Abstract
Objective
This study aimed to explore the prognostic value of mean platelet volume (MPV) in patients with ovarian clear cell carcinoma (OCCC) and evaluate the predictive performance of a random forest model incorporating MPV and other key clinicopathological factors.
Methods
A total of 204 patients with OCCC treated between January 2004 and December 2019 were retrospectively analyzed. Clinicopathological characteristics and preoperative laboratory data were collected, and survival outcomes were evaluated using the Kaplan–Meier method and Cox proportional hazards models. An optimal MPV cutoff was determined by receiver operating characteristic (ROC) curve analysis. A random forest model was then constructed using the identified independent prognostic factors, and its predictive performance was evaluated.
Results
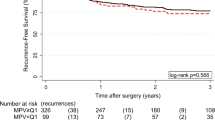
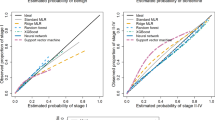
The ROC analysis identified 9.3 fL as the MPV cutoff value for predicting 2-year survival. The MPV-low group had lower 5-year overall survival and progression-free survival rates than the MPV-high group (p = 0.003 and p = 0.034, respectively). High MPV emerged as an independent prognostic factor (p = 0.006). The random forest model, incorporating the FIGO stage, residual tumors, peritoneal cytology, and MPV, demonstrated robust predictive performance (area under the curve: 0.905).
Conclusion
MPV is a promising prognostic indicator in OCCC. Lower MPV correlated with worse survival rates, advocating its potential utility in refining patient management strategies. The commendable predictive performance of the random forest model, integrating MPV and other significant prognostic factors, suggests a pathway toward enhanced survival prediction, thereby warranting further research.


Similar content being viewed by others
References
Shu CA et al (2015) Ovarian clear cell carcinoma, outcomes by stage: the MSK experience. Gynecol Oncol 139(2):236–241
del Carmen MG, Birrer M, Schorge JO (2012) Clear cell carcinoma of the ovary: a review of the literature. Gynecol Oncol 126(3):481–490
Bookman MA et al (2014) Better therapeutic trials in ovarian cancer. J Natl Cancer Inst 106(4):dju029
Tan DS, Kaye S (2007) Ovarian clear cell adenocarcinoma: a continuing enigma. J Clin Pathol 60(4):355–360
Sugiyama T et al (2000) Clinical characteristics of clear cell carcinoma of the ovary: a distinct histologic type with poor prognosis and resistance to platinum-based chemotherapy. Cancer 88(11):2584–2589
Chan JK et al (2008) Do clear cell ovarian carcinomas have poorer prognosis compared to other epithelial cell types? A study of 1411 clear cell ovarian cancers. Gynecol Oncol 109(3):370–376
Tammela J et al (1998) Clear cell carcinoma of the ovary: poor prognosis compared to serous carcinoma. Eur J Gynaecol Oncol 19(5):438–440
Bancroft AJ et al (2000) Mean platelet volume is a useful parameter: a reproducible routine method using a modified coulter thrombocytometer. Platelets 11(7):379–387
Repsold L, Joubert AM (2021) Platelet function, role in thrombosis, inflammation, and consequences in chronic myeloproliferative disorders. Cells 10(11):3034
Gay LJ, Felding-Habermann B (2011) Contribution of platelets to tumour metastasis. Nat Rev Cancer 11(2):123–134
Wojtukiewicz MZ et al (2017) Platelets and cancer angiogenesis nexus. Cancer Metastasis Rev 36(2):249–262
Takagi S et al (2013) Platelets promote tumor growth and metastasis via direct interaction between aggrus/podoplanin and CLEC-2. PLoS ONE 8(8):e73609
Kharel S et al (2022) Prognostic significance of mean platelet volume in patients with lung cancer: a meta-analysis. J Int Med Res 50(3):3000605221084874
Li N et al (2017) Elevated mean platelet volume predicts poor prognosis in colorectal cancer. Sci Rep 7(1):10261
Omar M et al (2018) Role of increased mean platelet volume (MPV) and decreased MPV/platelet count ratio as poor prognostic factors in lung cancer. Clin Respir J 12(3):922–929
Yagyu T et al (2021) Decreased mean platelet volume predicts poor prognosis in patients with pancreatic cancer. BMC Surg 21(1):8
