 254:933–940
Papaconstantinou HT, Sharp N, Thomas JS (2011) Single-incision right colectomy: a case-matched comparison with standard laparoscopic and hand-assisted laparoscopic techniques. J Am Coll Surg 213:72–80
Hammar JH, Basse L, Svendsen MN et al (2006) Impact of elective resection on plasma TIMP-1 levels in patients with colon cancer. Colorectal Dis 8:168–172
Froghi F, Sodergren MH, Wright VJ et al (2011) Single-center experience in systemic stress and short term morbidity of single-incision cholecystectomy. Surg Innovation 19:1–6
Chaudhary D, Verma GR, Gupta R et al (1999) Comparative evaluation of the inflammatory mediators in patients undergoing laparoscopic versus conventional cholecystectomy. Aus N Z J Surg 69:369–372
Veenhof AAFA, Vlug MS, van der Pas MHGM et al (2012) Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care. A Randomized trial. Ann Surg 2:216–221
Veenhof AAFA, Sietses C, von Blomberg BME et al (2011) The surgical stress response and postoperative immune function after laparoscopic or conventional total mesorectal excision in rectal cancer: a randomized trial. Int J Colorectal Dis 26:53–59
Osborne A, Lim J, Gash KJ, Chaudhary B, Dixon AR (2013) Single-incision and standard laparoscopic high anterior resection compared. Colorectal Dis 15:329–333
Ahmed K, Wang TT, Patel VM et al (2011) The role of single-incision laparoscopic surgery in abdominal and pelvic surgery: a systematic review. Surg Endosc 25:378–396
Fung AK-Y, Aly EH (2012) Systematic review of single-incision laparoscopic colonic surgery. Br J Surg 99:1353–1364
Acknowledgments
The authors are indebted to research nurse Cathrine H. Bachmann for help with blood sample collection and handling. The authors would also like to express our gratitude to Nicolai B. Foss, MD, DMSc from the Department of Anaesthesiology for his advice and review of the manuscript. Funding for this work was received from: The Kornerup Fund, The Aase and Ejnar Danielsen Fund, The Kathrine and Vigo Skovgaard Fund.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bulut, O., Aslak, K.K., Levic, K. et al. A randomized pilot study on single-port versus conventional laparoscopic rectal surgery: effects on postoperative pain and the stress response to surgery. Tech Coloproctol 19, 11–22 (2015). https://doi.org/10.1007/s10151-014-1237-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-014-1237-6