Abstract
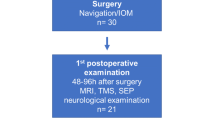
Navigated transcranial magnetic stimulation (nTMS) is a novel tool for preoperative functional mapping. It detects eloquent cortical areas directly, comparable to intraoperative direct cortical stimulation (DCS). The aim of this study was to evaluate the advantage of nTMS in comparison with functional magnetic resonance imaging (fMRI) in the clinical setting. Special focus was placed on accuracy of motor cortex localization in patients with rolandic lesions. Thirty consecutive patients were enrolled in the study. All patients received an fMRI and nTMS examination preoperatively. Feasibility of the technique and spatial resolution of upper and lower extremity cortical mapping were compared with fMRI. Consistency of preoperative mapping with intraoperative DCS was assessed via the neuronavigation system. nTMS was feasible in all 30 patients. fMRI was impossible in 7 out of 30 patients with special clinical conditions, pediatric patients, central vascular lesions, or compliance issues. The mean accuracy to localize motor cortex of nTMS was higher than in fMRI. In the subgroup of intrinsic tumors, nTMS produced statistically significant higher accuracy scores of the lower extremity localization than fMRI. fMRI failed to localize hand or leg areas in 6 out of 23 cases. Using nTMS, a preoperative localization of the central sulcus was possible in all patients. Verification of nTMS motor cortex localization with DCS was achieved in all cases. The fMRI localization of the hand area proved to be postcentral in one case. nTMS has fewer restrictions for preoperative functional mapping than fMRI and requires only a limited level of compliance. nTMS scores higher on the accuracy scale than fMRI. nTMS represents a highly valuable supplement for the preoperative functional planning in the clinical routine.







Similar content being viewed by others
References
Bittar RG, Olivier A, Sadikot AF, Andermann F, Reutens DC (2000) Cortical motor and somatosensory representation: effect of cerebral lesions. J Neurosurg 92(2):242–248. doi:10.3171/jns.2000.92.2.0242
Boroojerdi B, Foltys H, Krings T, Spetzger U, Thron A, Topper R (1999) Localization of the motor hand area using transcranial magnetic stimulation and functional magnetic resonance imaging. Clin Neurophysiol 110(4):699–704
Campero A, Ajler P, Martins C, Emmerich J, de Alencastro LF, Rhoton A Jr (2011) Usefulness of the contralateral omega sign for the topographic location of lesions in and around the central sulcus. Surg Neurol Int 2:164
Coburger J, Musahl C, Weissbach C, Bittl M (2011) Navigated transcranial magnetic stimulation-guided resection of a left parietal tumor: case report. Minim Invasive Neurosurg 54(1):38–40. doi:10.1055/s-0031-1273732
Eyre JA, Miller S, Ramesh V (1991) Constancy of central conduction delays during development in man: investigation of motor and somatosensory pathways. J Physiol 434:441–452
Fietzek UM, Heinen F, Berweck S, Maute S, Hufschmidt A, Schulte-Monting J, Lucking CH, Korinthenberg R (2000) Development of the corticospinal system and hand motor function: central conduction times and motor performance tests. Dev Med Child Neurol 42(4):220–227
Forster MT, Hattingen E, Senft C, Gasser T, Seifert V, Szelenyi A (2011) Navigated transcranial magnetic stimulation and functional magnetic resonance imaging—advanced adjuncts in preoperative planning for central region tumors. Neurosurgery 68:1317–1324. doi:10.1227/NEU.0b013e31820b528c
Giussani C, Roux FE, Ojemann J, Sganzerla EP, Pirillo D, Papagno C (2010) Is preoperative functional magnetic resonance imaging reliable for language areas mapping in brain tumor surgery? Review of language functional magnetic resonance imaging and direct cortical stimulation correlation studies. Neurosurgery 66(1):113–120. doi:10.1227/01.neu.0000360392.15450.c9
Juenger H, Ressel V, Braun C, Ernemann U, Schuhmann M, Krageloh-Mann I, Staudt M (2009) Misleading functional magnetic resonance imaging mapping of the cortical hand representation in a 4-year-old boy with an arteriovenous malformation of the central region. J Neurosurg Pediatr 4(4):333–338. doi:10.3171/2009.5.peds08466
