Abstract
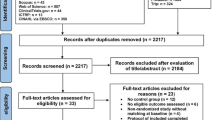
Although several studies have evaluated the effect of low-level laser therapy (LLLT) on orthodontic movement acceleration, results are still inconsistent. Such inconsistencies may be attributed to the differences in the LLLT application protocols, especially in terms of wavelength ranges. Objective: (i) to assess the clinical effects of LLLT on the acceleration of orthodontic movement and (ii) to establish the most effective LLLT wavelength to accelerate tooth movement during orthodontic treatments. MEDLINE (PubMed), Scopus, ScienceDirect, and LILACS were searched from inception to October 2022. Inclusion criteria: Split-mouth randomised clinical trials (RCTs) on systemically healthy patients reporting the effect of LLLT in accelerating orthodontic movements, specifically retraction of canines. The risk of bias was assessed using RoB-2. A random effect model was applied. Nineteen RCTs met the inclusion criteria for qualitative synthesis, and eighteen RCTs were included in the quantitative synthesis. Seventeen studies were rated as at some concerns of bias and two studies were classified as having a low risk of bias. In general terms, this systematic review and meta-analysis presents a moderate risk of bias. Findings of this systematic review and meta-analysis point to a tendency for faster orthodontic dental movement in the groups receiving LLLT treatment during the first (OR of 0.28 95% CI (0.07 to 0.48)), second (OR of 0.52 95% CI (0.31 to 0.73)), and third (OR of 0.41 95% CI (0.03 to 0.79)) month follow-up. Wavelengths ≤ 810 nm and energy density values ≤ 5.3 J/cm2 were associated with faster orthodontic tooth movement.




Similar content being viewed by others
Data availability
All data are provided within the manuscript.
References
Gkantidis N, Mistakidis I, Kouskoura T, Pandis N (2014) Effectiveness of non-conventional methods for accelerated orthodontic tooth movement: a systematic review and meta-analysis. J Dent 42(10):1300–1319. https://doi.org/10.1016/j.jdent.2014.07.013
Patil AK, Shetty AS, Setty S, Thakur S (2013) Understanding the advances in biology of orthodontic tooth movement for improved ortho-perio interdisciplinary approach. J Indian Soc Periodontol 17(3):309–318. https://doi.org/10.4103/0972-124X.115648
Hall M, Masella R, Meister M (2001) PDL neuron-associated neurotransmitters in orthodontic tooth movement: identification and proposed mechanism of action. Todays FDA 13(2):24–25
Long H, Pyakurel U, Wang Y, Liao L, Zhou Y, Lai W (2013) Interventions for accelerating orthodontic tooth movement A systematic review. Angle Orthodontist 83(1):164–171. https://doi.org/10.2319/031512-224.1
Dalaie K, Hamedi R, Kharazifard MJ, Mahdian M, Bayat M (2015) Effect of low-level laser therapy on orthodontic tooth movement: a clinical investigation. J Dent (Tehran) 12(4):249–256
Varella AM, Revankar AV, Patil AK (2018) Low-level laser therapy increases interleukin-1β in gingival crevicular fluid and enhances the rate of orthodontic tooth movement. Am J Orthod Dentofacial Orthop 154(4):535-544.e5. https://doi.org/10.1016/j.ajodo.2018.01.012
Limpanichkul W, Godfrey K, Srisuk N, Rattanayatikul C (2006) Effects of low-level laser therapy on the rate of orthodontic tooth movement. Orthod Craniofac Res 9(1):38–43. https://doi.org/10.1111/j.1601-6343.2006.00338.x
Yassaei S, Fekrazad R, Shahraki N (2013) Effect of low level laser therapy on orthodontic tooth movement: a review article. J Dent (Tehran) 10(3):264–272
Tam SY, Tam VCW, Ramkumar S, Khaw ML, Law HKW, Lee SWY (2020) Review on the cellular mechanisms of low-level laser therapy use in oncology. Front Oncol 10:1255. https://doi.org/10.3389/fonc.2020.01255
Rola P, Włodarczak S, Lesiak M, Doroszko A, Włodarczak A (2022) Changes in cell biology under the influence of low-level laser therapy. Photonics 9(7):502. https://doi.org/10.3390/photonics9070502
