Abstract
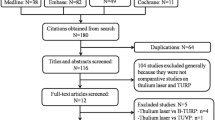
We conducted a meta-analysis to evaluate the efficacy and safety of photo selective vaporisation of the prostate (PVP) with the GreenLight Laser versus transurethral resection of the prostate (TURP) for the treatment of small-volume benign prostatic hyperplasia (BPH). As of July 2022, relevant literature in online databases such as Cochrane Library, PubMed, and Embase was searched, including studies published on or before that date, and there were 9 studies in total, including 5 RCTs and 4 non-RCTs. In total 1525 patients were included to compare the efficacy of PVP and TURP in treating BPH. The Cochrane Collaboration criteria were used to evaluate the risk of bias. The software was used for random effect meta-analysis with RevMan 5.3. Data extraction included: clinical baseline characteristics, perioperative parameters, complication rates, International Prostate Symptom Score (IPSS), prostate specific antigen (PSA), post-void residual urine (PVR), maximum flow rate (Qmax), and quality of life (QoL). The pooled analysis showed that PVP was associated with reduced blood loss, blood transfusion, clot retention, catheterization time, definitive catheter removal, and hospital stay, but was associated with longer operative time and more severe dysuria (all p < 0.05). The results of this meta-analysis show that PVP as a technique for the treatment of benign prostatic hyperplasia with a volume of less than 80 cc has similar efficacy to standard TURP in IPSS, PSA, PVR, Qmax and QoL, and is an effective alternative. It outperformed TURP in terms of blood transfusion, catheterization time and hospital stay, while TURP is superior to PVP in terms of operation time.





Similar content being viewed by others
Data Availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- PVP:
-
Photoselective vaporisation of the prostate
- TURP:
-
Transurethral resection of the prostate
- BPH:
-
Benign prostatic hyperplasia
- RCT:
-
Randomized controlled trials
- IPSS:
-
International Prostate Symptom Score
- PSA:
-
Prostate specific antigen
- PVR:
-
Post-void residual urine
- Qmax:
-
Maximum flow rate
- QoL:
-
Quality of life
- LUTSs:
-
Lower urinary tract symptoms
- TURS:
-
Transurethral resection syndrome
- Rezum:
-
Water vapour thermal therapy
- PAE:
-
Prostate artery embolisation
- UroLift:
-
Prostatic urethral lift
- i-TIND:
-
Temporary implantable nitinol device
- UTI:
-
Urinary tract infection
- HoLEP:
-
Holmium laser enucleation of the prostate;
- Tm:YAG:
-
Thulium: yttrium–aluminum-garnet
- TFL:
-
Thulium fiber laser
- HPS:
-
High Performance System
- BMI:
-
Body Mass Index
References
Hirayama A et al (2002) Comparison of parameters to determine the cause of urinary disturbance in men with prostate volume less than 20 milliliters. Int J Urol 9(10):554–9 (discussion 560)
Irwin DE et al (2006) Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 50(6):1306–14 (discussion 1314-5)
Tao W et al (2017) The efficacy and safety of 2-μm continuous laser in the treatment of high-risk patients with benign prostatic hyperplasia. Lasers Med Sci 32(2):351–356
Lerner LB et al (2021) Management of lower urinary tract symptoms attributed to Benign Prostatic Hyperplasia: AUA GUIDELINE PART I-Initial Work-up and Medical Management. J Urol 206(4):806–817
Michel MC et al (1998) Tamsulosin treatment of 19,365 patients with lower urinary tract symptoms: does co-morbidity alter tolerability? J Urol 160(3 Pt 1):784–791
Pirozzi L et al (2015) Current pharmacological treatment for male LUTS due to BPH: Dutasteride or finasteride? Curr Drug Targets 16(11):1165–1171
Roehrborn CG (2008) BPH progression: concept and key learning from MTOPS, ALTESS, COMBAT, and ALF-ONE. BJU Int 101(Suppl 3):17–21
Cantiello F et al (2021) Mechanical and ablative minimally invasive techniques for male LUTS due to Benign prostatic obstruction: A systematic review according to BPH-6 evaluation. Urol Int 105(9–10):858–868
Thomas D et al (2017) Emerging drugs for the treatment of benign prostatic hyperplasia. Expert Opin Emerg Drugs 22(3):201–212
Lokeshwar SD et al (2019) Epidemiology and treatment modalities for the management of benign prostatic hyperplasia. Transl Androl Urol 8(5):529–539
Hueber PA, Al-Asker A, Zorn KC (2011) Monopolar vs. bipolar TURP: assessing their clinical advantages. Can Urol Assoc J 5(6):390–1
Méndez-Probst CE et al (2011) A multicentre single-blind randomized controlled trial comparing bipolar and monopolar transurethral resection of the prostate. Can Urol Assoc J 5(6):385–389
Reich O et al (2008) Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol 180(1):246–249
Rassweiler J et al (2006) Complications of transurethral resection of the prostate (TURP)–incidence, management, and prevention. Eur Urol 50(5):969–79 (discussion 980)
