Abstract
Introduction
Gastric cancer with fusion genes involving the Rho GTPase-activating protein domain (RhoGAP-GC) is mainly included in the genomically stable type of The Cancer Genome Atlas classification. Clinical implications and histological characteristics of RhoGAP-GC in the early phase remain unclear.
Methods
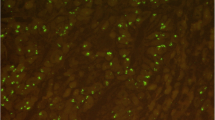
We analyzed 878 consecutive pT1b GCs for RhoGAP and its partner genes using fluorescence in situ hybridization assay.
Results
RhoGAP fusion was detected in 57 (6.5%) GCs. Univariate analysis revealed that female sex, middle–lower third tumor location, advanced macroscopic type, tumor diameter > 2 cm, pT1b2, lymphatic invasion, venous invasion, negative EBER-ISH, and RhoGAP fusion were significantly associated with lymph node metastasis (LNM). Multivariate analysis presented RhoGAP fusion, lymphatic invasion, tumor diameter > 2 cm, advanced macroscopic type, venous invasion, and middle–lower third tumor location as independent risk factors for LNM. Notably, RhoGAP fusion had the highest odds ratio (3.92) for LNM among analyzed parameters (95% CI 2.12–7.27; p < 0.001). Compared to non-RhoGAP-GCs, RhoGAP-GCs were significantly frequent in younger females and showed the highest incidence of lymphatic invasion (56.2%) and LNM (49.1%) (p < 0.001). Histologically, microtubular architecture with pseudo-trabecular interconnection and small aggregations of tumor cells with a varied amount of cytoplasmic mucin, named “microtubular–mucocellular (MTMC) histology,” was found in 93.0% (53 of 57) of RhoGAP-GCs in the intramucosal area. MTMC histology showed high sensitivity and negative predictive value (93.0% and 99.4%, respectively) for RhoGAP fusion, albeit positive predictive value is low (34.9%).
Conclusion
RhoGAP-GC is linked to a characteristic MTMC histology and a high incidence of LNM.



Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the present study are not publicly available in accordance with the policy of JFCR but may be available from the corresponding author by submitting a research proposal, which will be reviewed for scientific merit and feasibility.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Kwee RM, Kwee TC. Predicting lymph node status in early gastric cancer. Gastric Cancer. 2008;11:134–48.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2021 (ver. 6). Gastric Cancer. 2023;26:1–25.
Ono H, Yao K, Fujishiro M, Oda I, N Uedo, Nimura S, et al. Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer (second edition). Dig Endosc. 2021;33:4–20.
Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–25.
Laurén P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histoclinical classification. Acta Pathol Microbiol Scand. 1965;64:31–49.
Nakamura K, Sugano H, Takagi K. Carcinoma of the stomach in incipient phase: its histogenesis and histological appearances. Gan. 1968;59:251–8.
Carneiro F, Fukayama M, Grabsch HI, Yasui W. Gastric adenocarcinoma. In: WHO Classification of Tumours Editorial Board. Digestive System Tumours, 5th ed. Lyon: International Agency for Research on Cancer; 2019;85–97.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma. 3rd ed. Gastric Cancer 2011;101–112.
Cancer Genome Atlas Research Network. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–9.
Osumi H, Kawachi H, Yoshio T, Ida S, Yamamoto N, Horiuchi Y, et al. Epstein-Barr virus status is a promising biomarker for endoscopic resection in early gastric cancer: proposal of a novel therapeutic strategy. J Gastroenterol. 2019;54:774–83.
Yang H, Hong D, Cho SY, Park YS, Ko WR, Kim JH, et al. RhoGAP domain-containing fusions and PPAPDC1A fusions are recurrent and prognostic in diffuse gastric cancer. Nat Commun. 2018;9:4439.
Zhang WH, Zhang SY, Hou QQ, Qin Y, Chen XZ, Zhou ZG, et al. The significance of the CLDN18-ARHGAP fusion gene in gastric cancer: A systematic review and meta-analysis. Front Oncol. 2020;10:1214.
Shu Y, Zhang W, Hou Q, Zhao L, Zhang S, Zhou J, et al. Prognostic significance of frequent CLDN18-ARHGAP26/6 fusion in gastric signet-ring cell cancer. Nat Commun. 2018;9:2447.