Yoshida T, Yamaguchi M, Utsunomiya T, Kato M, Arai Y, Kaneda T et al (2009) Low-energy laser irradiation accelerates the velocity of tooth movement via stimulation of the alveolar bone remodeling. Orthod Craniofac Res 12(4):289–298. https://doi.org/10.1111/j.1601-6343.2009.01464.x
Gama SK, Habib FA, Monteiro JS, Paraguassú GM, Araújo TM, Cangussú MC et al (2010) Tooth movement after infrared laser phototherapy: clinical study in rodents. Photomed Laser Surg 28(Suppl 2):S79-83. https://doi.org/10.1089/pho.2009.2618
Salehi P, Heidari S, Tanideh N, Torkan S (2015) Effect of low-level laser irradiation on the rate and short-term stability of rotational tooth movement in dogs. Am J Orthod Dentofacial Orthop 147(5):578–586. https://doi.org/10.1016/j.ajodo.2014.12.024
Fujita S, Yamaguchi M, Utsunomiya T, Yamamoto H, Kasai K (2008) Low-energy laser stimulates tooth movement velocity via expression of RANK and RANKL. Orthod Craniofac Res 11(3):143–155. https://doi.org/10.1111/j.1601-6343.2008.00423.x
de Almeida VL, de Andrade Gois VL, Andrade RN, Cesar CP, de Albuquerque-Junior RL, de Mello RS et al (2016) Efficiency of low-level laser therapy within induced dental movement: a systematic review and meta-analysis. J Photochem Photobiol B 158:258–266. https://doi.org/10.1016/j.jphotobiol.2016.02.037
Sonesson M, De Geer E, Subraian J, Petrén S (2016) Efficacy of low-level laser therapy in accelerating tooth movement, preventing relapse and managing acute pain during orthodontic treatment in humans: a systematic review. BMC Oral Health 17(1):11. https://doi.org/10.1186/s12903-016-0242-8
Carvalho-Lobato P, Garcia VJ, Kasem K, Ustrell-Torrent JM, Tallón-Walton V, Manzanares-Céspedes MC (2014) Tooth movement in orthodontic treatment with low-level laser therapy: a systematic review of human and animal studies. Photomed Laser Surg 32(5):302–309. https://doi.org/10.1089/pho.2012.3439
Sousa MV, Pinzan A, Consolaro A, Henriques JF, de Freitas MR (2014) Systematic literature review: influence of low-level laser on orthodontic movement and pain control in humans. Photomed Laser Surg 32(11):592–599. https://doi.org/10.1089/pho.2014.3789
Nimeri G, Kau CH, Abou-Kheir NS, Corona R (2013) Acceleration of tooth movement during orthodontic treatment—a frontier in orthodontics. Prog Orthod 14:42. https://doi.org/10.1186/2196-1042-14-42
Sandoval P, Bizcar B, Navarro P, Knösel M. (2017) Efficacy of diode laser therapy in acceleration of orthodontic space closure: a split-mouth randomized clinical trial. Int J Dent Oral Health. 3(2). https://doi.org/10.16966/2378-7090.229
Caccianiga G, Paiusco A, Perillo L, Nucera R, Pinsino A, Maddalone M et al (2017) Does low-level laser therapy enhance the efficiency of orthodontic dental alignment? Results from a randomized pilot study. Photomed Laser Surg 35(8):421–426. https://doi.org/10.1089/pho.2016.4215
Urrútia G, Bonfill X (2010) Declaración PRISMA: una propuesta para mejorar la publicación de revisiones sistemáticas y metaanálisis [PRISMA declaration: a proposal to improve the publication of systematic reviews and meta-analyses]. Med Clin (Barc) 135(11):507–511. https://doi.org/10.1016/j.medcli.2010.01.015
Eid FY, El-Kenany WA, Mowafy MI, El-Kalza AR, Guindi MA (2022) A randomized controlled trial evaluating the effect of two low-level laser irradiation protocols on the rate of canine retraction. Sci Rep 12(1):10074. https://doi.org/10.1038/s41598-022-14280-0
Farhadian N, Miresmaeili A, Borjali M, Salehisaheb H, Farhadian M, Rezaei-Soufi L et al (2021) The effect of intra-oral LED device and low-level laser therapy on orthodontic tooth movement in young adults: a randomized controlled trial. Int Orthod 19(4):612–621. https://doi.org/10.1016/j.ortho.2021.09.002