Kantelhardt SR, Fadini T, Finke M, Kallenberg K, Siemerkus J, Bockermann V, Matthaeus L, Paulus W, Schweikard A, Rohde V, Giese A (2010) Robot-assisted image-guided transcranial magnetic stimulation for somatotopic mapping of the motor cortex: a clinical pilot study. Acta Neurochir (Wien) 152(2):333–343. doi:10.1007/s00701-009-0565-1
Korvenoja A, Kirveskari E, Aronen HJ, Avikainen S, Brander A, Huttunen J, Ilmoniemi RJ, Jaaskelainen JE, Kovala T, Makela JP, Salli E, Seppa M (2006) Sensorimotor cortex localization: comparison of magnetoencephalography, functional MR imaging, and intraoperative cortical mapping. Radiology 241(1):213–222. doi:10.1148/radiol.2411050796
Krieg SM, Shiban E, Buchmann N, Gempt J, Foerschler A, Meyer B, Ringel F (2012) Utility of presurgical navigated transcranial magnetic brain stimulation for the resection of tumors in eloquent motor areas. J Neurosurg 116(5):994–1001. doi:10.3171/2011.12.JNS111524
Lee CC, Ward HA, Sharbrough FW, Meyer FB, Marsh WR, Raffel C, So EL, Cascino GD, Shin C, Xu Y, Riederer SJ, Jack CR Jr (1999) Assessment of functional MR imaging in neurosurgical planning. AJNR Am J Neuroradiol 20(8):1511–1519
Lehericy S, Duffau H, Cornu P, Capelle L, Pidoux B, Carpentier A, Auliac S, Clemenceau S, Sichez JP, Bitar A, Valery CA, Van Effenterre R, Faillot T, Srour A, Fohanno D, Philippon J, Le Bihan D, Marsault C (2000) Correspondence between functional magnetic resonance imaging somatotopy and individual brain anatomy of the central region: comparison with intraoperative stimulation in patients with brain tumors. J Neurosurg 92(4):589–598. doi:10.3171/jns.2000.92.4.0589
Lioumis P, Zhdanov A, Makela N, Lehtinen H, Wilenius J, Neuvonen T, Hannula H, Deletis V, Picht T, Makela JP (2012) A novel approach for documenting naming errors induced by navigated transcranial magnetic stimulation. J Neurosci Methods 204(2):349–354
Ogg RJ, Laningham FH, Clarke D, Einhaus S, Zou P, Tobias ME, Boop FA (2009) Passive range of motion functional magnetic resonance imaging localizing sensorimotor cortex in sedated children. J Neurosurg Pediatr 4(4):317–322. doi:10.3171/2009.4.peds08402
Penfield W, Jasper H (1954) Epilepsy and the functional anatomy of the human brain. Little, Brown & Co, Boston
Petrella JR, Shah LM, Harris KM, Friedman AH, George TM, Sampson JH, Pekala JS, Voyvodic JT (2006) Preoperative functional mr imaging localization of language and motor areas: effect on therapeutic decision making in patients with potentially resectable brain tumors1. Radiology 240(3):793–802
Picht T, Mularski S, Kuehn B, Vajkoczy P, Kombos T, Suess O (2009) Navigated transcranial magnetic stimulation for preoperative functional diagnostics in brain tumor surgery. Neurosurgery 65(6 Suppl):93–98. doi:10.1227/01.NEU.0000348009.22750.59, discussion 98–99
Picht T, Schmidt S, Brandt S, Frey D, Hannula H, Neuvonen T, Karhu J, Vajkoczy P, Suess O (2011) Preoperative functional mapping for rolandic brain tumor surgery: comparison of navigated transcranial magnetic stimulation to direct cortical stimulation. Neurosurgery 69(3):581–588. doi:10.1227/NEU.0b013e3182181b89
Picht T, Schmidt S, Woitzik J, Suess O (2011) Navigated brain stimulation for preoperative cortical mapping in paretic patients: case report of a hemiplegic patient. Neurosurgery 68(5):E1475–E1480. doi:10.1227/NEU.0b013e318210c7df
Pirotte B, Neugroschl C, Metens T, Wikler D, Denolin V, Voordecker P, Joffroy A, Massager N, Brotchi J, Levivier M, Baleriaux D (2005) Comparison of functional MR imaging guidance to electrical cortical mapping for targeting selective motor cortex areas in neuropathic pain: a study based on intraoperative stereotactic navigation. AJNR Am J Neuroradiol 26(9):2256–2266
Quintana H (2005) Transcranial magnetic stimulation in persons younger than the age of 18. J ECT 21(2):88–95
Roux FE, Ranjeva JP, Boulanouar K, Manelfe C, Sabatier J, Tremoulet M, Berry I (1997) Motor functional MRI for presurgical evaluation of cerebral tumors. Stereotact Funct Neurosurg 68(1–4 Pt 1):106–111
Ruohonen J, Karhu J (2010) Navigated transcranial magnetic stimulation. Neurophysiol Clin 40(1):7–17. doi:10.1016/j.neucli.2010.01.006
Saisanen L, Julkunen P, Niskanen E, Danner N, Hukkanen T, Lohioja T, Nurkkala J, Mervaala E, Karhu J, Kononen M (2008) Motor potentials evoked by navigated transcranial magnetic stimulation in healthy subjects. J Clin Neurophysiol 25(6):367–372. doi:10.1097/WNP.0b013e31818e7944