Nakayama I, Shinozaki E, Sakata S, Yamamoto N, Fujisaki J, Muramatsu Y, et al. Enrichment of CLDN18-ARHGAP fusion gene in gastric cancers in young adults. Cancer Sci. 2019;110:1352–63.
Tanaka A, Ishikawa S, Ushiku T, Yamazawa S, Katoh H, Hayashi A, et al. Frequent CLDN18-ARHGAP fusion in highly metastatic diffuse-type gastric cancer with relatively early onset. Oncotarget. 2018;9:29336–50.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Jaiswal M, Derewenda U, Reis K, Nouri K, Koessmeier KT, Aspenström P, et al. Deciphering the molecular and functional basis of r RhoGAP family proteins: a systematic approach toward selective inactivation of Rho family proteins. J Biol Chem. 2016;291:20353–71.
Hodge RG, Ridley AJ. Regulating Rho GTPases and their regulators. Nat Rev Mol Cell Biol. 2016;17:496–510.
Komatsu M, Ichikawa H, Chiwaki F, Sakamoto H, Komatsuzaki R, Asaumi M, et al. ARHGAP-RhoA signaling provokes homotypic adhesion-triggered cell death of metastasized diffuse-type gastric cancer. Oncogene. 2022;41:4779–94.
Yao F, Kausalya JP, Sia YY, Teo AS, Lee WH, Ong AG, et al. Recurrent fusion genes in gastric cancer: CLDN18-ARHGAP26 induces loss of epithelial integrity. Cell Rep. 2015;12:272–85.
Hashimoto T, Ogawa R, Tang TY, Yoshida H, Taniguchi H, Katai H, et al. RHOA mutations and CLDN18-ARHGAP fusions in intestinal-type adenocarcinoma with anastomosing glands of the stomach. Mod Pathol. 2019;32:568–75.
Okamoto N, Kawachi H, Yoshida T, Kitagaki K, Sekine M, Kojima K, et al. “Crawling-type” adenocarcinoma of the stomach: a distinct entity preceding poorly differentiated adenocarcinoma. Gastric Cancer. 2013;16:220–32.
Ushiku T, Arnason T, Ban S, Hishima T, Shimizu M, Fukayama M, et al. Very well-differentiated gastric carcinoma of intestinal type: analysis of diagnostic criteria. Mod Pathol. 2013;26:1620–31.
Ushiku T, Ishikawa S, Kakiuchi A, Tanaka A, Katoh H, Aburatani H, et al. RHOA mutation in diffuse-type gastric cancer: a comparative clinicopathology analysis of 87 cases. Gastric Cancer. 2016;19:403–11.
Sekiguchi M, Oda I, Taniguchi H, Suzuki H, Morita S, Fukagawa T, et al. Risk stratification and predictive risk-scoring model for lymph node metastasis in early gastric cancer. J Gastroenterol. 2016;51:961–70.
Acknowledgements
We thank Ms. Miyuki Kogure, Ms. Tomoyo Kakita, Ms. Keiko Shiozawa, Ms. Mayumi Ogawa, Mr. Motoyoshi Iwakoshi, and Mr. Shuhei Ishii for their technical support.
Funding
This research was supported by the JSPS KAKENHI Grant Numbers JP16K08661 and JP21K06918.
Author information
Authors and Affiliations
Contributions
HN, SS, KT, and HK developed the study concept and design, interpretation of data, and statistical analysis and SS, SB, KT, and HK developed the methodology; HN, KN, CH, MT, ES, NY, and HK provided the histopathological diagnoses; HN, SS, KT, and HK wrote, reviewed, and revised the paper; TH, JF, and SN provided data acquisition. SB, YT, IN, and KI provided technical and material support. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest for this article.
Ethical approval
This study was approved by the institutional review board of the Japanese Foundation for Cancer Research (2022-GB-104). This study was conducted in accordance with the principles of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Noda, H., Sakata, S., Baba, S. et al. Early gastric cancer with RhoGAP fusion is linked to frequent nodal metastasis and a part of microtubular–mucocellular histology. Gastric Cancer (2024). https://doi.org/10.1007/s10120-024-01507-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10120-024-01507-4