Madersbacher S, Roehrborn CG, Oelke M (2020) The role of novel minimally invasive treatments for lower urinary tract symptoms associated with benign prostatic hyperplasia. BJU Int 126(3):317–326
Rieken M, Herrmann TRW, Füllhase C (2019) Surgical treatment of benign prostatic hyperplasia-resection, vaporization or enucleation? Urologe A 58(3):263–270
Oelke M et al (2013) EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 64(1):118–140
Meng QQ et al (2019) Tranexamic acid is beneficial for reducing perioperative blood loss in transurethral resection of the prostate. Exp Ther Med 17(1):943–947
Kuntzman RS et al (1996) Potassium-titanyl-phosphate laser vaporization of the prostate: a comparative functional and pathologic study in canines. Urology 48(4):575–583
Kuntzman RS et al (1997) High-power (60-watt) potassium-titanyl-phosphate laser vaporization prostatectomy in living canines and in human and canine cadavers. Urology 49(5):703–708
Lee R, Gonzalez RR, Te AE (2006) The evolution of photoselective vaporization prostatectomy (PVP): advancing the surgical treatment of benign prostatic hyperplasia. World J Urol 24(4):405–409
Malek RS, Kuntzman RS, Barrett DM (2005) Photoselective potassium-titanyl-phosphate laser vaporization of the benign obstructive prostate: observations on long-term outcomes. J Urol 174(4 Pt 1):1344–1348
Ghobrial FK et al (2020) A randomized trial comparing bipolar transurethral vaporization of the prostate with GreenLight laser (xps-180watt) photoselective vaporization of the prostate for treatment of small to moderate benign prostatic obstruction: outcomes after 2 years. BJU Int 125(1):144–152
Guo S et al (2015) The 80-W KTP GreenLight laser vaporization of the prostate versus transurethral resection of the prostate (TURP): adjusted analysis of 5-year results of a prospective non-randomized bi-center study. Lasers Med Sci 30(3):1147–1151
Kumar N et al (2016) Prospective randomized comparison of monopolar TURP, Bipolar TURP and Photoselective vaporization of the prostate in patients with benign prostatic obstruction: 36 months outcome. Low Urin Tract Symptoms 10(1):17–20
Mattevi D et al (2020) Comparison of GreenLight 180-W XPS laser vaporization versus transurethral resection of the prostate: Outcomes of a single regional center. Arch Ital Urol Androl 92(3). https://doi.org/10.4081/aiua.2020.3.169
Mordasini L et al (2018) 80-W greenlight laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic obstruction: 5-year outcomes of a single-center prospective randomized trial. Urology 116:144–149
Pereira-Correia JA et al (2012) GreenLight HPS™ 120-W laser vaporization vs transurethral resection of the prostate (<60 mL): a 2-year randomized double-blind prospective urodynamic investigation. BJU Int 110(8):1184–1189
Reimann M et al (2020) Outcome of photoselective vaporization of the prostate with the GreenLight-XPS 180 watt system compared to transurethral resection of the prostate. J Clin Med 8(7):1004.
Telli O et al (2015) A prospective, randomized comparative study of monopolar transurethral resection of the prostate versus photoselective vaporization of the prostate with GreenLight 120-W laser, in prostates less than 80 cc. Ther Adv Urol 7(1):3–8
Thomas JA et al (2015) A multicenter randomized noninferiority trial comparing GreenLight-XPS laser vaporization of the prostate and transurethral resection of the prostate for the treatment of Benign prostatic obstruction: two-yr outcomes of the GOLIATH study. Eur Urol 69(1):94–102
Tugcu V et al (2008) Comparison of photoselective vaporization of the prostate and transurethral resection of the prostate: a prospective nonrandomized bicenter trial with 2-year follow-up. J Endourol 22(7):1519–1525
Ene C, Geavlete P, Geavlete B (2020) What’s New in Bipolar TURP for Surgical Management of BPH? Chirurgia (Bucur) 115(3):307–313
Michalak J, Tzou D, Funk J (2015) HoLEP: the gold standard for the surgical management of BPH in the 21(st) century. Am J Clin Exp Urol 3(1):36–42
Fried NM, Murray KE (2005) High-power thulium fiber laser ablation of urinary tissues at 1.94 microm. J Endourol 19(1):25–31
Zhu Y et al (2015) Thulium laser versus standard transurethral resection of the prostate for benign prostatic obstruction: a systematic review and meta-analysis. World J Urol 33(4):509–515
Bozzini G et al (2023) Thulium: YAG vs continuous-wave thulium fiber laser enucleation of the prostate: do potential advantages of thulium fiber lasers translate into relevant clinical differences? World J Urol 41(1):143–150
Xue B et al (2013) GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a prospective randomized trial. J Xray Sci Technol 21(1):125–132
Bachmann A et al (2005) Photoselective vaporization (PVP) versus transurethral resection of the prostate (TURP): a prospective bi-centre study of perioperative morbidity and early functional outcome. Eur Urol 48(6):965–71 (discussion 972)
