Abstract
Purpose
Spinal MRI is the exam of choice for the workup of patients with suspected spinal infection. In this retrospective study, we assess the value of obtaining contrast-enhanced spinal MRI for patients presenting to the emergency department (ED) with acute back pain and a history of intravenous drug use (IVDU).
Methods
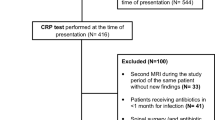
A retrospective IRB-approved, HIPAA compliant review of the imaging findings, reports and electronic charts of 167 consecutive IV drug-using patients (M/F = 96:71, mean age = 40 years) that presented to the ED with acute back pain over a 55-month period and underwent contrast-enhanced spinal MRI within 24 h. Fisher’s exact test was used to identify statistically significant (p < 0.05) associations with MRI findings.
Results
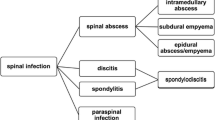
Evidence of infectious spondylitis was demonstrated on the spinal MRIs of 39.5% (n = 66) of 167 patients, all of whom were admitted, and nearly half (48.5%; 32/66) underwent surgical or percutaneous intervention. Statistically significant differences in the decision to admit, blood cultures, and the type of treatment was demonstrated in patients with findings of spinal infection on MRI (p < 0.05).
Conclusion
Use of emergent spinal MRI in the workup of IVDU patients with acute back pain is justified despite the resultant pressure on MRI scanner, technologist, and interpretation time.



Similar content being viewed by others
References
Sapico FL, Montgomerie JZ (1990) Vertebral osteomyelitis. Infect Dis Clin N Am 4(3):539–550
Ziu M, Dengler B, Cordell D, Bartanusz V (2014) Diagnosis and management of primary pyogenic spinal infections in intravenous recreational drug users. Neurosurg Focus 37(2):E3. https://doi.org/10.3171/2014.6.FOCUS14148
Soehle M, Wallenfang T (2002) Spinal epidural abscesses: clinical manifestations, prognostic factors, and outcomes. Neurosurgery 51(1):79–85; discussion 86-7. https://doi.org/10.1097/00006123-200207000-00013
Dziurzynska-Bialek E et al (2012) Diagnostic difficulties resulting from morphological image variation in spondylodiscitis MR imaging. Pol J Radiol 77(3):25–34
Chuo CY, Fu YC, Lu YM, Chen JC, Shen WJ, Yang CH, Chen CY (2007) Spinal infection in intravenous drug abusers. J Spinal Disord Tech 20(4):324–328. https://doi.org/10.1097/BSD.0b013e31802c144a
Duarte RM, Vaccaro AR (2013) Spinal infection: state of the art and management algorithm. Eur Spine J 22(12):2787–2799. https://doi.org/10.1007/s00586-013-2850-1
Schoener EP, Hopper JA, Pierre JD (2002) Injection drug use in North America. Infect Dis Clin N Am 16(3):535–551 vii
Rigamonti D, Liem L, Sampath P, Knoller N, Numaguchi Y, Schreibman DL, Sloan MA, Wolf A, Zeidman S (1999) Spinal epidural abscess: contemporary trends in etiology, evaluation, and management. Surg Neurol 52(2):189–196; discussion 197. https://doi.org/10.1016/S0090-3019(99)00055-5
Kayani I, Syed I, Saifuddin A, Green R, MacSweeney F (2004) Vertebral osteomyelitis without disc involvement. Clin Radiol 59(10):881–891. https://doi.org/10.1016/j.crad.2004.03.023
Kapeller P, Fazekas F, Krametter D, Koch M, Roob G, Schmidt R, Offenbacher H (1997) Pyogenic infectious spondylitis: clinical, laboratory and MRI features. Eur Neurol 38(2):94–98
Gouliouris T, Aliyu SH, Brown NM (2010) Spondylodiscitis: update on diagnosis and management. J Antimicrob Chemother 65(Suppl 3):iii11–iii24