Delago D et al (2020) The decreased mean platelet volume is associated with poor prognosis in patients with oropharyngeal cancer treated with radiotherapy. Radiat Oncol. https://doi.org/10.1186/s13014-020-01702-4
Kemal Y et al (2014) Mean platelet volume could be a useful biomarker for monitoring epithelial ovarian cancer. J Obstet Gynaecol 34(6):515–518
Yilmaz E et al (2017) MPV, NLR, and platelet count: new hematologic markers in diagnosis of malignant ovarian tumor. Eur J Gynaecol Oncol 38(3):346–349
Zhu C et al (2021) Clinical characteristics and prognosis of ovarian clear cell carcinoma: a 10-year retrospective study. BMC Cancer 21(1):322
Kimura N et al (2020) Optimal preoperative multidisciplinary treatment in borderline resectable pancreatic cancer. Cancers (Basel) 13(1):1–36
Schnack TH et al (2016) Demographic clinical and prognostic factors of primary ovarian adenocarcinomas of serous and clear cell histology-a comparative study. Int J Gynecol Cancer 26(1):82–90
Tang HS et al (2008) Clear cell carcinoma of the ovary: clinicopathologic features and outcomes in a Chinese cohort. Medicine 97(21):e10881
Li N et al (2017) Elevated mean platelet volume predicts poor prognosis in colorectal cancer. Sci Rep. https://doi.org/10.1038/s41598-017-11053-y
Shen XM et al (2016) Mean platelet volume provides beneficial diagnostic and prognostic information for patients with resectable gastric cancer. Oncol Lett 12(4):2501–2506
Lev EI (2016) Immature platelets: clinical relevance and research perspectives. Circulation 134(14):987–988
Couldwell G, Machlus KR (2019) Modulation of megakaryopoiesis and platelet production during inflammation. Thromb Res 179:114–120
Korniluk A et al (2019) Mean platelet volume (MPV): new perspectives for an old marker in the course and prognosis of inflammatory conditions. Mediat Inflamm 2019:9213074
Yin M et al (2022) Impact of adjuvant chemotherapy on FIGO stage I ovarian clear cell carcinoma: a systematic review and meta-analysis. Front Oncol 12:811638
Iida Y et al (2021) Clear cell carcinoma of the ovary: a clinical and molecular perspective. Int J Gynecol Cancer 31(4):605–616
Acknowledgements
This research was supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (JSPS), grant number 22K16876. We express our sincere gratitude to JSPS for their generous financial support which made this research possible.
Funding
This study was funded by Japan Society for the Promotion of Science (JSPS), 22K16876, Nobuhisa Yoshikawa.
Author information
Authors and Affiliations
Contributions
NY: data analysis, conceptualization, interpretation, and drafting of manuscript. TM, HS, SI, KY, MY, ST, AY, YI, YS, KN, KM: data collection. HK: supervision, revising the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Institutional Review Board statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Nagoya University Hospital (2006–0357). Patient consent was waived because data collection was retrospective.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10147_2023_2417_MOESM1_ESM.pdf
Supplementary file1 Supplemental Fig. 1: Comparison of mean MPV values: healthy individuals, patients with endometriosis, and patients with OCCC. Patients with endometriosis had a significantly higher mean MPV than patients with OCCC (p < 0.05). (PDF 59 KB)
10147_2023_2417_MOESM2_ESM.pdf
Supplementary file2 Supplemental Fig. 2: Comparison of MPV values across FIGO stages I, II, III, and IV. No statistically significant difference was detected between the MPV values of stages I–II and III–IV. (PDF 59 KB)
10147_2023_2417_MOESM3_ESM.pdf
Supplementary file3 Supplemental Fig. 3: Kaplan–-Meier survival curves of OCCC patients with ovarian clear cell carcinoma (OCCC) stratified by postoperative day 7 MPV. The prognosis significantly varied based on the 8.8 fL cutoff (p = 0.0291). (PDF 26 KB)
About this article
Cite this article
Yoshikawa, N., Matsukawa, T., Hattori, S. et al. Mean platelet volume as a potential biomarker for survival outcomes in ovarian clear cell carcinoma. Int J Clin Oncol 28, 1680–1689 (2023). https://doi.org/10.1007/s10147-023-02417-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-023-02417-8