Castellani D et al (2021) GreenLight Laser™ Photovaporization versus transurethral resection of the prostate: a systematic review and meta-analysis. Res Rep Urol 13:263–271
Tao W et al (2019) Application of 180W XPS GreenLight laser vaporization of the prostate for treatment of benign prostatic hyperplasia. J Xray Sci Technol 27(6):1121–1129
Zhou Y et al (2016) Greenlight high-performance system (HPS) 120-W laser vaporization versus transurethral resection of the prostate for the treatment of benign prostatic hyperplasia: a meta-analysis of the published results of randomized controlled trials. Lasers Med Sci 31(3):485–495
Yang TK et al (2015) Body mass index and age are predictors for symptom improvement after high-power laser vaporization for benign prostatic hyperplasia. J Formos Med Assoc 114(3):268–273
Anderson BB, Pariser JJ, Helfand BT (2015) Comparison of patients undergoing PVP Versus TURP for LUTS/BPH. Curr Urol Rep 16(8):55
Meeks JJ et al (2013) Clinically significant prostate cancer is rarely missed by ablative procedures of the prostate in men with prostate specific antigen less than 4 ng/ml. J Urol 189(1):111–115
Tao W et al (2019) Comparison of vaporization using 120-W GreenLight laser versus 2-micrometer continuous laser for treating benign prostatic hyperplasia: A 24-month follow-up study of a single center. J Xray Sci Technol 27(4):755–764
Te AE (2006) The next generation in laser treatments and the role of the greenlight high-performance system laser. Rev Urol 8 Suppl 3(Suppl 3):S24-30
Rieken M, Kaplan SA (2018) Enucleation, vaporization, and resection: how to choose the best surgical treatment option for a patient with male lower urinary tract symptoms. Eur Urol Focus 4(1):8–10
Wroclawski ML et al (2021) Shedding light on polypragmasy of pain after transurethral prostate surgery procedures: a systematic review and meta-analysis. World J Urol 39(10):3711–3720
Al-Ansari A et al (2010) GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up. Eur Urol 58(3):349–355
Funding
This work was supported by grants from the National Nature Science Foundation of China (No.81870525), Taishan Scholars Program of Shandong Province (No. tsqn201909199).
Author information
Authors and Affiliations
Contributions
Conceptualization: Zhongbao Zhou. Data curation: Shangjing Liu, Hongquan Liu. Formal analysis: Shangjing Liu, Huibao Yao, Fengze Sun. Funding acquisition: Jitao Wu. Investigation: Shangjing Liu, Huibao Yao, Fengze Sun. Methodology: Shangjing Liu, Hongquan Liu, Fengze Sun. Project administration: Zhongbao Zhou. Resources: Shangjing Liu, Hongquan Liu, Huibao Yao. Software: Shangjing Liu, Hongquan Liu. Supervision: Fengze Sun, Jitao Wu. Writing – original draft: Shangjing Liu, Hongquan Liu, Huibao Yao. Writing – review & editing: Zhongbao Zhou, Jitao Wu.
Corresponding authors
Ethics declarations
Ethics approval
No ethics to disclose.
Disclosures
All authors had no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shangjing Liu, Hongquan Liu, Huibao Yao: co-first author.
Supplementary Information
Below is the link to the electronic supplementary material.
10103_2023_3794_MOESM1_ESM.pdf
Supplementary file1 (PDF 506 KB) Supplemental Figure 1. Forest plots show the improvement of PVP and TURP on various data at 12-month follow-up after treatment. (a) IPSS; (b) PSA; (c) PVR; (d) Qmax; (e) Qol. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom
10103_2023_3794_MOESM2_ESM.pdf
Supplementary file2 (PDF 413 KB) Supplemental Figure 2. Forest plots show the improvement of PVP and TURP on various data at 24-month follow-up after treatment. (a) IPSS; (b) PVR; (c) Qmax; (d) Qol. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom
10103_2023_3794_MOESM3_ESM.pdf
Supplementary file3 (PDF 287 KB) Supplemental Figure 3. Forest plots show the improvement of PVP and TURP on various data at 60-month follow-up after treatment. (a) IPSS; (b) PVR; (c) Qmax; (d) Qol. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom
10103_2023_3794_MOESM4_ESM.pdf
Supplementary file4 (PDF 439 KB) Supplemental Figure 4. Forest plots showing various Postoperative Complications. (a) Bladder neck contracture; (b) Urethral stricture; (c) Urinary tract infection; (d) Urethral retention; (e) Reoperation rate. M-H, Mantel-Haenszel; CI, confidence interval; df, degrees of freedom
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, S., Liu, H., Yao, H. et al. A systematic review and meta-analysis of efficacy and safety comparing greenlight laser vaporization with transurethral resection of the prostate for benign prostatic hyperplasia with prostate volume less than 80 ml. Lasers Med Sci 38, 133 (2023). https://doi.org/10.1007/s10103-023-03794-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03794-2