James SL, Davies AM (2006) Imaging of infectious spinal disorders in children and adults. Eur J Radiol 58(1):27–40. https://doi.org/10.1016/j.ejrad.2005.12.002
Tyrrell PN, Cassar-Pullicino VN, McCall IW (1999) Spinal infection. Eur Radiol 9(6):1066–1077. https://doi.org/10.1007/s003300050793
Arko LT et al (2014) Medical and surgical management of spinal epidural abscess: a systematic review. Neurosurg Focus 37(2):E4. https://doi.org/10.3171/2014.6.FOCUS14127
Baleriaux DL, Neugroschl C (2004) Spinal and spinal cord infection. Eur Radiol 14(Suppl 3):E72–E83
Li T, Liu T, Jiang Z, Cui X, Sun J (2016) Diagnosing pyogenic, brucella and tuberculous spondylitis using histopathology and MRI: a retrospective study. Exp Ther Med 12(4):2069–2077. https://doi.org/10.3892/etm.2016.3602
Sharif HS (1992) Role of MR imaging in the management of spinal infections. AJR Am J Roentgenol 158(6):1333–1345. https://doi.org/10.2214/ajr.158.6.1590137
Stabler A, Reiser MF (2001) Imaging of spinal infection. Radiol Clin N Am 39(1):115–135. https://doi.org/10.1016/S0033-8389(05)70266-9
Tali ET (2004) Spinal infections. Eur J Radiol 50(2):120–133. https://doi.org/10.1016/j.ejrad.2003.10.022
Reihsaus E, Waldbaur H, Seeling W (2000) Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev 23(4):175–204; discussion 205. https://doi.org/10.1007/PL00011954
Sapico FL, Montgomerie JZ (1980) Vertebral osteomyelitis in intravenous drug abusers: report of three cases and review of the literature. Rev Infect Dis 2(2):196–206. https://doi.org/10.1093/clinids/2.2.196
Guerado E, Cervan AM (2012) Surgical treatment of spondylodiscitis. An update. Int Orthop 36(2):413–420. https://doi.org/10.1007/s00264-011-1441-1
Hickey NA, White PG (2000) Septic arthritis of a lumbar facet joint causing multiple abscesses. Clin Radiol 55(6):481–483. https://doi.org/10.1053/crad.2000.0091
Darouiche RO, Hamill RJ, Greenberg SB, Weathers SW, Musher DM (1992) Bacterial spinal epidural abscess. Review of 43 cases and literature survey. Medicine (Baltimore) 71(6):369–385. https://doi.org/10.1097/00005792-199211000-00004
Sawada M et al (1996) Cervical discitis associated with spinal epidural abscess caused by methicillin-resistant staphylococcus aureus. Neurol Med Chir (Tokyo) 36(1):40–44. https://doi.org/10.2176/nmc.36.40
Kumar K, Hunter G (2005) Spinal epidural abscess. Neurocrit Care 2(3):245–251. https://doi.org/10.1385/NCC:2:3:245
Wang Z, Lenehan B, Itshayek E, Boyd M, Dvorak M, Fisher C, Kwon B, Paquette S, Street J (2012) Primary pyogenic infection of the spine in intravenous drug users: a prospective observational study. Spine (Phila Pa 1976) 37(8):685–692. https://doi.org/10.1097/BRS.0b013e31823b01b8
Mackenzie AR, Laing RBS, Smith CC, Kaar GF, Smith FW (1998) Spinal epidural abscess: the importance of early diagnosis and treatment. J Neurol Neurosurg Psychiatry 65(2):209–212. https://doi.org/10.1136/jnnp.65.2.209
Davis DP, Wold RM, Patel RJ, Tran AJ, Tokhi RN, Chan TC, Vilke GM (2004) The clinical presentation and impact of diagnostic delays on emergency department patients with spinal epidural abscess. J Emerg Med 26(3):285–291. https://doi.org/10.1016/j.jemermed.2003.11.013
Pradilla G, Nagahama Y, Spivak AM, Bydon A, Rigamonti D (2010) Spinal epidural abscess: current diagnosis and management. Curr Infect Dis Rep 12(6):484–491. https://doi.org/10.1007/s11908-010-0140-1
Nussbaum ES, Rigamonti D, Standiford H, Numaguchi Y, Wolf AL, Robinson WL (1992) Spinal epidural abscess: a report of 40 cases and review. Surg Neurol 38(3):225–231. https://doi.org/10.1016/0090-3019(92)90173-K