Schiffbauer H, Berger MS, Ferrari P, Freudenstein D, Rowley HA, Roberts TP (2002) Preoperative magnetic source imaging for brain tumor surgery: a quantitative comparison with intraoperative sensory and motor mapping. J Neurosurg 97(6):1333–1342. doi:10.3171/jns.2002.97.6.1333
Schulder M, Maldjian JA, Liu WC, Holodny AI, Kalnin AT, Mun IK, Carmel PW (1998) Functional image-guided surgery of intracranial tumors located in or near the sensorimotor cortex. J Neurosurg 89(3):412–418. doi:10.3171/jns.1998.89.3.0412
Shurtleff H, Warner M, Poliakov A, Bournival B, Shaw DW, Ishak G, Yang T, Karandikar M, Saneto RP, Browd SR, Ojemann JG (2010) Functional magnetic resonance imaging for presurgical evaluation of very young pediatric patients with epilepsy. J Neurosurg Pediatr 5(5):500–506. doi:10.3171/2009.11.peds09248
Stippich C, Kress B, Ochmann H, Tronnier V, Sartor K (2003) Preoperative functional magnetic resonance tomography (FMRI) in patients with rolandic brain tumors: indication, investigation strategy, possibilities and limitations of clinical application. Rofo 175(8):1042–1050. doi:10.1055/s-2003-40920
Ulmer JL, Hacein-Bey L, Mathews VP, Mueller WM, DeYoe EA, Prost RW, Meyer GA, Krouwer HG, Schmainda KM (2004) Lesion-induced pseudo-dominance at functional magnetic resonance imaging: implications for preoperative assessments. Neurosurgery 55(3):569–579, discussion 580–561
Zhang D, Johnston JM, Fox MD, Leuthardt EC, Grubb RL, Chicoine MR, Smyth MD, Snyder AZ, Raichle ME, Shimony JS (2009) Preoperative sensorimotor mapping in brain tumor patients using spontaneous fluctuations in neuronal activity imaged with functional magnetic resonance imaging: initial experience. Neurosurgery 65(6 Suppl):226–236. doi:10.1227/01.neu.0000350868.95634.ca
Acknowledgments
We thank Claudia Weissbach and Klarissa Belicke for performing neurophysiological recordings with outstanding motivation and enthusiasm.
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Hugues Duffau, Montpellier, France
The authors compared navigated transcranial magnetic stimulation (nTMS) with preoperative functional magnetic resonance imaging (fMRI) and intraoperative direct cortical stimulation (DCS) to identify the primary motor cortex in a consecutive series of patients who underwent surgery for a lesion near or within the central region. They found that the cortical spatial resolution of nTMS was higher than of fMRI. Moreover, verification of nTMS motor cortex localization with DCS was achieved in all cases.
A very important message in this article is that nTMS was feasible in all cases, contrary to fMRI which was impossible in seven patients. Thus, preoperative nTMS may represent an interesting alternative to fMRI in pediatric, demented, or hemiplegic patients.
However, it is worth noting that, in this series, there were no significant differences between fMRI and nTMS. Therefore, the authors have to be cautious before to claim that the cortical spatial resolution of nTMS is higher than of fMRI, because this conclusion is not yet validated by their data. In addition, when Coburger et al. compared nTMS with DCS, they wrote that DCS had a cortical resolution of 10 mm within the gyrus, and that nTMS most likely had a very similar distribution. It is not totally true. Indeed, in glioma surgery, it was demonstrated that the combination of direct subcortical stimulation of the white matter pathways with DCS increased the spatial resolution, allowing an optimization of the resection until functional tracts have been encountered, with no margin [1, 2]. As a consequence, one should be aware about the impossibility for nTMS to perform subcortical mapping—which represents a main limitation in surgery for intra-axial brain tumor. This is the reason why it is dangerous to claim that “technically language mapping (using nTMS) similar to awake craniotomy is possible”, due to the fact that neural foundations of language are constituted by a subcortical connectivity which should absolutely be mapped and preserved intraoperatively because not able to be compensated when damaged [3, 4]. For all these reasons, intrasurgical direct electrical mapping remains the gold standard in glioma surgery, as recently demonstrated in a meta-analysis with more than 8,000 tumors [5].