Türker G, Yavuz İ, Gönen ZB (2021) Which method is more effective for accelerating canine distalization short term, low-level laser therapy or piezocision? A split-mouth study J Orofac Orthop 82(4):236–245. https://doi.org/10.1007/s00056-020-00250-6
AlSayed Hasan MMA, Sultan K, Hamadah O. (2018) Low-level laser therapy effectiveness in accelerating orthodontic tooth movement: a randomized controlled clinical trial [published correction appears in Angle Orthod. 88(1):125]. Angle Orthod. 2017;87(4):499–504. https://doi.org/10.2319/062716-503.1
Zheng J, Yang K (2021) Clinical research: low-level laser therapy in accelerating orthodontic tooth movement. BMC Oral Health 21(1):324. https://doi.org/10.1186/s12903-021-01684-z
Impellizzeri A, Horodynski M, Fusco R, Palaia G, Polimeni A, Romeo U et al (2020) Photobiomodulation therapy on orthodontic movement: analysis of preliminary studies with a new protocol. Int J Environ Res Public Health 17(10):3547. https://doi.org/10.3390/ijerph17103547
Lalnunpuii H, Batra P, Sharma K, Srivastava A, Raghavan S (2020) Comparison of rate of orthodontic tooth movement in adolescent patients undergoing treatment by first bicuspid extraction and en-mass retraction, associated with low level laser therapy in passive self-ligating and conventional brackets: a randomized controlled trial. Int Orthod 18(3):412–423. https://doi.org/10.1016/j.ortho.2020.05.008
Mistry D, Dalci O, Papageorgiou SN, Darendeliler MA, Papadopoulou AK (2020) The effects of a clinically feasible application of low-level laser therapy on the rate of orthodontic tooth movement: a triple-blind, split-mouth, randomized controlled trial. Am J Orthod Dentofacial Orthop 157(4):444–453. https://doi.org/10.1016/j.ajodo.2019.12.005
Arumughan S, Somaiah S, Muddaiah S, Shetty B, Reddy G, Roopa S (2018) A comparison of the rate of retraction with low-level laser therapy and conventional retraction technique. Contemp Clin Dent 9(2):260–266. https://doi.org/10.4103/ccd.ccd_857_17
Guram G, Reddy RK, Dharamsi AM, Syed Ismail PM, Mishra S, Prakashkumar MD (2018) Evaluation of low-level laser therapy on orthodontic tooth movement: a randomized control study. Contemp Clin Dent 9(1):105–109. https://doi.org/10.4103/ccd.ccd_864_17
Kochar GD, Londhe SM, Varghese B, Jayan B, Kohli S, Kohli VS (2017) Effect of low-level laser therapy on orthodontic tooth movement. J Indian Orthod Soc 51(2):81–86. https://doi.org/10.4103/jios.jios_200_16
Qamruddin I, Alam MK, Mahroof V, Fida M, Khamis MF, Husein A (2017) Effects of low-level laser irradiation on the rate of orthodontic tooth movement and associated pain with self-ligating brackets. Am J Orthod Dentofacial Orthop 152(5):622–630. https://doi.org/10.1016/j.ajodo.2017.03.023
Üretürk SE, Saraç M, Fıratlı S, Can ŞB, Güven Y, Fıratlı E (2017) The effect of low-level laser therapy on tooth movement during canine distalization. Lasers Med Sci 32(4):757–764. https://doi.org/10.1007/s10103-017-2159-0
Yassaei S, Aghili H, Afshari JT, Bagherpour A, Eslami F (2016) Effects of diode laser (980 nm) on orthodontic tooth movement and interleukin 6 levels in gingival crevicular fluid in female subjects. Lasers Med Sci 31(9):1751–1759. https://doi.org/10.1007/s10103-016-2045-1
Kansal A, Kittur N, Kumbhojkar V, Keluskar KM, Dahiya P (2014) Effects of low-intensity laser therapy on the rate of orthodontic tooth movement: a clinical trial. Dent Res J (Isfahan) 11(4):481–488
Pereira SCC (2014) Influência do laser de baixa intensidade na movimentação ortodôntica — avaliação clínica e radiográfica [Tese de doutorado]. Bauru: Faculdade de Odontologia de Bauru. https://doi.org/10.11606/T.25.2014.tde-03062015-093530
Souza JMS (2014) Avaliação da influência do laser de baixa intensidade na movimentação ortodôntica e supressão da dor [Tese de doutorado]. Bauru: Faculdade de Odontologia de Bauru. https://doi.org/10.11606/T.25.2014.tde-11042015-102431.