Modic MT, Feiglin DH, Piraino DW, Boumphrey F, Weinstein MA, Duchesneau PM, Rehm S (1985) Vertebral osteomyelitis: assessment using MR. Radiology 157(1):157–166. https://doi.org/10.1148/radiology.157.1.3875878
Carragee EJ (1997) The clinical use of magnetic resonance imaging in pyogenic vertebral osteomyelitis. Spine (Phila Pa 1976) 22(7):780–785. https://doi.org/10.1097/00007632-199704010-00015
Bremer AA, Darouiche RO (2004) Spinal epidural abscess presenting as intra-abdominal pathology: a case report and literature review. J Emerg Med 26(1):51–56. https://doi.org/10.1016/j.jemermed.2003.04.005
Stratton A, Faris P, Thomas K (2017) The prognostic accuracy of suggested predictors of failure of medical management in patients with nontuberculous spinal epidural abscess. Glob Spine J p. 2192568217719437
Kumar Y, Gupta N, Chhabra A, Fukuda T, Soni N, Hayashi D (2017) Magnetic resonance imaging of bacterial and tuberculous spondylodiscitis with associated complications and non-infectious spinal pathology mimicking infections: a pictorial review. BMC Musculoskelet Disord 18(1):244. https://doi.org/10.1186/s12891-017-1608-z
Hong SH, Choi JY, Lee JW, Kim NR, Choi JA, Kang HS (2009) MR imaging assessment of the spine: infection or an imitation? Radiographics 29(2):599–612. https://doi.org/10.1148/rg.292085137
Arora S, Sabat D, Maini L, Sural S, Kumar V, Gautam VK, Gupta A, Dhal A (2012) Isolated involvement of the posterior elements in spinal tuberculosis: a review of twenty-four cases. J Bone Joint Surg Am 94(20):e151. https://doi.org/10.2106/JBJS.K.01464
Maiuri F, laconetta G, Gallicchio B, Manto A, Briganti F (1997) Spondylodiscitis. Clinical and magnetic resonance diagnosis. Spine (Phila Pa 1976) 22(15):1741–1746. https://doi.org/10.1097/00007632-199708010-00012
Bond A, Manian FA (2016) Spinal epidural abscess: a review with special emphasis on earlier diagnosis. Biomed Res Int 2016:1614328
Galhotra RD, Jain T, Sandhu P, Galhotra V (2015) Utility of magnetic resonance imaging in the differential diagnosis of tubercular and pyogenic spondylodiscitis. J Nat Sci Biol Med 6(2):388–393. https://doi.org/10.4103/0976-9668.160016
Berbari EF, Kanj SS, Kowalski TJ, Darouiche RO, Widmer AF, Schmitt SK, Hendershot EF, Holtom PD, Huddleston PM 3rd, Petermann GW, Osmon DR, Infectious Diseases Society of America (2015) 2015 Infectious Diseases Society of America (IDSA) clinical practice guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults. Clin Infect Dis 61(6):e26–e46. https://doi.org/10.1093/cid/civ482
Hadland SE, DeBeck K, Kerr T, Feng C, Montaner JS, Wood E (2014) Prescription opioid injection and risk of hepatitis C in relation to traditional drugs of misuse in a prospective cohort of street youth. BMJ Open 4(7):e005419. https://doi.org/10.1136/bmjopen-2014-005419
Ebright JR, Pieper B (2002) Skin and soft tissue infections in injection drug users. Infect Dis Clin N Am 16(3):697–712. https://doi.org/10.1016/S0891-5520(02)00017-X
Crum-Cianflone NF (2008) Bacterial, fungal, parasitic, and viral myositis. Clin Microbiol Rev 21(3):473–494. https://doi.org/10.1128/CMR.00001-08
Dunbar JA et al (2010) The MRI appearances of early vertebral osteomyelitis and discitis. Clin Radiol 65(12):974–981. https://doi.org/10.1016/j.crad.2010.03.015