References
1. Duffau H, Gatignol P, Mandonnet E, Capelle L, Taillandier L (2008) Intraoperative subcortical stimulation mapping of language pathways in a consecutive series of 115 patients with grade II glioma in the left dominant hemisphere. J Neurosurg 109:461–471
2. Gil Robles S, Duffau H (2010) Surgical management of World Health Organization Grade II gliomas in eloquent areas: the necessity of preserving a margin around functional structures? Neurosurg Focus 28(2):E8
3. Duffau H (2009) Does post-lesional subcortical plasticity exist in the human brain? Neurosci Res 65:131–135
4. Ius T, Angelini E, Thiebaut de Schotten M, Mandonnet E, Duffau H (2011) Evidence for potentials and limitations of brain plasticity using an atlas of functional resectability of WHO grade II gliomas: towards a “minimal common brain”. Neuroimage 56:992–1000
5. De Witt Hamer PC, Gil Robles S, Zwinderman AH, Duffau H, Berger MS (2012) Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol (in press)
Matthias Krammer, Christianto B. Lumenta, Munich, Germany
This article is a good amendment to the existing literature dealing with the new method of navigated transcranial magnetic stimulation (nTMS) in comparison to functional MRI in patients with tumors in the rolandic area.
There are only few articles that describe the method of nTMS itself already.
The authors compare the two methods in 30 patients with very different benign and malignant tumors and vascular lesions. We think this is tolerable in such a paper that introduce a new method and is even necessary for further investigations. There exists up to date no articles with a bigger patient group. One problem is that it was not possible to perform fMRI in seven patients (23 %) due to compliance or other problems. This is a well-known problem of this method but makes statistical statements comparing the two methods in a patient group with 30 cases questionable.
The authors report about a patient where the fMRI showed the motor hand area postcentral and concluded that this is an error. According to the intraoperative control performed in this study with negative direct cortical stimulation this is really a false-positive localization. Kombos et al. (Acta Neurochir 799 (Wien) (1999) 141: 1295–1301) identified true functional motor areas 800 in the postcentral parietal location using direct monopolar and bipolar 801 stimulation results in 7.85 % few cases.
The authors report further about identification of the motor cortex even in hemiplegic patients. Do we look forward to get an improvement after tumor resection? This could be possible in our opinion in a hemiparetic patient and in hemiplegic patients with motor function improvement after antiedematous therapy, but in really hemiplegic patients? Is the surgical procedure in this case the same for infiltrating tumors in comparison to, e.g., meningioma? Do the authors stop tumor resection in a true hemiplegic patient with a glioblastoma when they reach the identified motor cortex and there is still vital and visible tumor?
Although it is not part of this study, we think that the most important tools for surgery in the rolandic area are the neurophysiological methods looking for the central sulcus with the phase reversal, direct cortical, and subcortical stimulation. Independent from the cortical localization of a tumor, it is also important during the resection to save the subcortical pathways. In opposite to nTMS, subcortical pathways could be identified by fMRI and MRI-DTI. A good new method is the combination of nTMS and DTI using the nTMS motor cortex region as starting point for the DTI generation.
Christopher Nimsky, Marburg, Germany
Preoperative functional mapping is an important part of preoperative planning and decision making in lesions close to eloquent brain areas. Magnetoencephalography (MEG) and functional magnetic resonance imaging (fMRI) were among the first techniques to identify these eloquent brain areas. Despite having different physical principles being the bases of these methods, a quite reliable identification of the motor cortex or language-related areas is possible. fMRI has the advantage to be widely available; however, the method is not able to identify the proper structures in all cases, so some groups prefer to combine the results of fMRI and MEG. The authors demonstrate the application of navigated transcranial magnetic stimulation (nTMS) and could show that it had fewer restrictions than fMRI in their series to identify the motor cortex. So potentially nTMS might also be an alternative for MEG, which is measuring the electrical activity directly, in contrast to fMRI measuring oxygen consumption. It will be interesting to see, whether nTMS will also be able to localize speech relevant areas, which might be even more interesting in a clinical setting.
Rights and permissions
About this article
Cite this article
Coburger, J., Musahl, C., Henkes, H. et al. Comparison of navigated transcranial magnetic stimulation and functional magnetic resonance imaging for preoperative mapping in rolandic tumor surgery. Neurosurg Rev 36, 65–76 (2013). https://doi.org/10.1007/s10143-012-0413-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-012-0413-2