Doshi-Mehta G, Bhad-Patil WA (2012) Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop 141(3):289–297. https://doi.org/10.1016/j.ajodo.2011.09.009
Sousa MV, Scanavini MA, Sannomiya EK, Velasco LG, Angelieri F (2011) Influence of low-level laser on the speed of orthodontic movement. Photomed Laser Surg 29(3):191–196. https://doi.org/10.1089/pho.2009.2652
Cruz DR, Kohara EK, Ribeiro MS, Wetter NU (2004) Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers Surg Med 35(2):117–120. https://doi.org/10.1002/lsm.20076
Domínguez Camacho A, Montoya Guzmán D, Velásquez Cujar SA (2020) Effective wavelength range in photobiomodulation for tooth movement acceleration in orthodontics: a systematic review. Photobiomodul Photomed Laser Surg 38(10):581–590. https://doi.org/10.1089/photob.2020.4814
Yamaguchi M, Hayashi M, Fujita S, Yoshida T, Utsunomiya T, Yamamoto H et al (2010) Low-energy laser irradiation facilitates the velocity of tooth movement and the expressions of matrix metalloproteinase-9, cathepsin K, and alpha(v) beta(3) integrin in rats. Eur J Orthod 32(2):131–139. https://doi.org/10.1093/ejo/cjp078
Domínguez A, Velásquez SA (2021) Acceleration of dental movement by photobiomodulation: how does it happen? Photobiomodul Photomed Laser Surg 39(6):379–380. https://doi.org/10.1089/photob.2020.4969
Saygun I, Karacay S, Serdar M, Ural AU, Sencimen M, Kurtis B (2008) Effects of laser irradiation on the release of basic fibroblast growth factor (bFGF), insulin like growth factor-1 (IGF-1), and receptor of IGF-1 (IGFBP3) from gingival fibroblasts. Lasers Med Sci 23(2):211–215. https://doi.org/10.1007/s10103-007-0477-3
Jose JA, Somaiah S, Muddaiah S, Shetty B, Reddy G, Roopa S (2018) A comparative evaluation of interleukin 1 beta and prostaglandin E2 with and without low-level laser therapy during en masse retraction. Contemp Clin Dent 9(2):267–275. https://doi.org/10.4103/ccd.ccd_859_17
Smith KC (1991) The photobiological basis of low level laser radiation therapy. Laser Ther 3(1):19–24. https://doi.org/10.5978/islsm.91-OR-03
Hadis MA, Zainal SA, Holder MJ, Carroll JD, Cooper PR, Milward MR et al (2016) The dark art of light measurement: accurate radiometry for low-level light therapy. Lasers Med Sci 31(4):789–809. https://doi.org/10.1007/s10103-016-1914-y
Karu TI (2010) Multiple roles of cytochrome c oxidase in mammalian cells under action of red and IR-A radiation. IUBMB Life 62(8):607–610. https://doi.org/10.1002/iub.359
Dominguez A, Castro P, Morales M (2009) An in vitro study of the reaction of osteoblasts to low-level laser irradiation. J Oral Laser Appl 9(1):21–28
Olmedo-Hernández OL, Mota-Rodríguez AN, Torres-Rosas R, Argueta-Figueroa L (2022) Effect of the photobiomodulation for acceleration of the orthodontic tooth movement: a systematic review and meta-analysis. Lasers Med Sci 37(5):2323–2341
Li J, Ge X, Guan H, Jia L, Chang W, Ma W (2021) The effectiveness of photobiomodulation on accelerating tooth movement in orthodontics: a systematic review and meta-analysis. Photobiomodul Photomed Laser Surg 39(4):232–244. https://doi.org/10.1089/photob.2020.4954
Ge MK, He WL, Chen J, Wen C, Yin X, Hu ZA, Liu ZP, Zou SJ (2015) Efficacy of low-level laser therapy for accelerating tooth movement during orthodontic treatment: a systematic review and meta-analysis. Lasers Med Sci 30(5):1609–1618
Ruan MJ, Chen G, Xu TM (2018) Comparison of orthodontic tooth movement between adolescents and adults based on implant superimposition. PLoS One. 13(5):e0197281. https://doi.org/10.1371/journal.pone.0197281
Iwasaki LR, Liu Y, Liu H, Nickel JC (2017) Speed of human tooth movement in growers and non-growers: selection of applied stress matters. Orthod Craniofac Res 20(Suppl 1):63–67. https://doi.org/10.1111/ocr.12161
Khalid Z, Bangash AA, Anwar A, Pasha H, Amin E (2018) Canine retraction using a closed nickel titanium coil spring and an elastic module. J Coll Physicians Surg Pak 28(9):695–698. https://doi.org/10.29271/jcpsp.2018.09.695
Author information
Authors and Affiliations
Contributions
Conceptualisation: MG. Methodology: NR and OJ. Search strategy and article selection: MG and KS. Data extraction: MG and JM. Qualitative synthesis: OJ. Quantitative synthesis: HA. Risk of bias assessment: OJ. Formal analysis: MG, NR, and HA. Writing: NR, JM, and MG. Supervision of the manuscript: NR and MG.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have given their approval for publication and agree to be accountable for all aspects of the work.
Competing interests
The authors declare no competing interests.
Disclaimer
In consideration of the Editors of the Progress in Orthodontics Journal, taking action in reviewing and editing this submission, the authors undersigned hereby transfer, assign, or otherwise convey all copyright ownership, in the event that such work is published in that Journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Grajales, M., Ríos-Osorio, N., Jimenez-Peña, O. et al. Effectiveness of photobiomodulation with low-level lasers on the acceleration of orthodontic tooth movement: a systematic review and meta-analysis of split-mouth randomised clinical trials. Lasers Med Sci 38, 200 (2023). https://doi.org/10.1007/s10103-023-03870-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03870-7