Okada F, Takayama H, Doita M, Harada T, Yoshiya S, Kurosaka M (2005) Lumbar facet joint infection associated with epidural and paraspinal abscess: a case report with review of the literature. J Spinal Disord Tech 18(5):458–461. https://doi.org/10.1097/01.bsd.0000159036.42989.93
Thrush A, Enzmann D (1990) MR imaging of infectious spondylitis. AJNR Am J Neuroradiol 11(6):1171–1180
Dagirmanjian A, Schils J, McHenry M, Modic MT (1996) MR imaging of vertebral osteomyelitis revisited. AJR Am J Roentgenol 167(6):1539–1543. https://doi.org/10.2214/ajr.167.6.8956593
Tung GA, Yim JWK, Mermel LA, Philip L, Rogg JM (1999) Spinal epidural abscess: correlation between MRI findings and outcome. Neuroradiology 41(12):904–909. https://doi.org/10.1007/s002340050865
Ledermann HP, Schweitzer ME, Morrison WB, Carrino JA (2003) MR imaging findings in spinal infections: rules or myths? Radiology 228(2):506–514. https://doi.org/10.1148/radiol.2282020752
DeSanto J, Ross JS (2011) Spine infection/inflammation. Radiol Clin N Am 49(1):105–127. https://doi.org/10.1016/j.rcl.2010.07.018
Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ (2000) Hematogenous pyogenic spinal infections and their surgical management. Spine (Phila Pa 1976) 25(13):1668–1679. https://doi.org/10.1097/00007632-200007010-00010
Gillams AR, Chaddha B, Carter AP (1996) MR appearances of the temporal evolution and resolution of infectious spondylitis. AJR Am J Roentgenol 166(4):903–907. https://doi.org/10.2214/ajr.166.4.8610571
Cheung WY, Luk KD (2012) Pyogenic spondylitis. Int Orthop 36(2):397–404. https://doi.org/10.1007/s00264-011-1384-6
Crum NF (2004) Bacterial pyomyositis in the United States. Am J Med 117(6):420–428. https://doi.org/10.1016/j.amjmed.2004.03.031
Yu CW, Hsiao JK, Hsu CY, Shih TTF (2004) Bacterial pyomyositis: MRI and clinical correlation. Magn Reson Imaging 22(9):1233–1241. https://doi.org/10.1016/j.mri.2004.08.005
Numaguchi Y, Rigamonti D, Rothman MI, Sato S, Mihara F, Sadato N (1993) Spinal epidural abscess: evaluation with gadolinium-enhanced MR imaging. Radiographics 13(3):545–559; discussion 559-60. https://doi.org/10.1148/radiographics.13.3.8316663
Lu CH, Chang WN, Lui CC, Lee PY, Chang HW (2002) Adult spinal epidural abscess: clinical features and prognostic factors. Clin Neurol Neurosurg 104(4):306–310. https://doi.org/10.1016/S0303-8467(02)00020-3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript declare no conflicts of interest, and no relationships with any companies whose products or services may be related to the subject matter of the article.
Disclosure
-
1.
The scientific guarantor of this publication is Charles Colip MD.
-
2.
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
-
3.
The authors state that this work has not received any funding.
-
4.
No complex statistical methods were necessary for this paper. One of the authors has significant statistical experience.
-
5.
Institutional review board approval was obtained.
-
6.
Written informed consent was waived by the institutional review board.
-
7.
Human subjects.
-
8.
No study subjects or cohorts have been previously reported.
-
9.
Methodology:
-
Retrospective
-
Observational
-
Performed at one institution
Rights and permissions
About this article
Cite this article
Colip, C.G., Lotfi, M., Buch, K. et al. Emergent spinal MRI in IVDU patients presenting with back pain: do we need an MRI in every case?. Emerg Radiol 25, 247–256 (2018). https://doi.org/10.1007/s10140-017-1572-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-017-1572-9